Health Sector of India
COVID-19 exposed several weaknesses in India’s underfunded health system. Rural primary care is underfunded and has shortages of staff, equipment, drugs and infrastructure in many parts of the country. Urban primary healthcare has still not emerged as an active programme in many States. District and medical college hospitals suffer shortages of specialist doctors and support staff.

| General facts about Health and Nutrition | |
| Birth Rate (2021)
| 16 Live Births (per thousand of the population) ???? declining |
|
| 70 Years 70 Years, 67 Years |
| Infant Mortality Rate (IMR)
| As per Sample Registration System (SRS) Bulletin of Registrar General of India (RGI) it is IMR is 30 per 1,000 live births in 2019 at National Level. IMR by 42% over 11 years but still higher than global average (29) |
| Neonatal Mortality Rate (NMR) (NHFS – 5, 2019-21) | 25 16 deaths per 1000 live births by 2025. (With the current trend, India would fail to achieve this) 12 deaths per 1000 live births by 2030 |
| Maternal Mortality Ratio (National Health Profile 2021) | India on track to achieve the SDG target |
| Total Fertility Rate (TFR) (NFHS – 5, 2019-21) | 2.0 (Below Replacement Levels) Bihar, Meghalaya, Uttar Pradesh, Jharkhand, and Manipur. |
| Sex Ratio at Birth (SRB) (NFHS – 5, 2019-21) | – 1020 (increased from 933 in Census 2001) – 929 |
| Proportion of institutional deliveries (NFHS - 5) | increased from 40% in 2005-06 to 100% institutional Deliveries |
| Doctor Density | (allopathic + AYUSH doctors) |
| AYUSH | |
| Disease Burden and Measures | |
| Non-communicable diseases (NCD) (WHO report) | NCD responsible for > 60% of all deaths in India can be attributed to NCDs. risks dying from an NCD before they reach the age of 70. alone account for 55% of the premature mortality in India in the age group of 30?69 years. Physical inactivity, tobacco use, excessive use of alcohol, unhealthy diets and Psycho-Social Stress. |
| HIV/AIDS (SDG INDIA INDEX 2.0) | : 3rd largest HIV/AIDS population in world per 1000 uninfected population declined from 0.64 in 1995 to 0.07 in 2017. |
| Tuberculosis (TB) (Annual TB Report 2022) | (28%) in the world and highest number of cases (WHO, 2019). India has the second-highest number globally. |
| Food and Nutrition | |
| Hunger & Malnutrition in India (NFHS- 5) | 20% of men are undernourished aged between 15 - 49 years are anaemic. under age of 5 years are anaemic. global Average: 13%) % |
| Obesity in India (NFHS - 5) | in the world after the US and China |
Issues and Challenges for health sector
India’s healthcare system has been battling various issues, including the low number of institutions and less-than-adequate human resources for quite a while now.
- Lack of Infrastructure: India has been struggling with deficient infrastructure in the form of lack of well-equipped medical institutes for quite a while now.
- For a considerable time, the government regulation mandated that private medical colleges must be built on at least five acres of land.
- As a result, quite a few private colleges were built in rural areas, where it became quite difficult to recruit adequately qualified, full-time doctors due to lack of proper living conditions, besides low pay scales.
- National Medical Commission (NMC) has put forward the idea to do away with the requirement of minimum five acres of land for setting up a medical college.
- Further, the commission has proposed to curtail the minimum number of beds required as a proportion of the number of seats in the college.
- Shortage of trained manpower: this includes doctors, nurses, paramedics and primary healthcare workers.
- The situation remains worrisome in rural areas, where almost 66 per cent of India’s population resides.
- The doctor-to-patient ratio remains abysmally low, which is merely 0.7 doctors per 1,000 people. This is compared to the World Health Organisation (WHO) average of 2.5 doctors per 1,000 people.
- Unmanageable load of Patients: Healthcare facilities had been feeling the strain due to unmanageable patient-load.
- In addition, there is the challenge to think beyond the obvious and promote virtual care protocols, and telehealth services, which can be leveraged to reduce the patient-load burden to a large extent.
- Public health policy and proactive healthcare: The latest National Health Policy (NHP) 2017 highlights the ‘Health for All’ approach to provide assured healthcare for all at an affordable cost.
- Ideally, the public health policy needs to be focussed towards proactive healthcare, not reactive healthcare.
- High out-of-pocket expenditure remains a stress factor: While public hospitals offer free health services, these facilities are understaffed, poorly equipped, and located mainly in urban areas.
- Most health services are, therefore, provided by private facilities, and 65 per cent of medical expenses in India are paid out of pocket by patients.
- Unregulated private sector: NITI Aayog has recently published the document, ‘Investment Opportunities in India’s Healthcare Sector’. This promotes further privatisation of health care in a country which already has one of the most privatised health systems in the world .
