
- My presentations

Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video
Hypertension Case Study
Published by Priscila Fretwell Modified over 9 years ago
Similar presentations
Presentation on theme: "Hypertension Case Study"— Presentation transcript:
Hypertension Medications By: Elizabeth Rangel University of the Incarnate Word.
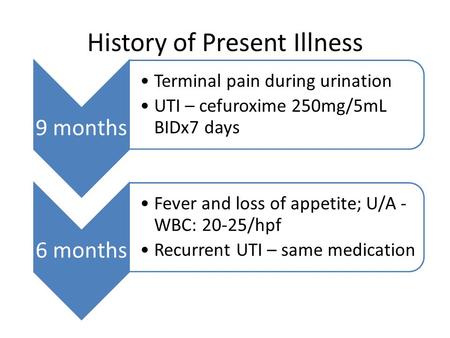
History of Present Illness 9 months Terminal pain during urination UTI – cefuroxime 250mg/5mL BIDx7 days 6 months Fever and loss of appetite; U/A - WBC:
Clinical Case Presentation
Block 9 Board Review Endocrine/Rheum 14Feb14 Chauncey D. Tarrant, M.D. Chief of Residents
Atypical Polymyalgia Rheumatica
Prepared by: Tristan Villanueva Arcibal BSN-RN Presented on: July 16, 2013 A CASE PRESENTATION OF A PATIENT WITH DIABETIC KETOACIDOCIS (DKA)
© 2007 Thomson - Wadsworth Chapter 13 Nutrition Care and Assessment.
GOING TO THE DOCTOR Prof. Teresita Rojas González.

Linking Medicine with Dental Professional Internal Medicine for Dentists.
History and Physical Examination Mike Clark, M.D..

Nursing Health Assessments
1 Clinical Case Presentation Building Blocks of Life Case # 6 Diabetes Mellitus Type 1 Building Blocks of Life Case # 6 Diabetes Mellitus Type 1.
Periodic Health Evaluations Components, Procedures, and Why They Could Save Your Life!!!
Example Conference EBM format
Case Study 37 By Chris Sanders.
The History and Physical Exam. The History Welcome the patient - ensure comfort and privacy Know and use the patient's name - introduce and identify yourself.

PROGRESS NOTE (SOAP Notes)
Central Sleep Apnea Problem Based Learning Module Vidya Krishnan, and Sutapa Mukherjee for the Sleep Education for Pulmonary Fellows and Practitioners,
Prescreening ä To optimize safety ä To permit the development of a sound and effective exercise prescription.
How to write your medical documents? Jun Xu, M.D., L. Ac.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.

- Previous Article
- Next Article
Presentation
Clinical pearls, case study: treating hypertension in patients with diabetes.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Evan M. Benjamin; Case Study: Treating Hypertension in Patients With Diabetes. Clin Diabetes 1 July 2004; 22 (3): 137–138. https://doi.org/10.2337/diaclin.22.3.137
Download citation file:
- Ris (Zotero)
- Reference Manager
L.N. is a 49-year-old white woman with a history of type 2 diabetes,obesity, hypertension, and migraine headaches. The patient was diagnosed with type 2 diabetes 9 years ago when she presented with mild polyuria and polydipsia. L.N. is 5′4″ and has always been on the large side,with her weight fluctuating between 165 and 185 lb.
Initial treatment for her diabetes consisted of an oral sulfonylurea with the rapid addition of metformin. Her diabetes has been under fair control with a most recent hemoglobin A 1c of 7.4%.
Hypertension was diagnosed 5 years ago when blood pressure (BP) measured in the office was noted to be consistently elevated in the range of 160/90 mmHg on three occasions. L.N. was initially treated with lisinopril, starting at 10 mg daily and increasing to 20 mg daily, yet her BP control has fluctuated.
One year ago, microalbuminuria was detected on an annual urine screen, with 1,943 mg/dl of microalbumin identified on a spot urine sample. L.N. comes into the office today for her usual follow-up visit for diabetes. Physical examination reveals an obese woman with a BP of 154/86 mmHg and a pulse of 78 bpm.
What are the effects of controlling BP in people with diabetes?
What is the target BP for patients with diabetes and hypertension?
Which antihypertensive agents are recommended for patients with diabetes?
Diabetes mellitus is a major risk factor for cardiovascular disease (CVD). Approximately two-thirds of people with diabetes die from complications of CVD. Nearly half of middle-aged people with diabetes have evidence of coronary artery disease (CAD), compared with only one-fourth of people without diabetes in similar populations.
Patients with diabetes are prone to a number of cardiovascular risk factors beyond hyperglycemia. These risk factors, including hypertension,dyslipidemia, and a sedentary lifestyle, are particularly prevalent among patients with diabetes. To reduce the mortality and morbidity from CVD among patients with diabetes, aggressive treatment of glycemic control as well as other cardiovascular risk factors must be initiated.
Studies that have compared antihypertensive treatment in patients with diabetes versus placebo have shown reduced cardiovascular events. The United Kingdom Prospective Diabetes Study (UKPDS), which followed patients with diabetes for an average of 8.5 years, found that patients with tight BP control (< 150/< 85 mmHg) versus less tight control (< 180/< 105 mmHg) had lower rates of myocardial infarction (MI), stroke, and peripheral vascular events. In the UKPDS, each 10-mmHg decrease in mean systolic BP was associated with a 12% reduction in risk for any complication related to diabetes, a 15% reduction for death related to diabetes, and an 11% reduction for MI. Another trial followed patients for 2 years and compared calcium-channel blockers and angiotensin-converting enzyme (ACE) inhibitors,with or without hydrochlorothiazide against placebo and found a significant reduction in acute MI, congestive heart failure, and sudden cardiac death in the intervention group compared to placebo.
The Hypertension Optimal Treatment (HOT) trial has shown that patients assigned to lower BP targets have improved outcomes. In the HOT trial,patients who achieved a diastolic BP of < 80 mmHg benefited the most in terms of reduction of cardiovascular events. Other epidemiological studies have shown that BPs > 120/70 mmHg are associated with increased cardiovascular morbidity and mortality in people with diabetes. The American Diabetes Association has recommended a target BP goal of < 130/80 mmHg. Studies have shown that there is no lower threshold value for BP and that the risk of morbidity and mortality will continue to decrease well into the normal range.
Many classes of drugs have been used in numerous trials to treat patients with hypertension. All classes of drugs have been shown to be superior to placebo in terms of reducing morbidity and mortality. Often, numerous agents(three or more) are needed to achieve specific target levels of BP. Use of almost any drug therapy to reduce hypertension in patients with diabetes has been shown to be effective in decreasing cardiovascular risk. Keeping in mind that numerous agents are often required to achieve the target level of BP control, recommending specific agents becomes a not-so-simple task. The literature continues to evolve, and individual patient conditions and preferences also must come into play.
While lowering BP by any means will help to reduce cardiovascular morbidity, there is evidence that may help guide the selection of an antihypertensive regimen. The UKPDS showed no significant differences in outcomes for treatment for hypertension using an ACE inhibitor or aβ-blocker. In addition, both ACE inhibitors and angiotensin II receptor blockers (ARBs) have been shown to slow the development and progression of diabetic nephropathy. In the Heart Outcomes Prevention Evaluation (HOPE)trial, ACE inhibitors were found to have a favorable effect in reducing cardiovascular morbidity and mortality, whereas recent trials have shown a renal protective benefit from both ACE inhibitors and ARBs. ACE inhibitors andβ-blockers seem to be better than dihydropyridine calcium-channel blockers to reduce MI and heart failure. However, trials using dihydropyridine calcium-channel blockers in combination with ACE inhibitors andβ-blockers do not appear to show any increased morbidity or mortality in CVD, as has been implicated in the past for dihydropyridine calcium-channel blockers alone. Recently, the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) in high-risk hypertensive patients,including those with diabetes, demonstrated that chlorthalidone, a thiazide-type diuretic, was superior to an ACE inhibitor, lisinopril, in preventing one or more forms of CVD.
L.N. is a typical patient with obesity, diabetes, and hypertension. Her BP control can be improved. To achieve the target BP goal of < 130/80 mmHg, it may be necessary to maximize the dose of the ACE inhibitor and to add a second and perhaps even a third agent.
Diuretics have been shown to have synergistic effects with ACE inhibitors,and one could be added. Because L.N. has migraine headaches as well as diabetic nephropathy, it may be necessary to individualize her treatment. Adding a β-blocker to the ACE inhibitor will certainly help lower her BP and is associated with good evidence to reduce cardiovascular morbidity. Theβ-blocker may also help to reduce the burden caused by her migraine headaches. Because of the presence of microalbuminuria, the combination of ARBs and ACE inhibitors could also be considered to help reduce BP as well as retard the progression of diabetic nephropathy. Overall, more aggressive treatment to control L.N.'s hypertension will be necessary. Information obtained from recent trials and emerging new pharmacological agents now make it easier to achieve BP control targets.
Hypertension is a risk factor for cardiovascular complications of diabetes.
Clinical trials demonstrate that drug therapy versus placebo will reduce cardiovascular events when treating patients with hypertension and diabetes.
A target BP goal of < 130/80 mmHg is recommended.
Pharmacological therapy needs to be individualized to fit patients'needs.
ACE inhibitors, ARBs, diuretics, and β-blockers have all been documented to be effective pharmacological treatment.
Combinations of drugs are often necessary to achieve target levels of BP control.
ACE inhibitors and ARBs are agents best suited to retard progression of nephropathy.
Evan M. Benjamin, MD, FACP, is an assistant professor of medicine and Vice President of Healthcare Quality at Baystate Medical Center in Springfield, Mass.
Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Res Notes

A teenager with uncontrolled hypertension: a case report
Abdul wadud chowdhury.
1 Department of Cardiology, Dhaka Medical College Hospital, Dhaka, Bangladesh
ATM Hasibul Hasan
2 Department of Medicine (Outdoor Patient Department), Dhaka Medical College Hospital, Dhaka, Bangladesh
SME Jahan Kabir
Km nurus sabah.
Takayasu Arteritis is a vasculitis occurring mostly in young females which may present in diverse ways. Here we report a teenager with Takayasu Arteritis who presented with uncontrolled hypertension. This case depicts an atypical presentation of this disease where the girl visited many physicians for controlling the level of hypertension and put a diagnostic dilemma about the underlying etiology of young hypertension.
Case presentation
A 13 year old girl presented with epistaxis, persistent headache and uncontrolled hypertension. Her clinical examination revealed normal radial, very feeble femoral and absent other lower limb pulses. There was a blood pressure discrepancy of 50/40 mm of Hg between two arms. There were bruits over multiple areas including the abdominal aorta. She had features of left ventricular hypertrophy. Her Arch aortogram showed hugely dilated arch of aorta which became abruptly normal just after origin of left subclavian artery. There was ostio-proximal stenosis of right bracheocephalic artery, left common carotid and left subclavian artery with post stenotic dilatation of all the vessels. Abdominal aortogram revealed critical stenosis of abdominal aorta above the origin of renal arteries with a pressure gradient of 80/11 mm of Hg.
Takayasu’s Arteritis should also be kept in mind while searching for the cause of uncontrolled hypertension in the young age group.
The estimated prevalence of hypertension in pediatric age group is between 2%–5% [ 1 ]. The usual form of hypertension in young is attributable to secondary causes. The most common cause is the renovascular one (60–70%) [ 2 , 3 ]. Cushing syndrome, hyperthyroidism, pheochromocytoma, essential hypertension, coarctation of aorta, SLE are also found less commonly with hypertension in children and adeloscent [ 4 ]. With the growing knowledge and awareness of hypertension, the rate of diagnosis is increasing in children [ 1 ]. Evidences are increasing regarding early development of atherosclerosis in child and their possible relation to hypertension and coronary artery disease [ 5 ]. Several studies have reported the correlation between pediatric hypertension and family H/O hypertension, low birth weight, excess body weight [ 6 , 7 ]. Here we describe a 13 year old girl presenting with epistaxis, headache and uncontrolled hypertension despite poly drug therapy, abnormal peripheral pulses and unequal blood pressure in upper limbs. Further investigations were done to determine the cause of hypertension. The arch and abdominal aortography further correlated the uncontrolled hypertension with Takayasu’s disease according to American College Rheumatology (ACR) criteria. KS Chugh et al. described Takayasu Arteritis as the most common cause of renovascular hypertension in India [ 8 ]. Takayasu Arteritis is a large vessel vasculitis of unknown origin characterized by granulomatous inflammation of aorta and its major branches, leading to stenosis, thrombosis and aneurysm formation.
A 13 year old girl presented with three episodes of spontaneous profuse nasal bleeding within last three years which had remission without specific therapy. She had diffuse persistent headache without nausea or vomiting and uncontrolled hypertension, despite taking amlodipine and atenolol. She gave no H/O chest pain, shortness of breath, fever, prolonged cough, pulsatile tinnitus, light headedness, arthralgia, skin rash, weight loss, claudication or colour changes on cold exposure. There was no history of contact with TB patient. She did not give any H/O dizziness or syncope. On examination, both radial pulses were 80 beats/min, regular, high volume and surprisingly apparently symmetrical on both sides. There was no radio-femoral delay. Both the femoral pulses were feeble. All other lower limb pulses were absent. BP on right arm was 120/80 mmHg and on left arm was 170/120mmHg. There were bruits over both carotids, suprasternal, supraclavicular areas and over abdominal aorta. On precordial examination-apex beat was palpable at left 5th intercostal space just lateral to the midclavicular line. It was heaving in nature. A 2 was loud, there was no added sound. All other systemic examinations including optic fundi were normal. On investigation, Hemoglobin was 11.2 gm/dl, Total Count-5100/mm [ 3 ], Neutrophil- 51%, Lymphocyte- 35%, Monocyte- 03%, Eosinophil-07%, Erythrocyte sedimentation rate (ESR)- 30 mm in 1st hour. Mantoux test (MT) and C-reactive protein (CRP) were negative. Blood glucose, Serum creatinine, urine analysis were normal. Chest X-ray showed cardiomegaly with LV type apex (Figure (Figure1 1 A).

A: CXR P-A view. Cardiomegaly with LV type apex. B ECG. Left ventricular hypertrophy.
ECG fulfilled the voltage criteria of left ventricular hypertrophy (Figure (Figure1B). 1 B). 2D, M-mode and Doppler echocardiography revealed concentric left ventricular hypertrophy, aneurysmal dilatation of aortic arch, proximal stenosis and post stenotic dilatation of brachiocephalic, left common carotid and left subclavian artery and narrowing of descending thoracic aorta beyond the origin of left subclavian artery. Arch Aortogram showed hugely dilated (70 mm) arch of aorta which became abruptly normal (35 mm) just after origin of left subclavian artery. Right bracheocephalic artery had ostio-proximal stenosis with marked post stenotic dilatation (Figure (Figure2A: 2 A: white arrow). There was also ostio-proximal stenosis of left common carotid and left subclavian artery with post stenotic dilatation (Figure (Figure2B: 2 B: white arrow). Abdominal aortogram revealed critical stenosis of abdominal aorta (8.9 mm) above the origin of renal arteries (Figure (Figure2C: 2 C: white arrow). Renal arteries were however normal. Pressure study in abdominal aorta showed a pressure tracing of 200/106 mm of Hg above and 120/95 mm of Hg below the stenosis (Figure (Figure3 3 ).

A: Arch Aortogram. Hugely dilated (70 mm) arch of aorta which became abruptly normal (35 mm) just after origin of left subclavian artery. Right bracheocephalic artery had ostio-proximal stenosis with marked post stenotic dilatation (white arrow). B : Arch Aortogram. Ostio-proximal stenosis of left common carotid and left subclavian artery with post stenotic dilatation (white arrow). C : Abdominal Aortogram critical stenosis of abdominal aorta (8.9 mm) above the origin of renal arteries (white arrow).