- The report fails to acknowledge the negative aspects of unregulated private health care; neither is there any mention of the need for regulation of private hospitals.

Government Initiatives
- Anganwadi System: The Anganwadi system was established as part of the Integrated as Child Development Service (ICDS) programme , which has since been renamed Saksham Anganwadi and Poshan 2.0.
- Under the MoWCD, the Anganwadi Services Scheme is a centrally sponsored programme.
- It stands for one of the biggest and most distinctive early childhood care and development projects in the entire globe.
- Objectives: The program's objectives are to enhance the nutritional and physical health of young children (0–6 years), expectant mothers, and nursing mothers, as well as to lower the occurrences of mortality, morbidity, and malnutrition.
- System Depth: Through Anganwadi Centres (AWCs), Anganwadi Workers (AWWs), and Anganwadi Helpers (AWHs), the system provides services to 906.17 lakh beneficiaries.
- NATIONAL FAMILY HEALTH SURVEY-5 (NFHS) REPORT: NFHS-5 was released by the Ministry of Health and Family Welfare (MoHFW).
- Objective: To deliver accurate and comparable data on various topics, such as family welfare and health.
- The NFHS-5's scope is broadened by the inclusion of new dimensions like death registration, pre-school instruction, enlarged child immunisation areas, menstrual hygiene, etc.
| Indicators | Findings |
| Total fertility rate, average number of children per woman | declined from 2.2 to 2.0 |
| Institutional births | increased from nd in areas around births being delivered in institutions and in urban areas. |
| Fully immunized | more months, compared with 62% in NFHS-4. |
| Level of stunting |
|
| prevalence of overweight or obesity | increased from among and . |
RIGHT TO HEALTH IN INDIA
- Provisions in Constitution:
- Article 21: This article of the Constitution guarantees the right to life and personal liberty, which has been interpreted by the courts to include the Right to Health .
- DPSP: Part IV of the Constitution under the Directive Principles of State Policy (DPSP) (Articles 38, 39, 42, 43, & 47) ensures social and economic justice to its citizens directly or indirectly relating to public policy in terms of health putting the obligation on the state to ensure the effective realization of the Right to Health.
- Judicial Activism:
- Supreme Court in Paschim Banga Khet Mazdoor Samity case (1996) held that the primary duty of the government is to secure the welfare of the people being an obligation of the government to provide adequate medical facilities for its people in a welfare state.
- Supreme Court had ruled that every doctor whether at a government hospital or otherwise has the professional obligation to extend his services with due expertise for protecting life in Parmanand Katara Vs Union of India (1989) .
- Human Dignity: The right to health is an essential component of human dignity and should be protected and promoted for all individuals, regardless of their gender, race, ethnicity, religion, or socioeconomic status.
- International Conventions: India is a signatory of the Article 25 of the Universal Declaration of Human Rights (1948) by the United Nations that grants the right to a standard of living adequate for the health and well-being to humans including food, clothing, housing and medical care and necessary social services.
Need of RTH in India
- Privilege to few: The right to equality guaranteed under Article 15 upholds non-discrimination on the basis religion, race, caste, gender, place of birth, etc. still the dismal investment in public health for decades has made healthcare a privilege available to a few.
- Break Discriminatory Structure: Right to health is critical to breaking discriminatory structures that will otherwise continue to perpetuate inequality in all spheres of life, including education, opportunity, wealth, and social mobility.
- Article 21’s Interpretation: The judicial interpretation of the right to life and liberty under Article 21 in several judgments as inclusive of health was crucial.
- As the universal access to healthcare is now as achievable as it is indispensable.
- Progressive Rights of the people: The rights of people are not stagnant, and must evolve as the country evolves.
- Service-Delivery Model: Ayushman Bharat is an ambitious scheme with great potential, but there is a difference between a right and a service-delivery model of development.
- Lack of Efficiency in healthcare: Healthcare facilities across the country lacks different levels of efficiency and sufficiency which can be outdone RTH.
- Dismal Primary Health Sector: RTH will help in developing the root of the healthcare sector i.e., the primary healthcare sector that lacks proper guidance and implementation of policies which makes people disbelieve in healthcare sector in India.
Arguments against RTH
- Due to the lack of clarity over who will be responsible for paying for the required free emergency treatment, private healthcare providers have been the most vocal opponents of the RTH.
- Critics claim that it is an attempt to surrender the State's duty to provide health protection and increases the burden of patients on the private sector.
- Many believe that the RTH will be unnecessary and highly restrictive.
- Without development or improvisation of the present structure of the healthcare facilities, implementing RTH will be devastating for already stressed medical field in India.
Challenges Related to Right to Health in India
- Inadequate Healthcare Infrastructure: India's healthcare infrastructure remains inadequate, particularly in rural areas where the 73% of the Indian population lack even basic medical facilities.
- Burden of schemes : Doctors are protesting against the RTH because they question the need for it when there are already schemes like Chiranjeevi that cover most of the population.
- Specialization concerns : They are also objecting to certain clauses, such as defining “emergency” and being compelled to treat patients outside their specialty as part of an emergency.
- High Disease Burden: India has a high burden of communicable and non-communicable diseases which requires significant investment in healthcare infrastructure and resources.
- Frontiers in Public Health Report: More than 33% of the individuals are still suffering from infectious diseases out of the total ailing population in India.
- Gender Inequalities: Women in India face significant health disparities.
- World Economic Forum 2021: India consistently ranks among the five worst countries in the world for the health and survival of females.
- Health Financing: Low levels of public spending on healthcare limits the government's ability to invest in healthcare infrastructure and resources, leading to inadequate healthcare services for individuals.
- Government of India spent 2.1% of GDP on healthcare in FY23 which is lower than the average health spending share of the GDP — at around 5.2% — of the Lower- and Middle-Income Countries (LMIC).
- No detailing of the process : To the charge that there is no detailing of the process, health rights activists have pointed out that it would be a function of the Rules, not the law itself.
- Concerns pertaining to compensation: Healthcare providers have a problem with reimbursement delays. Additionally, there are complaints that the predetermined package rates for various medical procedures and treatments are not sufficiently profitable or do not cover the actual cost.
Government Initiative in tackling the Challenges
- Implementing Universal Health Coverage: As a critical indicator for human equity, security and dignity UHC makes sure that all people have access to the health services they need without the risk of financial hardship when paying for them.
- Health accessibility and affordability : A crucial healthcare problem even in the 21st century prompted World Health Organization to choose “Universal Health Coverage” as the theme for World Health Day 2019.
- India started working towards the universal problem of affordability and accessibility with the introduction of Ayushman Bharat.
Significance of UHC:
- Universal health coverage has a direct impact on a population’s health and welfare.
- Access and use of health services enables people to be more productive and active contributors to their families and communities.
- Financial risk protection prevents people from being pushed into poverty when they have to pay for health services out of their own pockets.
- Universal health coverage is a critical component of sustainable development and poverty reduction, and a key element of any effort to reduce social inequities.
- Universal coverage is the hallmark of a government’s commitment to improve the wellbeing of all its citizens.
Issues and Challenges related to UHC
- Lack of Funds: Public sector is severely underfunded.
- Unaffordable Healthcare: Private sector is witnessing a high-cost healthcare service which is problematic.
- Regulation: Ineffective regulation is a concerned area.
- Poor Health Education: Lack of education and awareness regarding healthy lifestyles and preventive health measures can lead to an increase in preventable illnesses and conditions.
Government Steps for implementing UHC in Healthcare sector
- National Health Policy (NHP) 2017 : Allocating resources of up to two-thirds or more to primary care for achieving “the highest possible level of good health and well-being, through a preventive and promotive healthcare orientation”.
- A 167% increase in allocation for the Pradhan Mantri Jan Arogya Yojana (PMJAY) — the insurance programme which aims to cover 10 crore poor families for hospitalisation expenses of up to ?5 lakh per family per annum.
- The government’s steps to incentivise the private sector to open hospitals in Tier II and Tier III cities.
- Individual states are adopting technology to support health-insurance schemes. Example: Remedinet Technology (India’s first completely electronic cashless health insurance claims processing network) has been signed on as the technology partner for the Karnataka Government’s recently announced cashless health insurance schemes.
National Health Policy
National Health Policy: National Health Policy is an initiative by the Central Government to strengthen the health system in India covering various dimensions of health sectors like disease prevention, promotion of good health via cross-sectoral actions, health investment, strengthening human resources, technological advancements and more.
Launched in 2017 by the Central Government, has introduced four significant goals:
- Changing health priorities : Aims to tackle the increasing non- communicable and infectious diseases in India.
- Growth of the health care industry : Strengthen the health care industry by introducing technological advancement.
- Lower the expenditure : Aims to reduce medical expenses and provide superior services to poor and backward communities.
- Economic growth : Aims to enhance fiscal capacity by boosting economic growth.
Objectives of National Health Policy
- Basic Structure: National Health Policy commits to integrity, highest professional standards and ethics integrating these functions in health care delivery services by maintaining transparency and a sustainable environment.
- Doing away Disparities: Aims to offer superior health services to every age group and gender.
- Universal Healthcare Services: Focuses on providing universal access to excellent quality health care services at an affordable price preventing regional disparities.
- Reducing Mortality Rate: Aims to reduce premature mortality from cancer, cardiovascular diseases, chronic respiratory diseases, and diabetes by 25% within 2025.
- Recognises the importance of sustainable development and time-bound quantitative goals.
- Developing Overall Health Structure: Aims to improve overall health structure through promotive, palliative, and rehabilitative services.