Pressure tracing in abdominal aorta.
She fulfilled four of the six major ACR (American College of Rheumatology) criteria for Takayasu’s disease eg, onset of age is 13 years (<40years), 50 mm of Hg pressure difference between systolic BP between arms (>10mm of Hg pressure difference), subclavian and aortic bruit and narrowing of major branches of aorta. She was prescribed Amlodipine 10 mg, Atenolol 100mg, Prazosin 6mg, Hydrochlorthiazide 50mg and Amiloride 5mg. Methotrexate 5mg weekly with Folinic acid supplementation were given too. Plan for Angioplasty and Stenting of abdominal aortic stenosis was provided to the patient.
Takayasu’s Arteritis (TA) is a chronic inflammatory large vessel vasculitis of unknown origin, predominantly affecting aorta and its major branches. It is also called Aortic arch syndrome, Pulse less disease, Occlusive thromboaortopathy, Martorell syndrome [ 9 ]. The first scientific description of Takayasu’s Arteritis was given by Mikito Takaysu, Professor of Opthalmology at Kanazawa University, Japan, in 1905 at 12th Annual conference of Japanese Ophthalmology Society [ 10 ]. He presented a 21year old woman with a peculiar form of arteriovenus anastomoses at optic fundi. K Onishi and T Kagosha also contributed with their patients of absent radial pulse in the same conference [ 10 ]. But the first ever documented description of this arteritis dates back to 1830. Rokushu Yamamoto who practiced Japanese oriental medicine, described a case of 45 years old man presenting with absent pulse in one upper limb and feeble pulse in another one following a year long history of high grade fever. During the period of follow up the patient subsequently became emaciated, dyspnoeic and died suddenly after 11 years [ 10 ]. The world wide prevalence of Takayasu’s disease is 3.3/million. The disease is more common in East Asia and in Asian descendants in other countries [ 11 ]. TA commonly presents in 2nd or 3rd decade of life, with a high female preponderance. But the female to male ratio declines from Eastern Asia to the West [ 12 ]. TA may manifest as asymptomatic pulseless disease to catastrophic neurological impairements. The disease may present in two phase, a prepulseless phase of nonspecific inflammatory signs, followed by a chronic phase of vascular insufficiency [ 13 - 15 ]. Presentation of TA varies among the races. Japanese patients are predominantly female, presents with pulslessness, dizziness, vertigo, aortic regurgitation, inflammatory process commonly affecting the arch and its major branches, whereas Indian patients are male dominant. Indian cases present with more hypertension, headache, LV hypertrophy and vasculitic involvement of abdominal aorta and renal arteries [ 15 ]. Diminished or absent pulse along with upper limb claudication and blood pressure difference is found in 84–96% of cases [ 16 ]. Vascular bruits involving carotid, subclavian and abdominal vessels are also common (80–94%) [ 17 ]. Hypertension is associated with 33–83% patients of TA [ 15 , 17 ]. Our index case was also a young girl with feeble femoral pulse and absent other peripheral pulses in lower limb, blood pressure discrepancy between arms, bruits over multiple areas of chest and neck and hypertension. The blood pressure discrepancy of 50/40 mm of Hg is probably due to the difference in percentage of stenosis among the brachiocephalic (70–80% stenosis) and left subclavian vessels (50–60% stenosis). Retinopathy, aortic regurgitation, congestive heart failure, cardiomyopathy, myocardial ischemia, headache, dizziness, seizure are less common association of TA. From common findings of TA, American College of Rheumatology has devised some diagnostic criteria for TA in 1990. Angiography remains the gold standard investigation for diagnosis. The main differential diagnosis include other causes of large vessel vasculitis eg inflammatory vasculitis (Syphilis, Tuberculosis, Behchets, SLE); development abnormalities (Coarctation of aorta, Marfans syndrome) and neurofibromatosis. TA has been classified on the basis of angiographic findings. The new classification was described at Takayasu Arteritis Conference in 1994 based on vessel involvement. Type-I involving branches from aortic arch, Type-IIa denoting ascending aorta, aortic arch and its branches, Type-IIb including Type-Ia plus descending thoracic aorta. Type-III means descending thoracic aorta, abdominal aorta and/ or renal arteries. Type-IV involves abdominal aorta and/ or renal arteries. Type-V is combined features of Type-IIb and Type-IV [ 15 ]. Ishikawa classified different clinical groups based on natural history and complications. He described Group-I as uncomplicated disease with or without pulmonary artery involvement, Group-IIA as mild/moderate single complication together with uncomplicated disease, Group-IIB as severe single complication together with uncomplicated disease, Group-III as two or more complications together with uncomplicated disease [ 17 ]. Ishikawa defined Takayasu retinopathy, Secondary hypertension, Aortic regurgitation, Aneurysm formation as four most important complications. Our index case met the angiographic criteria of Type-IV Takayasu Arteritis class and Group-III of Ishikawa class [ 17 ]. Ishikawa class caries a prognostic significance not only for the Japanese patients but also for the Indians. The overall five year survival rate is 83%. The survival rate is 100% in Group-I and 70% in Group-IIb and Group-III. The most common cause of mortality is cerebrovascular disease and cardiac failure. Regarding treatment strategy steroid had been the mainstay of treatment. Shelhamer et al. showed half of the TA patients on steroid won’t respond [ 18 ]. Kerr et al. showed overall remission rate of 33% with immunosuppressive drugs in steroid unresponsive patients [ 16 ]. Methotrexate though not more efficacious than others, became popular due to its well tolerability [ 19 , 20 ]. The combination of steroid and methotrexate demonstrated a remission rate of 81% in steroid unresponsive patients [ 21 ]. Treatment of hypertension and prevention of thrombosis are also important aspects of therapy. Treatment of hypertension with ACE inhibitors requires careful monitoring for renal artery stenosis. Surgery may be needed in patients with critical renal artery stenoses, limb claudication limiting the daily activities, stenosis of three or more cerebral vessels, moderate aortic regurgitation. Stenoses of renal artery are best treated by Percutaneous Transluminal Angioplasty [ 21 ]. Stent placement following angioplasty is a safe and effective procedure [ 22 ]. Takayasu’s Arteritis is a chronic progressive vasculopathy. So long term follow up is recommended. Markers of acute phase response are unreliable during follow up. Doppler studies and MRA are can help to determine the vessel wall thickness and lumen configuration.
Takaysu’s Arteritis can have varied presentation. So a young female patient presenting with absent pulse, unequal blood pressure between arms and hypertension should be suspected clinically for Takayasu’s disease.
Written informed consent was obtained from the patient’s guardian for publication of this case report and for all the accompanying images.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AWC is the first author and was involved in diagnosis by performing the angiography and writing a part of the manuscript. ATMHH is the communicating author and was involved in writing the manuscript. SMEJK and KMNS were responsible for the management of the patient. All the authors read and approved the final manuscript.
Acknowledgement
We acknowledge Professor H I Lutfur Rahman Khan for providing the overall support to us.
- Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004; 113 (3 pt 1):475–482. [ PubMed ] [ Google Scholar ]
- Ooi BS, Chen BTM, Toh CCS, Khoo OT. “Cause of Hypertension in Young” Br Med J. 1970; 3 :744–746. doi: 10.1136/bmj.3.5725.744. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flynn JT. Evaluation and management of hypertension in childhood. Prog Pediatr Cardiol. 2001; 12 :177–188. doi: 10.1016/S1058-9813(00)00071-0. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004; 114 (2 suppl 4th report):555–576. [ PubMed ] [ Google Scholar ]
- Luma GB, Spoitta RT. “Hypertension in Children and Adeloscent” Am Fam Physician. 2006; 73 (9):1558–1566. [ PubMed ] [ Google Scholar ]
- Franco MC, Christofalo DM, Sawaya AL, Ajzen SA, Sesso R. Effects of low birth weight in 8- to 13-yearold children: implications in endothelial function and uric acid levels. Hypertension. 2006; 48 (1):45–50. doi: 10.1161/01.HYP.0000223446.49596.3a. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moore WE, Stephens A, Wilson T, Wilson W, Eichner JE. Body mass index and blood pressure screening in a rural public school system: the Healthy Kids Project. Prev Chronic Dis. 2006; 3 (4):A114. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chugh KS, Jain S, Sakhuja V. Renovascular hypertension due to Takayasu’s Arteritis among Indian patients. QJM. 1992; 85 :833–843. [ PubMed ] [ Google Scholar ]
- Lupi-Herrera E, Sánchez-Torres G, Marcushamer J. Takayasu Arteritis. Clinical study of 107 cases. Am Heart J. 1977; 93 :94–103. doi: 10.1016/S0002-8703(77)80178-6. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Numano F, Okawara M, Inomata H. Takayasu’s Arteritis. Lancet. 2000; 356 :1023–1025. doi: 10.1016/S0140-6736(00)02701-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Watts R, Al Taiar A, Mooney J, Scott D, MacGregor A. The Epidemiology of Takayasu Arteritis in the UK. Rheumatology. 2009; 48 :1008–1011. doi: 10.1093/rheumatology/kep153. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnston SL, Lock RJ, Gompels MM. Takayasu Arteritis: a review. J Clin Pathol. 2002; 55 :481–486. doi: 10.1136/jcp.55.7.481. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moriwaki R, Noda M, Yajima M. Clinical manifestations of Takayasu Arteritis in India and Japan—new classification of angiographic findings. Angiology. 1997; 48 :369–379. [ PubMed ] [ Google Scholar ]
- Jain S, Sharma N, Singh S. Takayasu Arteritis in children and young Indians. Int J Cardiol. 2000; 75 :S153–S157. [ PubMed ] [ Google Scholar ]
- Subramanyan R, Joy J, Balakrishnan KG. Natural history of aortoarteritis (Takayasu’s disease) Circulation. 1989; 80 :429–437. doi: 10.1161/01.CIR.80.3.429. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kerr GS, Hallahan CW, Giordano J. Takayasu Arteritis. Ann Intern Med. 1994; 120 :919–929. [ PubMed ] [ Google Scholar ]
- Ishikawa K. Natural history and classification of occlusive thromboaortopathy (Takayasu’s disease) Circulation. 1978; 57 :27–35. doi: 10.1161/01.CIR.57.1.27. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shelhamer JH, Volkman DJ, Parrillo JE. Takayasu’s Arteritis and its therapy. Ann Intern Med. 1985; 103 :121–126. [ PubMed ] [ Google Scholar ]
- Hoffman GS, Leavitt RY, Kerr GS. Treatment of Takayasu’s Arteritis (TA) with methotrexate (MTX) Arthritis Rheum. 1991; 34 :S74. [ PubMed ] [ Google Scholar ]
- Hoffmann GS, Leavitt RY, Kerr GS. Treatment of glucocorticoid-resistant or relapsing Takayasu Arteritis with methotrexate. Arthritis Rheum. 1994; 37 :578–582. doi: 10.1002/art.1780370420. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Giordano JM. Surgical treatment of Takayasu’s Arteritis. Int J Cardiol. 2000; 75 :S123–S128. [ PubMed ] [ Google Scholar ]
- Sharma BK, Jain S, Bali HK. A follow-up study of balloon angioplasty and de-novo stenting in Takayasu Arteritis. Int J Cardiol. 2000; 75 :S147–S152. [ PubMed ] [ Google Scholar ]
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Pathophysiology and clinical presentation – correct diagnosis