Drawbacks of the policy
- Repetition of Ideas: The new policy repeats several old ideas, and fails to fulfil 2015 promise of a Right to Health.
- It fails to make health a justiciable right in the way the Right to Education 2005 did for school education.
- Assurance-based Approach: The policies reference to an “assurance-based approach” abandons a radical change proposed in the draft policy of 2015 where National Health Rights Act aimed at making health a right.
- Disagreement with States: Health Ministry officials said the idea was dropped because state governments felt that health infrastructure was not yet at levels at which health could be made an entitlement, and the citizen could theoretically take a government to court for its denial.
- Diagnostics, drugs and essential health care services are already free in many states.
- Longevity in Implementation: The policy says that 2.5% GDP spend target for Health would be met by 2025 but the HLEG report of 2011, quoted by the 12th Plan document, had set the same target for the Plan that ends at the end of this march 2017.
- Health Cess: A health cess was a pathbreaking idea in the Health Ministry’s draft policy but now it has been rejected, with health officials maintaining that there is no dearth of funds.
WAY FORWARD:
- Increase Public Investment in Healthcare : The government should increase the budgetary spending on healthcare and allocate more resources to build a strong healthcare infrastructure.
- Enhancement of Health Expenditure: Health Expenditure which currently stands lower than most of the developing nations needs to be enhanced as a percentage of GDP .
- Prioritize Primary Sector: Strengthening the primary healthcare sector should be the priority.
- Expand Health Insurance Coverage: Expanding the health insurance coverage to all citizens would help reducing out-of-pocket expenses and make healthcare more affordable.
- Improve Healthcare Quality: The government should invest in improving the quality of care by developing quality standards, ensuring adherence to these standards, and providing training to healthcare providers.
- Invest in Health Information Systems: Priority should to given to develop robust health information systems that can provide timely and accurate data.
- Promote Preventive Healthcare: Focusing on preventive healthcare can reduce the burden of disease and the cost of healthcare.
Drug regulation in India:
India, has been mulling the creation of a mandatory recall law for substandard drugs since 1976, and yet no law exists that mandates such medicine be removed from the market to this day.
- In 1976, the Drugs Consultative Committee (DCC), which consists of all the state drug controllers along with senior bureaucrats from the Ministry of Health and the national drug regulator, the Central Drug Standard Control Organisation (CDSCO), discussed the issue of drug recalls.
- The issue of recalls came up again in meetings of the DCC in 1989, 1996, 1998, 2004, 2007, and 2011 but none of them resulted in amendments to the Drugs & Cosmetics Act to create a mandatory recall mechanism.
- Why has this issue been pending for so long in India with no redress?
- the Drug Regulation Section of the Union health ministry is simply not up to the task of tackling complex drug regulatory issues
- combination of different factors including apathy, lack of expertise in the area, and a greater interest in enabling the growth of the pharmaceutical industry than protecting public health.
- India’s highly fragmented regulatory structure , with each state having its own drug regulator.
- India’s drug regulators are aware of the fact that a mandatory drug recall system, which necessarily has to be centred on a system of wide publicity, will bring to public attention to the rotten state of affairs in India’s pharmaceutical industry.
- Dozens of drugs fail random-testing in government laboratories . Ideally, these drugs will be mandatorily recalled in a transparent manner, with the people being informed of the failures.
- Liberal punishments: Guidelines were first published by the Drugs Consultative Committee in 1993 and again in 2010. According to these recommendations, harassing medication makers would result from prosecuting every instance of inferior drugs. Therefore, the committee was established to carefully punish the producers.

- The Union Health Ministry recently published a new draft Bi ll to replace the antiquated Drugs and Cosmetics Act, 1940.
- To create an effective recall mechanism, the responsibility of recalling drugs has to be centralised, with one authority that has the legal power to hold companies liable for failures to recall drugs from across the country.
- If India is a single market for drugs, it follows that it should have one regulator.
- The Drug and Cosmetics Act, 1940 : imposes regulatory restrictions on the in-country production, distribution, and sale of medicines and cosmetics. The Act designates the sale of subpar medications as a serious violation since these medications have the potential to cause patients harm. A jail sentence or fine may be issued in accordance with this Act.
- Amend the Drugs and Cosmetics Act: The medications and Cosmetics Act's main objective is to prevent inferior medications from entering the market in the first place rather than to react to them after the fact. Therefore, the DCA must be changed to stop the production of inferior pharmaceuticals in the first place.
- Good Manufacturing Practices: Manufacturers ought to implement a rigorous system of quality control. Simple checks and balances must be followed, such as checking raw materials before incorporating them into drugs, purchasing raw materials from authorised producers, keeping equipment clean, etc. Any time there is a quality issue, a root cause analysis should be carried out right away.