Image Reference: https://blog.ekincare.com/2018/06/29/diagnosis-of-hypertension/
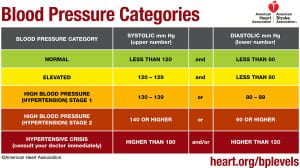
Hypertension or high blood pressure, is when an individual has consistently high arterial blood pressure, also known as the force with which blood flows through a person’s blood vessels (McCance & Huether, 2019). A normal blood pressure reading is a systolic (upper) number lower than 120 mmHg and a diastolic (lower) number that is lower than 80 mmHg (American Heart Association, 2017). Elevated blood pressure is when the systolic (upper) number is 120-129 mmHg with a normal diastolic (lower) number (American Heart Association, 2017). Stage one high blood pressure or hypertension is when the systolic (upper) number is between 130 mmHg and 139 mmHg and the diastolic (lower) number is between 80 and 89 mmHg (American Heart Association, 2017). The second stage of hypertension or high blood pressure is when the systolic (upper) number is 140 mmHg or higher and the diastolic (lower) number is 90 mmHg or higher (American Heart Association, 2017).
For someone to be diagnosed with hypertension their blood pressure measurements have to be taken two separate times that are at least two minutes apart, with the person seated, arm supported at heart level, with the person having rested for at least five minutes, and they should not have been smoking or drank any caffeine in the last 30 minutes (McCance & Huether, 2019). For hypertension to be diagnosed the diastolic and systolic numbers of the two readings are averaged and that measurement are found to be high according to the numbers above (McCance & Huether, 2019). Hypertension is often called a silent disease because in its early stages, there are commonly no other clinical manifestations besides high blood pressure measurements (McCance & Huether, 2019).
Hypertension is thought to be caused by both genetic and environmental factors (McCance & Huether, 2019). Genetic variations that cause the sympathetic nervous system (SNS) or the renin-angiotensin-aldosterone system (RAAS) to be overactive predispose a person to hypertension (McCance & Huether, 2019). Additionally, genetic modifications in the function of renal sodium excretion, sensitivity to insulin, and sodium and/or calcium transport can also contribute to an increased risk for hypertension (McCance & Huether, 2019). Some environmental factors that increase the risk for hypertension include diet, exercise, and smoking (McCance & Huether, 2019).
There are two mechanisms by which blood pressure can be increased: an increase in vascular resistance, an increase in cardiac output, or both (McCance & Huether, 2019). Cardiac output increases when stroke volume or heart rate increases and vascular resistance is increased by vasoconstriction or when the blood becomes thicker (McCance & Huether, 2019). Many pathophysiologic processes are involved in facilitating the maintenance of these mechanisms.
The renal excretion of sodium is one of these processes. Blood volume increases when the renal system excretes less salt due to water retention, thus increasing stroke volume and consequently blood pressure (McCance & Huether, 2019). When this system functions normally , the kidneys excrete the appropriate amount of salt to maintain, but not increase blood pressure. Those with hypertension are more likely to secrete less sodium in their urine at any given blood pressure (McCance & Huether, 2019).
The sympathetic nervous system (SNS) also helps modulate blood pressure by stimulating cardiac contractility and prompting vasoconstriction (McCance & Huether, 2019). It does so by controlling the release of epinephrine and norepinephrine which can bind to either alpha 1 receptors that reside on peripheral blood vessels or beta 1 receptors that reside on cardiac tissue (McCance & Huether, 2019). When this system functions normally , these catecholamines are released in the appropriate amount and interact with their receptors properly. In those with hypertension, there may be an increase in production of these catecholamines or their receptors may be especially reactive (McCance & Huether, 2019). This increased SNS activity triggers the heart rate to increase when affecting the beta 1 receptors and peripheral vasoconstriction when affecting the alpha 1 receptors (McCance & Huether, 2019). Both of these functions raise blood pressure (McCance & Huether, 2019).
There is also a connection between the sympathetic nervous system and kidney function. SNS activity triggers the release of renin, increases the amount of sodium that is reabsorbed, and lowers blood flow to the kidneys (McCance & Huether, 2019).
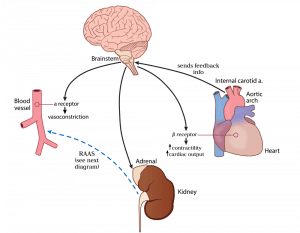
Image Reference: https://hasshe.com/vasodilation-nicotine-5c148fe58719620724c2bbfa/
Hypertension can be affected by inflammation (McCance & Huether, 2019). Injury to endothelial cells, or the cells that line the inside of blood vessels, along with lack of good blood supply to tissues in the body can trigger the immune system to release substances which directly impact the actions of the blood vessels (McCance & Huether, 2019). In a normal short-term injury , the appropriate substances (vasoactive cytokines) are released and help to heal the injured cite without causing overall harm to the body (McCance & Huether, 2019). When an injury to endothelial cells lasts a long time or becomes chronic, the cytokines can cause permanent damage resulting in a change in structure that prevents cells from functioning normally (McCance & Huether, 2019). This permanent change often leads to decreased production of vasodilators, or substances that the body produces to relax the blood vessels (nitric oxide) and an increased production of vasoconstrictors, or substances that the body produces to tighten blood vessels and increase blood pressure (McCance & Huether, 2019). This combination of events leads to an overall increase in blood pressure (McCance & Huether, 2019).
Insulin resistance is commonly associated with hypertension (McCance & Huether, 2019). Insulin resistance occurs when the body has a decreased response to insulin (McCance & Huether, 2019). Insulin is a hormone which normally acts in the body to stabilize blood sugar levels, and in doing so, interacts appropriately with other substances in the body to maintain a normal balance of vasodilators, salt and water (McCance & Huether, 2019). When someone is insulin resistant, there is an associated decrease in release of vasodilators (substances that decrease blood pressure) by endothelial cells (McCance & Huether, 2019). Insulin resistance impacts kidney function which leads to salt and water retention (McCance & Huether, 2019). Overactivity of the SNS and RAAS is also common in patients with insulin resistance (McCance & Huether, 2019). In some patients with diabetes, effective management of blood sugar levels can decrease blood pressure (McCance & Huether, 2019).
Obesity can have a major impact on hypertension (McCance & Huether, 2019). Obesity is associated with increased inflammation, activation of the RAAS and SNS, insulin resistance, as well as kidney and endothelial cell dysfunction (McCance & Huether, 2019). All these phenomena, as discussed above on this page, cause blood pressure levels to rise (McCance & Huether, 2019). Obesity causes changes in the fat tissue’s secretion of adipokines (McCance & Huether, 2019). Normally, adipokines are substances released by fat cells that act to regulate the actions of the fat cells and the tissues which the cells make up (McCance & Huether, 2019). When an individual is obese, there is an associated resistance to the action of an adipokine called leptin (McCance & Huether, 2019). In most individuals without obesity, leptin acts in the fat tissue to reduce the overall weight and fat content in a person (McCance & Huether, 2019). Under normal circumstances, the use of leptin by fat cells leads to its uptake from the blood into cells. In obese individuals, the decreased use of leptin by fat cells leads to an increase in the amount of leptin left circulating in the blood (McCance & Huether, 2019). This increase in leptin levels in the blood cause an increase in SNS activity and affect the kidneys in such a way that leads to less filtering of sodium out of the body (McCance & Huether, 2019).
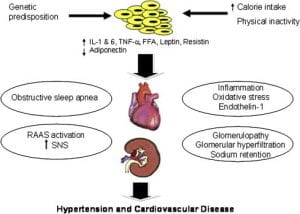
Image Reference:
Kurukulasuriya, lr., md, stas, s., md, lastra, g., md, manrique, c., md and sowers, j.r., md. (1 september 2011). hypertension in obesity [diagram]. retrieved from: https://www-clinicalkey-com.proxy.lib.ohio-state.edu/#/content/playcontent/1-s2.0-s0025712511000629returnurl=https:%2f%2flinkinghub.elsevier.com%2fretrieve%2fpii%2fs0025712511000629%3fshowall%3dtrue&referrer=.
Levels of adiponectin, a protein made by fat tissues, are reduced in obese individuals (McCance & Huether, 2019). This lack of a normal adiponectin level is associated with insulin resistance, decreased nitric oxide (a vasodilator that decreases blood pressure), and an increased activation of the SNS and RAAS (McCance & Huether, 2019). These factors lead to overall constriction of the blood vessels, retention of excess water and salt in the body, and kidney dysfunction (McCance & Huether, 2019). All of these lead to a rise in blood pressure (McCance & Huether, 2019).
Secondary hypertension is when high blood pressure is caused by another disease or medication (McCance & Huether, 2019). Primary hypertension is caused by a combination of one or more factors explained above. Some things that can cause secondary hypertension include kidney disease, tumors associated with the adrenal gland, and medications such as oral contraceptives, antihistamines and corticosteroids (McCance & Huether, 2019) . The cause can be identified and treated or removed to lower blood pressure (McCance & Huether, 2019) .
Hypertension Case Study
Jul 26, 2014
671 likes | 1.71k Views
Hypertension Case Study. Chief Complaint.
Share Presentation
- lung cancer
- high power field
- hypertension case study
- ventricular hypertrophy
- mild expiratory