Zero Tolerance to Drugs
The Centre has adopted a zero-tolerance policy towards narcotics
- According to the 2019 National Survey on Extent and Pattern of Substance Use in India, 2.26 crore people, or roughly 2.1% of the population, use opioids.
- Additionally, same poll revealed that 31 million Indians, or 2.8% of the population, used cannabis for bhang, ganja and charas.
- Drug abuse has increased as a result of the breakdown of the united family system, a reduction in religious and moral values, and other factors, such as the desire to escape the harsh reality of life.
- Peer pressure: Many young people begin using drugs as a result of peer pressure from friends, teachers, or other members of their informal social networks.
- Easy Accessibility — India is positioned in such a way that the "Golden Triangle" and the "Golden Crescent" are to its east and west, respectively.
Initiatives:
- The MHA established the Narcos Coordination Centre (NCORD) system in 2016 to ensure efficient drug law enforcement.
- The portal serves as an efficient method for exchanging information amongst various institutions and authorities.
- The minister added that the Supreme Court is discussing the creation of fast-track courts and exclusive courts for the expeditious trial of drug cases.
Way Forward:
India could reduce the treatment gap for mental disorders, increase the number of personnel in the mental health sector, work towards reducing discriminatory attitudes, and devise an integrated approach for detecting, treating, and managing patient needs.
- Corporate Social Responsibility (CSR) should be encouraged in the field of mental health.
Mental Health
Mental health issues are a major health challenge in the world today. According to the World Health Organization (WHO), there is a 10-25-year life expectancy reduction in patients with severe mental disorders. About 72% of member states had a standalone policy or plan for mental health in 2017.
- India introduced the National Mental Health Policy (NMHP) in 2014, and a rights-based Mental Healthcare Act in 2017, which replaced the Mental Healthcare Act of 1987.
- The NMHP, National Health Mission, National Adolescent Health Programme, and Ayushman Bharat have the necessary components to address the mental health issues of all sections of the population.
Issues and Challenges
- The share of mental hospitals per 1,00,000 population is as low as 0.01 in line with developing countries, according to the WHO.
- India was at the 99th position in the distribution of mental health outpatient facilities (per 1,00,000 population), with 0.18 units per 1,00,000 population.
- India was also at the 64th position in the distribution of mental health day treatment facilities
- The distribution of community residential facilities globally for the median year 2016 showed India at the 58th position, with 0.017 units per 1,00,000 population among the WHO member countries.
- Mental Illness: Mental illnesses include anxiety disorders, psychotic disorders, mood disorders, substance use disorders, personality disorders and eating disorders.
- The suicide rate was 10.6 per 1,00,000 population whereas in India, it was 16.3 per 1,00,000 in 2016.
- The suicide rate was higher among males compared to females.
- Mental health facilities: There are also challenges regarding funding, delivery of mental health packages, lack of trained staff, etc.

- Mental Healthcare Act, 2017
- The Act ensures healthcare for people suffering from mental illness through health services funded by the Government. It decriminalises suicide, disallows sterilisation.
- As part of Section 19, the government was made responsible for creating opportunities to access less restrictive options for community living — such as halfway homes, sheltered accommodations, rehab homes, and supported accommodation.
- Under the MHCA, all States are required to establish a State Mental Health Authority and Mental Health Review Boards (MHRBs) – bodies.
- While Ayushman Bharat allows for insurance for medical treatment of the mentally unwell, financial protection in the form of allowances should be initiated.
- National suicide Prevention Strategy: The Ministry of Health and Family Welfare’s recently published National Suicide Prevention Strategy fits right there.
- The most common reasons include family problems and illnesses, while other causes include marital conflicts, love affairs, bankruptcy, substance abuse and dependence .
- In India, more than one lakh lives are lost every year to suicide. In the past three years, the suicide rate has increased from 10.2 to 11.3 per 1,00,000 population.
- The Strategy also intends to write in mental health in the curriculum in educational institutions within the next eight years.
- It also lists interventions that have reduced the suicide rate in various sections in the country, including among students and rural groups, by limiting the availability of pesticides.
Answer our survey to get FREE CONTENT


Feel free to get in touch! We will get back to you shortly
- Privacy Policy
- Terms of Service
- Quality Enrichment Program (QEP)
- Intensive News Analysis (INA)
- Topper's UPSC PYQ Answer
- Essay Enrichment Program
- NEEV GS + CSAT Foundation
- News-CRUX-10
- Daily Headlines
- Geo. Optional Monthly Editorials
- Past Papers
- © Copyright 2024 - theIAShub
Talk To Our Counsellor
- Our Centers Delhi Bhubaneswar Lucknow
CURRENT AFFAIRS FOR UPSC IAS
Indian Health Sector: Opportunities and Challenges
Published: 10th Apr, 2021
In Budget 2021 health sector is focused on by Government, which was severely hit by the unprecedented pandemic. The focus has been laid on healthcare and infrastructure with an eye on achieving the vision of Atmanirbhar Bharat.