Presentation Transcript
Chief Complaint • The chief complaint is a brief statement of the reason why the patient consulted the physician, stated in the patient’s own words. In order to convey the patient’s symptoms accurately, medical terms and diagnoses are generally not used. The appropriate medical terminology is used after an appropriate evaluation (i.e., medical history, physical examination, laboratory and other testing) leads to a medical diagnosis.
Chief Complaint • “I just moved to town, and I’m here to see my new doctor for a checkup. I’m just getting over a cold. Overall, I’m feeling fine, except for occasional headaches and some dizziness in the morning. My other doctor prescribed a low-salt diet for me, but I don’t like it!”
HPI • The history of present illness is a more complete description of the patient’s symptom(s). Usually included in the HPI are: • Date of onset • Precise location • Nature of onset, severity, and duration • Presence of exacerbations and remissions • Effect of any treatment given • Relationship to other symptoms, bodily functions, or activities (e.g., activity, meals) • Degree of interference with daily activities
HPI • Sam Street is a 62-year-old African-American male who presents to his new family medicine physician for evaluation and follow-up of his medical problems. He generally has no complaints, except for occasional mild headaches and some dizziness after he takes his morning medications.
He states that he is dissatisfied with being placed on a low sodium diet by his former primary care physician. He reports a “usual” chronic cough and shortness of breath, particularly when walking moderate distances (states, “I’m just out of shape”).
PMH • The past medical history includes serious illnesses, surgical procedures, and injuries the patient has experienced previously. Minor complaints (e.g., influenza, colds) are usually omitted unless they might have a bearing on the current medical situation.
PMH • Hypertension × 15 years • Type 1 diabetes mellitus • Chronic obstructive pulmonary disease, Stage 2 (Moderate) • Benign prostatic hyperplasia • Chronic kidney disease
FH • The family history includes the age and health of parents, siblings, and children. For deceased relatives, the age and cause of death are recorded. In particular, heritable diseases and those with a hereditary tendency are noted (e.g., diabetes mellitus, cardiovascular disease, malignancy, rheumatoid arthritis, obesity).
FH • Father died of acute MI at age 71. Mother died of lung cancer at age 64. Mother had both HTN and DM.
SH • The social history includes the social characteristics of the patient as well as the environmental factors and behaviors that may contribute to the development of disease. Items that may be listed are the patient’s marital status; number of children; educational background; occupation; physical activity; hobbies; dietary habits; and use of tobacco, alcohol, or other drugs.
SH • Former smoker (quit 3 years ago; smoked 1 ppd × 28 years); reports moderate amount of alcohol intake. He admits he has been nonadherentto his low sodium diet (states, “I eat whatever I want.”) He does not exercise regularly and is limited somewhat functionally by his COPD. He is retired and lives alone.
Meds: • The medication history should include an accurate record of the patient’s current use of prescription medications, nonprescription products, and dietary supplements. Because pharmacists possess extensive knowledge of the thousands of prescription and nonprescription products available, they can perform a valuable service to the health care team by obtaining a complete medication history that includes the names, doses, routes of administration, schedules, and duration of therapy for all medications, including dietary supplements and other alternative therapies.
Meds: • Triamterene/hydrochlorothiazide 37.5 mg/25 mg po Q AM • Insulin 70/30, 24 units Q AM, 12 units Q PM • Doxazosin 2 mg po Q AM • Albuterol INH 2 puffs Q 4–6 h PRN shortness of breath • Tiotropium DPI 18 mcg 1 capsule INH daily • Salmeterol DPI 1 INH BID • Entex PSE 1 capsule Q 12 h PRN cough and cold symptoms • Acetaminophen 325 mg po Q 6 h PRN headache
ALL: • Allergies to drugs, food, pets, and environmental factors (e.g., grass, dust, pollen) are recorded. An accurate description of the reaction that occurred should also be included. Care should be taken to distinguish adverse drug effects (“upset stomach”) from true allergies (“hives”).
All • PCN—Rash
ROS • In the review of systems, the examiner questions the patient about the presence of symptoms related to each body system. In many cases, only the pertinent positive and negative findings are recorded. In a complete ROS, body systems are generally listed by starting from the head and working toward the feet and may include the skin, head, eyes, ears, nose, mouth and throat, neck, cardiovascular, respiratory, gastrointestinal, genitourinary, endocrine, musculoskeletal, and neuropsychiatric systems.
The purpose of the ROS is to evaluate the status of each body system and to prevent the omission of pertinent information. Information that was included in the HPI is generally not repeated in the ROS.
ROS • Patient states that overall he is doing well and just getting over a cold. He has noticed no major weight changes over the past few years. He complains of occasional headaches, which are usually relieved by acetaminophen, and he denies blurred vision and chest pain. He states that his shortness of breath is “usual” for him, and that his albuterol helps.
He denies experiencing any hemoptysis or epistaxis; he also denies nausea, vomiting, abdominal pain, cramping, diarrhea, constipation, or blood in stool. He deniesurinary frequency, but states that he used to have difficulty urinating until his physician started him on doxazosin a few months ago.
Physical Examination • The exact procedures performed during the physical examination vary depending upon the chief complaint and the patient’s medical history. In some practice settings, only a limited and focused physical examination is performed. In psychiatric practice, greater emphasis is usually placed on the type and severity of the patient’s symptoms than on physical findings. A suitable physical assessment textbook should be consulted for the specific procedures that may be conducted for each body system. The general sections for the PE are outlined as follows:
Gen (general appearance) • VS (vital signs)—blood pressure, pulse, respiratory rate, and temperature. • In hospital settings, the presence and severity of pain is included as “the fifth vital sign, weight and height are included in the vital signs section here, but they are not technically considered to be vital signs. • Skin (integumentary)
HEENT (head, eyes, ears, nose, and throat) • Lungs/Thorax (pulmonary) • Cor or CV (cardiovascular) • Abd (abdomen) • Genit/Rect (genitalia/rectal) • MS/Ext (musculoskeletal and extremities) • Neuro (neurologic)
Gen: • WDWN, African-American male; moderately overweight; in no acute distress. • WDWN = Well-developed, well-nourished.
VS • BP 168/92 mm Hg (sitting; repeat 170/90), HR 76 bpm (regular), RR 16 per min, T 37°C; Wt 95 kg, Ht 6'2'‘ • BP = Blood Pressure. • HR = Heart rate. • Bpm = beat per minute. • RR = Respiratory rate. • T = Temperature. • Wt = Weigt • Ht= Hight
HEENT • TMs clear; mild sinus drainage; AV nicking noted; no hemorrhages, exudates, or papilledema. • TM = Tympanic membrane. • AV = arteriovenous
Neck: • Supple without masses or bruits, no thyroid enlargement or lymphadenopathy Lungs: • Lung fields CTA bilaterally. Few basilar crackles, mild expiratory • wheezing
Heart: • RRR; normal S1 and S2. No S3 or S4 • RRR = Regular rate and rhythm. • S = Sound.
Abd: • Soft, NTND; no masses, bruits, or organomegaly. Normal BS. • NTND = Non-tender/non-distended. • BS = Bowel sounds; breath sounds or blood sugar
Genit/Rect: • Enlarged prostate; benign Ext: • No CCE. • CCE = Clubbing, cyanosis, edema
Neuro: • No gross motor-sensory deficits present. CN II–XII intact. A & O × 3. • CN II–XII = Cranial Nerves 2 to 12. • A & O × 3 = Awake and oriented to person, place, and time.
UA: • Yellow, clear, SG 1.007, pH 5.5, (+) protein, (–) glucose, (–) ketones, (–) bilirubin, (–) blood, (–) nitrite, RBC 0/hpf, WBC 1–2/ hpf, . negbacteria, 1–5 epithelial cells. • Hpf = High Power Field. • SG = Specific gravity.
ECG • Normal sinus rhythm ECHO (6 months ago): • Mild LVH, estimated EF 45%: • LVH = Left ventricular hypertrophy. • EF = Ejection fraction.
Assessment: • Hypertension, uncontrolled • Type 1 diabetes mellitus, controlled on current insulin regimen • Moderate COPD, stable on current regimen • BPH, symptoms improved on doxazosin
Problem Identification • 1.a. Create a list of this patient’s drug-related problems, including any medications which may be contributing to the patient’s uncontrolled hypertension.
DDIs: • Significant - Monitor Closely • triamterene + albuterol • triamterene increases and albuterol decreases serum potassium. Effect of interaction is not clear, use caution. Significant - Monitor Closely. • triamterene + salmeterol • triamterene increases and salmeterol decreases serum potassium. Effect of interaction is not clear, use caution. Significant - Monitor Closely. • albuterol + salmeterol • albuterol and salmeterol both decrease serum potassium. Significant - Monitor Closely.
albuterol + hydrochlorothiazide • albuterol and hydrochlorothiazide both decrease serum potassium. Significant - Monitor Closely. • salmeterol + hydrochlorothiazide • salmeterol and hydrochlorothiazide both decrease serum potassium. Significant - Monitor Closely. • albuterol + salmeterol • albuterol and salmeterol both decrease sedation. Significant - Monitor Closely. • albuterol + salmeterol • albuterol and salmeterol both increase sympathetic (adrenergic) effects, including increased blood pressure and heart rate. Significant - Monitor Closely.
Minor • albuterol + hydrochlorothiazide • albuterol, hydrochlorothiazide. Mechanism: pharmacodynamic synergism. Minor or non-significant interaction. Hypokalemia. • salmeterol + hydrochlorothiazide • salmeterol, hydrochlorothiazide. Mechanism: pharmacodynamic synergism. Minor or non-significant interaction. Hypokalemia. • hydrochlorothiazide + insulin glargine • hydrochlorothiazide decreases effects of insulin glargine by pharmacodynamic antagonism. Minor or non-significant interaction. Thiazide dosage >50 mg/day may increase blood glucose.
Problem Identification • 1.b. How would you classify this patient’s HTN (e.g., Prehypertension, Stage 1, or Stage 2), according to JNC 7 Guidelines? • 1.c. What are the patient’s known cardiovascular risk factors, and what is the patient’s Framingham risk score? • 1.d. What evidence of target organ damage or clinical cardiovascular disease does this patient have?
Framingham Risk score calculator • http://hp2010.nhlbihin.net/atpiii/calculator.asp
Desired Outcome • 2. List the goals of treatment for this patient (including the patient’s goal blood pressure, according to JNC 7 Guidelines).
Therapeutic Alternatives • 3.a. What lifestyle modifications should be encouraged for this patient to achieve and maintain adequate blood pressure reduction?
Therapeutic Alternatives • 3.b. What reasonable pharmacotherapeutic options are available for controlling this patient’s blood pressure, and what comorbidities and individual patient considerations should be taken into account when selecting pharmacologic therapy for his HTN? How might Mr. Street’s HTN medications potentially affect his other medical problems?
Optimal Plan • 4.a. Outline specific lifestyle modifications for this patient. • 4.b. Outline a specific and appropriate pharmacotherapeuticregimen for this patient’s uncontrolled hypertension, including drug(s), dose(s), dosage form(s), and schedule(s).
Outcome Evaluation • 5. Based on your recommendations, what parameters should be monitored after initiating this regimen and throughout the treatment course? At what time intervals should these parameters be monitored?
Patient Education • 6. Based on your recommendations, provide appropriate education to this patient.
- More by User
Case Study. Dominican Republic – Measures Affecting the Importation and Internal Sale of Cigarettes 蔡奉真、黃琳君、李炎蒼. Parties and measure in dispute. parties : Dominican Republic Honduras Measure in dispute : 一、多明尼加要求於該國境內銷售之香菸,不論是否進口產品,包裝上均應貼上印花,以證明已經繳稅得以合法銷售。
1.25k views • 37 slides
Case Studies in Acute Hypertension
Investigations ● Advances ● Applications. Case Studies in Acute Hypertension. Edwin G. Avery, MD, CPI Assistant Professor of Anesthesiology Massachusetts General Hospital Heart Center Harvard Medical School . Case Study #1. Case Studies of Acute Hypertension. Type A Aortic Dissection.
1.33k views • 32 slides
Case Study. Presented by. Araro Jireh Ary Andana Bambang Wijarnako. The Content. Southwest Airlines at a Glance. What makes SWA Different?. Case Analysis. Recommendation. Southwest Airlines at a Glance. Southwest Airlines at a Glance.
1.38k views • 21 slides
Haemorrhagic Fever In search of the “culprit ”. CASE STUDY. Study case presented by Daniele de Meneghi: UNITO_FMV, Italy ; Carla Rosenfeld: UACH, Chile; Ludovina Padre: UEVORA, Portugal; Carolina Pujol: UABC, Mexico , SAPUVETNET III members of group VII.
875 views • 27 slides
Case Study.
612 views • 7 slides
Case Study. By: Carla Norman. Part A: Getting to know your student. Motivation Survey Strengths: concept of print, return sweep, and word boundary Weaknesses: word formation, letter/sound association, reading comprehension
372 views • 9 slides
Hypertension A Case Study
Hypertension A Case Study. Jennifer Kitchen July 19, 2013. Vicki, a patient just diagnosed with Hypertension (HTN) What is Hypertension? Appropriate T reatment Prognosis (including therapies, medications, etc.) Patient Teaching Potential B arriers to Therapy. O verview. 42 years old
3.32k views • 12 slides
Hypertension Case Presentation
Hypertension Case Presentation. Kori Lawie , Pharm. d candidate SaRAH DAOUD, PHARM. D CANDIDATE Preceptor: dr. Thomas Robertson. Objectives. Case Overview Define hypertension Discuss diagnostic criteria Identify the pathophysiology of hypertension Identify the pathophysiology of NIDDM
2.21k views • 31 slides
Case Study. Prasun K Jalal MD Baylor College of Medicine. Case no. 1. 53/M, Caucasian Fatigue and lower extremity swelling- 6 m H/O IV drug use in 1970’s Drinks 2-3 beer a day for 20 yrs, stopped 6 m back. Examination. BMI 35 Spider angioma on chest Hepatosplenomegaly
747 views • 38 slides
CASE STUDY. Learning Objectives. To research and revise the case study for Section B of the exam. Warp Documentary.
523 views • 16 slides

Case Study . The Study of an Environmental Impact Statement for a Wind Farm Liam Dervan, EHO Galway. E.I.S. Team, Galway. Under the auspices of; Mr Brendan Lawlor, A/PEHO Team Members; Mr Gerry Leen, SEHO Mr Seamus Mitchell, SEHO Ms Niamh Kelly, EHO
669 views • 45 slides
Case Study. Deirdre Downes. My Father: My Siblings Mother, and Mom likes me best. Many Siblings One Health Care Proxy: the story of Mr. L
305 views • 7 slides
Case Study. Blood Diamonds & Human Rights in Africa. Bell Work . Finish the following words or sentences with as many words or phrases as you can. “Diamonds are …”. Blood Diamonds.
589 views • 11 slides
A CASE OF MALIGNANT HYPERTENSION
A CASE OF MALIGNANT HYPERTENSION. DR ANN HOLMES GPST2. CASE. Px, 56, c/o loss of central vision R eye, blurred vision L +mild generalised headache.
571 views • 16 slides
Case Study. The Ombudsman Perspective. What safety issues would you look for in this resident’s case?.
372 views • 11 slides
Case Study. The Financial Professional recommended that they put their retirement funds into a product such as an annuity with a guaranteed principal feature. The Financial Professional helped Dan and Sheryl purchase a conservative
534 views • 1 slides
Case Study. Integrated Metadata Driven Statistical Data Management System (IMD SDMS) CSB of Latvia [email protected] METIS 2010. Outline. The main steps for IMD SDMS creation IMD SDMS fundamental elements Costs & benefits IMD SDMS implementation strategy
477 views • 20 slides
Ted A. Bonebrake, M.D. Case Study. Initial Presentation.
958 views • 63 slides