- The unprecedented COVID-19 pandemic has completely changed the situation no one could ever imagine. Almost all aspects of society have witnessed disruptions.
- However, every challenge comes with various opportunities, so does this pandemic.
- It has opened a wide window of opportunities to restructure and reform the Indian health industry which has been in a bad state of repair.
- Underscoring the significant importance of health and wellbeing for the growth and development of the country, the Budget allocation for the same was increased to ?2,23,846 crore in 2021-22 as against this year's ?94,452 crores, according to an official release.
- This manifests into an increase of 137%.
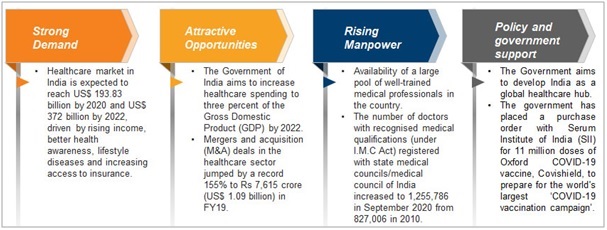
Assessing Indian Healthcare Industry
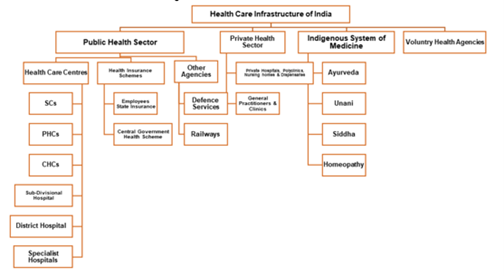
- In India, the Health care sector is one of the largest sectors in terms of both revenue and employment.
- Public health care hospitals comprise secondary and tertiary care institutions in urban areas while primary basic facilities are focused in rural areas.
- Private health care sectors provide secondary, tertiary, and quaternary services in metro cities.
Healthcare Industry in India
What are the issues and concerns of the Sector?
India’s health care sector has achieved some positive achievements on the health indicators but suffers some serious shortcomings in care delivery.
| contain provisions regarding Health. |
- Inadequate reach: The inadequate reach of basic healthcare services, shortage of medical personnel, quality assurance, the inadequate outlay for health, and most importantly insufficient impetus to research.
- Inadequate Fund: The inadequate fund allocation by the administrations is one of the grave concerns.
- Optimal Insurance: The concept of health insurance is still not clear in India and the market is still virgin.
- No focus on Preventive Care : In India, there is a very low emphasis on preventive care, which can be proved very effective in solving a lot of problems for the patient in terms of misery or financial losses.
- Less emphasis on Medical Research: In India, there is no much impetus is being given to R&D and cutting-edge technology-led new initiatives. Such technologies could be useful in an unprecedented situation like Covid-19.
- Issue of Policymaking: For providing effective and efficient healthcare services policymaking is certainly an important aspect. In India, the problem is fundamental of supply than demand, where policymaking can be effective.
- Shortage of Medical Workforce: In India, there is a shortage of doctors, nurses, and other staff in the health sector. As per a report laid down by a minister in Parliament, there is a shortage of 600,000 doctors in India.
- Inadequate outlay for health: As per National Health Policy 2002, India contributes only 0.9 percent of its GDP to the Health care sector.
- Lack of structure: Private hospitals are expensive and public hospitals are either not enough for the Indian Population or lack the basic facilities.
Opportunities in Health Care Sector
- Indian health care sector is expected to increase to Rs. 8.6 trillion (US$ 133.44 billion) by 2022. It is almost three times which is what it’s now in present.
- Data Analytics: With the arrival of the National Digital Health Mission (NDHM), the digital Health ID will come which will store the data of patients. It would help in effective policymaking and private players can get an edge in introducing the new technologies in the market.
|
|
- Employment opportunity: As we know Indian health care sector lacks a workforce, there is a space for thousands of employees.
- Start-ups: With the help of Government and private players an environment of start-ups and entrepreneurship can be created in this field.
- Medical Tourism: India is already one of the favorite medical Tourism Destinations in the world and in the upcoming years this sector can be harnessed efficiently.
| In December 2020, a new COVID-19 vaccine delivery digital platform called 'CO-WIN' is being prepared to deliver vaccines. In Union Budget 2020 21, Rs. 35,600 crore (US$ 5.09 billion) has been allocated for nutrition-related programs. outlay announced for the health sector that is inclusive of Rs. 6,400 crore (US$ 915.72 million) for PMJAY in Union Budget 2020–21. Over the last decade, the Government has been silently working on translating the SDH framework into practice, with key interventions in the areas of: ) ) ) ) ) |
What measures are required in the sector?
- Improving infrastructure: There is a need of improvising the infrastructure of public hospitals which have a lot of burden due to the high population in India.