A Case of Hypertension
A Case of Hypertension. Dr. Susan Poe, case presentation Dr. Paul Kellerman, topic discussion October 10, 2007. No financial incentives. Case.
1.9k views • 14 slides
CASE STUDY. We are going to analyze and review the zero tolerance policy but in terms of using “common sense.’ Today’s case study will take place in three different school campuses, simultaneously. Keep in mind: The definition of violence. The need for a zero tolerance policy.
941 views • 23 slides
AIRLIE Hypertension Study
AIRLIE Hypertension Study. A utomated I ntervention to R educe L ifestyle I mpact on E merging Hypertension. Principal Investigator Judith McCalla, PhD Co-Investigators Ali Ahmed, MD Shawna Ehlers, PhD Kevin Everett, PhD Paula Rhode, PhD Tracy Riley, PhD, RN. Consultants
392 views • 30 slides
GWS:is hypertension a special case
GWS:is hypertension a special case. Genome Scans in complex traits: is hypertension a special case? Anna F Dominiczak. Guilt by association- WTCCC.
282 views • 14 slides
- Letter to the Editor
- Open access
- Published: 14 August 2024
The first case of heterotopic auxiliary liver transplantation of discarded right hemiliver allograft with intrahepatic bile duct stones
- Bangyou Zuo 1 ,
- Xinyu You 1 ,
- Tao Liu 1 ,
- Jipeng Jiang 1 ,
- Donghui Cheng 1 ,
- Peng Li 1 ,
- Chong Yang 1 &
- Yu Zhang 1
Journal of Translational Medicine volume 22 , Article number: 765 ( 2024 ) Cite this article
Metrics details
To the editor:
Due to the shortage of donor organs for transplantation, liver transplantation from marginal donors has been accepted as a treatment option [ 1 ]. Technical advances in transplantation, such as auxiliary liver transplantation, reduced size transplantation, split liver transplantation and the use of living donors for partial liver transplantation, as well as changes in immunosuppression and improvements in prophylaxis, have led to improved survival rates [ 2 , 3 ].
In this paper, we present the first successful case of heterotopic auxiliary liver transplantation using a discarded liver from intrahepatic bile duct stones. The procedure was modified by performing a splenectomy and implanting the graft into the splenic fossa. The patient recovered well after transplantation.
Case presentation
A morbidly 54-year-old male presented to the emergency department with acute portal hypertension-related gastrointestinal hemorrhage. Vital signs were within the normal range. Upon admission, a physical examination revealed splenomegaly and mild ascites. Abdominal ultrasonography and computed tomography demonstrated marked liver cirrhosis and splenomegaly. He had severe cirrhosis and was on the liver transplantation waiting list in the China Organ Transplant Response System (blood group, O+). Given his critical clinical condition, emergent liver transplantation was indicated.
Thankfully, a 24-year-old female with intrahepatic bile duct stones in the right lobe had blood group O+. The patient planned to undergo a right hemi-hepatectomy and volunteered to donate her resected right lobe, which would otherwise be discarded. The calculated volume of the right lobe on computed tomography (CT) volumetry was 286 ml, resulting in a predicted graft-to-recipient weight ratio (GRWR) of 0.49%, which is insufficient for orthotopic liver transplantation [ 4 ]. Prior to the surgical procedure, a three-dimensional reconstruction of the donor liver was created (Fig. 1 A) in order to facilitate a more comprehensive evaluation of the anatomical structure.

Figure A, preoperative three-dimensional reconstruction of the patient’s hepatic ducts reveals the presence of a stenosis in the right hepatic duct. Figure B, the patient exhibited a markedly enlarged right posterior inferior vein, which exerted a considerable influence on subsequent venous outflow tract reconstruction. Figure C, the intraoperative situation revealed the presence of stones within the right anterior and right posterior hepatic ducts following the incision of the stenotic right hepatic duct. Figure D, the excised right half of the liver was trimmed, the outflow tract was reconstructed, and the complete removal of the stone was confirmed. Figure E-F, postoperative enhanced CT imaging demonstrated the satisfactory condition of the grafts and vessels. RHD, right hepatic duct; RPIV, right posterior inferior vein; IVC, inferior vena cava; PV, portal vein; RPHD, right posterior hepatic duct; RAHD, right anterior hepatic duct; RHV, right hepatic vein; RHA, right hepatic artery
In the surgical procedure, the porta hepatis was first exposed, followed by the right hepatic artery and right portal vein. In close proximity to the posthepatic inferior vena cava, a thick right posterior inferior vein is observed (Fig. 1 B). Following the dissection of the right hepatic duct, the right anterior and posterior lobe bile ducts were clipped separately (Fig. 1 C), and stones were extracted using a choledochoscope. The liver was then split along the right edge of the middle hepatic vein up to the second porta hepatis, revealing the thick right posterior inferior vein and the right hepatic vein.
After heparinization, the proximal part of vessels was clipped successively via laparoscopy. The liver graft was quickly transferred and infused with enough cold UW (University of Wisconsin) solution through the portal vein until clear solution flowed out. We then reconstructed the hepatic vein, using an artificial vessel to bring the two thick veins together (Fig. 1 D). Furthermore, the complete removal of the stone was confirmed.
At the same time as the donor surgery, the recipient underwent splenectomy with excellent preservation of the splenic vessels. The absence of tumor and hepatic fibrosis was confirmed by a rapid intraoperative biopsy before transplantation to the recipient. The graft was then implanted into the recipient’s splenic fossa. Anastomosis of the vessels was then performed. The reconstruction of the hepatic biliary duct was performed by Roux-en-Y biliary-jejunal anastomosis.
Recipients underwent standard thromboprophylaxis and immunosuppression were administered in the postoperative period. And the postoperative enhanced CT scan demonstrated satisfactory graft hematopoiesis (Fig. 1 E-F). The postoperative recovery of the donor and recipient was uncomplicated, and they were discharged home on the 8th and 17th postoperative days, respectively. The volume of the liver increased from 286 g at the time of surgery to a predicted 642 ml (post-operative day 8), and 731 ml (post-operative day 16).
In this case, the patient required a splenectomy due to portal hypertension, splenomegaly, and hypersplenism. We successfully preserved the splenic vasculature and used the discarded liver with intrahepatic bile duct stones (which had been drained of stones) as a heterotopic auxiliary liver graft. This was an initial exploration, which we felt was safer compared to traditional living donor liver transplantation. The ligation of the left renal vein did not result in any impairment of renal function. In fact, the size of the left renal vein was found to be within the normal range following the ligation of the left renal vein [ 5 ].
One potential drawback of heterotopic auxiliary partial liver transplantation for cirrhotic liver disease is the risk of carcinogenesis in the residual native liver. This issue remains to be discussed. However, as the size of the auxiliary liver increases, it can be evaluated for a second-stage resection of the native liver.
Both operations were successfully completed in the donors and recipients. The findings of our study indicate that the discarded right half of the liver following laparoscopic resection for intrahepatic bile duct stones may be utilized as an auxiliary transplanted liver for the treatment of patients with portal hypertension and need emergent liver transplantation.
Data availability
Data are available upon request.
Sun B, Mu X, Wang X. Successful adult-to-adult liver transplantation of an otherwise discarded partial liver allograft with a cavernous hemangioma: new strategy for expanding liver donor pool. Transpl Int. 2013;26:e79–80.
Article PubMed Google Scholar
Pei JH, Shen CH, Li RD, Tao YF, Lu L, Wang ZX. Successful adult-to-pediatric liver transplantation of discarded partial liver allograft with benign caudate lobe tumor. Hepatobiliary Pancreat Dis Int. 2023;22:92–5.
Tan M, Di Carlo A, Robinson P, Tchervenkov JI, Barkun JS, Metrakos P. Successful outcome after transplantation of a donor liver with focal nodular hyperplasia. Liver Transpl. 2001;7:652–5.
Article CAS PubMed Google Scholar
Ikegami T, Yoshizumi T, Sakata K, Uchiyama H, Harimoto N, Harada N, Itoh S, Nagatsu A, Soejima Y, Maehara Y. Left lobe living donor liver transplantation in adults: what is the safety limit? Liver Transpl. 2016;22:1666–75.
Dou K, Wang D, Tao K, Yue S, Ti Z, Song Z, Li L, He Y, Hou X. A modified heterotopic auxiliary living donor liver transplantation: report of a case. Ann Hepatol. 2014;13:399–403.
Download references
The Natural Science Foundation of China (82373189), the Youth Talent Fund of Sichuan Provincial People’s Hospital (2022QN53), and the Science and Technology Department of Sichuan Province (2024NSFSC1935).
Author information
Authors and affiliations.
Department of Hepatobiliary and Pancreatic Surgery, Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China, Chengdu, China
Bangyou Zuo, Xinyu You, Tao Liu, Jipeng Jiang, Donghui Cheng, Peng Li, Chong Yang & Yu Zhang
You can also search for this author in PubMed Google Scholar
Contributions
(I) Conception and design: Bangyou Zuo, Yu Zhang and Xinyu You; (II) Administrative support: Bangyou Zuo, Tao Liu and Yu Zhang (III) Provision of study materials or patients: Bangyou Zuo and Chong Yang (IV) Collection and assembly of data: Donghui Cheng, Jipeng Jiang and Peng Li (V) Data analysis and interpretation: (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
Corresponding author
Correspondence to Yu Zhang .
Ethics declarations
Ethics and informed consent.
The procurement of the graft from the discarded liver (living donor) were approved by the Medical Affairs Department and the Ethics Committee of the Sichuan Provincial People’s Hospital, and informed consent was obtained from the patient.
Disclosures
The authors of this manuscript have no conflicts of interest to disclose.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zuo, B., You, X., Liu, T. et al. The first case of heterotopic auxiliary liver transplantation of discarded right hemiliver allograft with intrahepatic bile duct stones. J Transl Med 22 , 765 (2024). https://doi.org/10.1186/s12967-024-05584-y
Download citation
Received : 30 July 2024
Accepted : 04 August 2024
Published : 14 August 2024
DOI : https://doi.org/10.1186/s12967-024-05584-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Journal of Translational Medicine
ISSN: 1479-5876
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Enhancing Diagnostics with AI-Driven Medical Analysis
Miguel Nunez
Aug 13, 2024, 8:22 PM
HCA Healthcare – Enhancing Diagnostics with AI-Driven Medical Analysis
In collaboration with Vanderbilt Data Science, HCA Healthcare embarked on a project to improve the identification of vascular conditions from radiology reports. By leveraging advanced AI techniques, the project aimed to enhance the accuracy and efficiency of medical diagnoses, ultimately improving patient outcomes. This initiative marks a significant step forward in applying AI to healthcare, providing faster and more reliable diagnostic processes.
AI-Driven Diagnostics Presentation
The project was presented by a student of Vanderbilt’s Data Science program who showcased the use of a transformer-based AI model to analyze and interpret radiology reports. This AI-driven approach moved beyond traditional keyword-matching algorithms, offering a more sophisticated method to accurately identify vascular conditions.
Project Highlights:
Over the course of the project, the team focused on several key aspects of AI-driven medical analysis, including:
- Purpose: To enhance the identification of vascular conditions from radiology reports, providing quicker and more accurate diagnoses to improve patient care.
- Techniques: The project utilized a fine-tuned transformer-based model, specifically RadBERT, designed for medical contexts to understand and interpret complex medical terminology.
- Applications: The AI model was implemented to support medical professionals by reducing their workload, cutting operational costs, and ensuring timely and accurate evaluations.
Session Insights:
- The use of RadBERT significantly improved the accuracy of identifying vascular conditions, showcasing the potential of AI in medical diagnostics.
- This project demonstrated that AI-driven models could effectively streamline the diagnostic process, leading to better patient outcomes and more efficient healthcare operations.
- The collaboration highlighted the importance of integrating cutting-edge technology in healthcare to enhance care delivery and operational efficiency.
Project Data:
This collaboration between HCA Healthcare and Vanderbilt Data Science exemplifies the transformative potential of AI in healthcare. By focusing on improving diagnostic accuracy and efficiency, the project opens up multiple forward-facing avenues for ai-integration in medical technology.
What is a capstone project?
Explore story topics.
- - Generative AI
- Capstone Case Study
- Medical Sciences
- Natural and Life Sciences