- Focus on private hospitals: Private hospitals must be encouraged by the government because their contribution is important. Private sector also needs to participate because the challenges are significant and these cannot be resolved only by the government alone.
- Efficiency enhancement: More medical personnel must be recruited to enhance the capabilities and efficiency of the sector.
- Technology utilisation: Technologies must be used to connect the dots in the health system. Medical devices in hospitals/ clinics, mobile care applications, wearables, and sensors are some forms of technology that should be added in this sector.
- Awareness: People should be made aware of early detection and preventive care. It would help them in saving pocket expenditure also.
The year 2021 could be the year when India consolidates and expands on its social determinants of health (SDH) approach. India now needs to sustain its current interest in strategic health policy as a key pillar of the economy.
More Articles

Verifying, please be patient.
Our Centers
DELHI (Karol Bagh)
GS SCORE, 1B, Second Floor, Pusa Road, Karol Bagh, New Delhi - 110005 (Beside Karol Bagh Metro Station Gate No. 8)
Get directions on Google Maps
BHUBANESWAR (Jaydev Vihar)
GS SCORE, Plot No.2298, Jaydev Vihar Square, Near HCG Day Care, BBSR - 751013
LUCKNOW (Aliganj)
GS SCORE, 2nd Floor, B-33, Sangam Chauraha, Sector H, Aliganj, Lucknow, UP - 226024
Delhi (Karol Bagh) Centre
GS SCORE, Second Floor, Metro Tower, 1B, Pusa Road, Karol Bagh, New Delhi - 110005 (Beside Karol Bagh Metro Station Gate No. 8)
Email: [email protected]
Phone: +91 8448496262
Classroom / online / Live programs
- Mains Classes
- Mains Advance Classes
- Ethics & Essay Classes
- IAS Foundation
- Aadhar:NCERT Foundation
- Target PT:Prelims Classes
- Current Affairs Mentorship Program
- Optional Classes
- Optional Q&A (TEST SERIES & Mentorship)
- Mains Previous Year Questions
TEST SERIES/ MENTORSHIP
- ITS:Integrated Test Series & Mentorship
- GS Mains Q&A (Mentorship & Test Series)
- GS Test Series
- Ethics & Essay Test Series
- Samarth - Mains Answer Writing
STUDY MATERIAL
- Prelims Study Material
- Mains Study Material
- Mains Answer Writing Workbook
- Meet the Mentor
- Terms & Conditions
- © 2024 - IAS SCORE
All Rights Reserved.
Welcome to our secure login portal. Access your account with ease.

- Using Password
Not registered yet? register here!
Welcome to our secure register portal. For a brighter future, register now and unlock endless learning opportunities.
User Register
Already have an account? Login
Oops, forgot your password? Don't worry, we've got you covered. Reset it here
Lost your login details? No problem! forgot your password in just a few clicks
Forgot Password
Verify your mobile number, you have successfully logged in.
Join Us on WhatsApp
General Studies
All Programmes
Study Material
No Articles Found.
Let’s find a better place for you to go..
© 2024 Vajiram & Ravi. All rights reserved
- TRP for UPSC Personality Test
- Interview Mentorship Programme – 2023
- Daily News & Analysis
- Daily Current Affairs Quiz
- Baba’s Explainer
- Dedicated TLP Portal
- 60 Day – Rapid Revision (RaRe) Series – 2024
- English Magazines
- Hindi Magazines
- Yojana & Kurukshetra Gist
- All India Prelims Test Series – 2025
- Gurukul Foundation
- Gurukul Foundation – Delhi
- Gurukul Advanced
- TLP Connect – 2025
- TLP (+) Plus – 2025
- Integrated Learning Program (ILP) – 2025
- MAINS PYQs Mastery
- TLP Plus – 2024
- Sociology Foundation Course – 2025
- Sociology Test Series – 2024 (Coming Soon!)
- Public Administration FC – 2024
- Anthropology Foundation Course
- Anthropology Optional Test Series (Coming Soon!)
- Geography Optional Foundation Course
- Geography Optional Test Series – Coming Soon!
- PSIR Foundation Course
- PSIR Test Series – Coming Soon
- KPSC ಪಶುವೈದ್ಯಾಧಿಕಾರಿ (Veterinary Medical Officer – VMO) Exam 2024
- ‘Mission ಸಂಕಲ್ಪ’ – KPSC Foundation Course
- ‘Mission ಸಂಕಲ್ಪ’ – KPSC Prelims Crash Course
- Daily News & Analysis हिन्दी
- Monthly Magazine
India’s Health Sector
- March 6, 2023

Context : Recently the Government of India and World Bank signed two complimentary loans worth $1 billion to support and enhance India’s healthcare infrastructure.