COMMENTS
Patient Case Presentation. Mr. E.A. is a 40-year-old black male who presented to his Primary Care Provider for a diabetes follow up on October 14th, 2019. The patient complains of a general constant headache that has lasted the past week, with no relieving factors. He also reports an unusual increase in fatigue and general muscle ache without ...
Presentation of Case Dr. Sally A. Ingham (Medicine): A 45-year-old woman was admitted to this hospital because of dyspnea on exertion, fatigue, and confusion.
PowerPoint Presentation. hypertension Case Study2017 Nicolas E. Davies Community Health Award of ExcellenceUnity Health Care, Inc.Washington, DC. Overview. About Unity Health Care. Hypertension Case Study. HIMSS Davies Application Team. Catherine Anderton, Associate Director for Quality Improvement and Research. Angela Diop.
IntroductIon: Hypertension is highly prevalent among aging adults and can lead to coronary artery disease, diastolic and systolic heart failure and other cardiovascular conditions. Hypertension is also known to worsen clinical heart failure since high afterload increases the work of the heart, prompting a maladaptive state that is reflected by congestion, fatigue and edema.
Objectives Case Overview Define hypertension Discuss diagnostic criteria Identify the pathophysiology of hypertension Identify the pathophysiology of NIDDM Discuss treatment strategies for hypertension Evaluate and assess the patient's current drug therapy Discuss pharmacist's care plan Discuss counseling points
Case Presentation. The patient was a 17-year-old male who was admitted to our hospital in May 2020 due to uncontrolled hypertension for 6 months and weakness of limbs for 20 days. Six months prior to admission, blood pressure of the patient was found to have increased to 200/120 mmHg during the physical examination.
Hypertension A Case Study. Jennifer Kitchen July 19, 2013. Vicki, a patient just diagnosed with Hypertension (HTN) What is Hypertension? Appropriate T reatment Prognosis (including therapies, medications, etc.) Patient Teaching Potential B arriers to Therapy. O verview. 42 years old
Hypertension Case Presentation. Kori Lawie , Pharm. d candidate SaRAH DAOUD, PHARM. D CANDIDATE Preceptor: dr. Thomas Robertson. Objectives. Case Overview Define hypertension Discuss diagnostic criteria Identify the pathophysiology of hypertension Identify the pathophysiology of NIDDM
Definitions used in these clinical case scenarios. Definitions Stage 1 hypertension Clinic blood pressure is 140/90 mmHg or higher and. subsequent ambulatory blood pressure monitoring (ABPM) daytime average or home blood pressure monitoring (HBPM) average blood pressure is 135/85 mmHg or higher. Stage 2 hypertension Clinic blood pressure is 160 ...
Download ppt "Hypertension Case Study". Chief Complaint The chief complaint is a brief statement of the reason why the patient consulted the physician, stated in the patient's own words. In order to convey the patient's symptoms accurately, medical terms and diagnoses are generally not used. The appropriate medical terminology is used after ...
Presentation L.N. is a 49-year-old white woman with a history of type 2 diabetes,obesity, hypertension, and migraine headaches. The patient was diagnosed with type 2 diabetes 9 years ago when she presented with mild polyuria and polydipsia. L.N. is 5′4″ and has always been on the large side,with her weight fluctuating between 165 and 185 lb. Initial treatment for her diabetes consisted of ...
Here we report a teenager with Takayasu Arteritis who presented with uncontrolled hypertension. This case depicts an atypical presentation of this disease where the girl visited many physicians for controlling the level of hypertension and put a diagnostic dilemma about the underlying etiology of young hypertension.
CASE 7 56 year old man with hypertension presented to a primary stroke center (PSC) with acute-onset right-sided weakness and inability to talk. NIHSS 23 on presentation, consistent with large left MCA syndrome. Non-contrast head CT showed a dense L MCA (figure 1A) without early infarct changes, ASPECTS 10 (figure 1B).
Hypertension or high blood pressure, is when an individual has consistently high arterial blood pressure, also known as the force with which blood flows through a person's blood vessels (McCance & Huether, 2019). A normal blood pressure reading is a systolic (upper) number lower than 120 mmHg and a diastolic (lower) number that is lower than ...
Presentation Transcript Hypertension Case Study Chief Complaint • The chief complaint is a brief statement of the reason why the patient consulted the physician, stated in the patient's own words. In order to convey the patient's symptoms accurately, medical terms and diagnoses are generally not used.
Case presentation A 49-year-old male patient visited our hospital on January 24, 2019, with back and subxiphoid pain that had persisted for 11 hours. He had no history of hypertension, hyper-lipidemia, stroke, diabetes mellitus, peripheral artery disease, coronary heart disease, autoimmune disease, or tumor disease, as well as no early family ...
We present a case report of cement reaction with unusual presentation, that is, hypoxia, hypertension and tachycardia. A 74-year-old hypertensive male on regular medications sustained a slip and fall, presented with a right intertrochanteric neck of femur fracture, now posted for cemented hemiarthroplasty.
Idiopathic intracranial hypertension (IIH) is a condition characterized by increased pressure around the brain, leading to symptoms including vision changes, headaches, and other neurological issues. The effect of yoga nidra on IIH is still unexplored. This case study investigates the effect of yoga nidra on a 16-year-old female with a known case of IIH with episodic seizures. The patient ...
Case presentation. A morbidly 54-year-old male presented to the emergency department with acute portal hypertension-related gastrointestinal hemorrhage. ... The findings of our study indicate that the discarded right half of the liver following laparoscopic resection for intrahepatic bile duct stones may be utilized as an auxiliary transplanted ...
HCA Healthcare - Enhancing Diagnostics with AI-Driven Medical Analysis In collaboration with Vanderbilt Data Science, HCA Healthcare embarked on a project to improve the identification of vascular conditions from radiology reports. By leveraging advanced AI techniques, the project aimed to enhance the accuracy and efficiency of medical diagnoses, ultimately improving patient outcomes. This ...