About India’s healthcare sector at glance:
- In the Economic Survey of 2022 , India’s public expenditure on healthcare stood at 1% of GDP in 2021-22 against 1.8% in 2020-21 and 1.3% in 2019-20.
- India had 7 physicians per 1,00,000 people in 2017 (in contrast to 98 in Pakistan, 100 in Sri Lanka and 241 in Japan).
- 53 beds per 1,00,000 people (in contrast to 63 in Pakistan, 79.5 in Bangladesh, 415 in Sri Lanka and 1,298 in Japan).
- 7 nurses and midwives per 1,00,000 people (in contrast to 220 in Sri Lanka, 40 in Bangladesh, 70 in Pakistan, and 1,220 in Japan).
- India has among the highest out-of-pocket (OOP) expenditures of all countries in the world- 62% of the total health expenditure in India is OOP.
- According to the World Health Organization (WHO), India ranks 184 out of 191 countries in health spending.
- The US spends over 16% of its total GDP on healthcare , while Japan, Canada, Germany etc. spend over 10% of their GDP on healthcare.
Health Index for states developed by Niti Aayog:
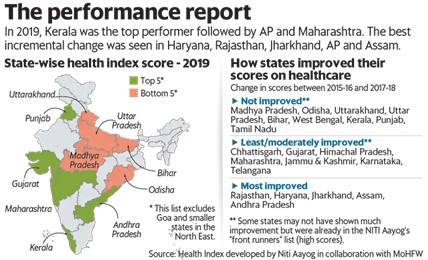
- The Health Index for States developed by Niti Aayog in consultation with the health ministry and the World Bank has rankings for large states, smaller states and Union territories.
- It is based on 23 health parameters ranging from mortality rate and sex ratio to functioning cardiac care units.
- In 2019, Kerala was the top performer followed by Andhra Pradesh and Maharashtra.
- The index results indicated that states even with a lower economic output are performing better on health and well-being.
Challenges associated with India’s healthcare sector:
- Low Budget Spending : India’s public expenditure on healthcare is only 2.1% of GDP in 2021-22 while Japan, Canada and France spend about 10% of their GDP on public healthcare.
- Unequal distribution: India’s health care system is concentrated in urban areas with very little presence in the rural areas where majority of the population lives.
- Lack of Medical Research : In India, R&D and cutting-edge technology-led new projects receive little attention.
- Low doctor-patient ratio: The doctor patient ratio in India is about 1:1500 much higher than the WHO norm of one doctor for every 1,000 people.
- The private sector also provides for 58 percent of the hospitals and 81 percent of the doctors in India.
Govt of India Initiatives to improve healthcare sector in the country :
- Pradhan Mantri-Ayushman Bharat Health Infrastructure Mission (PM-ABHIM) : it aims to strengthen India’s health infrastructure and improve the country’s primary, secondary and tertiary care services.
- Ayushman Bharat : Follows a two- pronged approach by Creation of health and wellness centres to bring health care closer to homes.
- formulation of a Pradhan Mantri Jan Arogya Yojana (PMJAY) to protect poor and vulnerable families against financial risk arising out of health episodes.
- Ayushman Bharat Digital Mission: aims to connect the digital health solutions of hospitals across the country. Under this, every citizen will now get a digital health ID and their health record will be digitally protected.
- National Ayush Mission : it is a centrally sponsored scheme for the development of traditional medicines
- Pradhan Mantri Swasthya Suraksha Yojana (PMSSY) :aims to correct regional imbalances in the availability of affordable/reliable tertiary healthcare services and also to augment facilities for quality medical education in the country.
Way Forward:
There is an urgency to focus on all the three levels of primary, secondary and tertiary healthcare, it is imperative that the government look towards improving primary health care as a public good.
The lesson emerging most unequivocally from the pandemic experience is that if India does not want a repeat of the immeasurable suffering and the social and economic loss, we need to make public health a central focus.
There is also a need to declutter policy dialogue and provide clarity to the nomenclatures. India needs to move beyond the doctor-led system and Para medicalise several functions. India should focus on technology upgradation and preventive care to further its march towards healthy India.
Source: The Hindu
Previous Year Questions
Q.1) Consider the following:
- Aarogya Setu
Which of the above are built on top of open-source digital platforms? (2022)
- 1 and 2 only
- 2, 3 and 4 only
- 1, 3 and 4 only
- 1, 2, 3 and 4
Q.2) With reference to recent developments regarding ‘Recombinant vector Vaccines’, consider the following statements:
- Genetic engineering is applied in the development of these vaccines.
- Bacteria and viruses are used as vectors.
Which of the statements given above is/are correct? (2021)
- Both 1 and 2
- Neither 1 nor 2
Related Posts :
Rupee appreciation and depreciation, indian tea industry.
Enter your email address to subscribe to this blog and receive notifications of new posts by email.
Email Address
- UPSC Quiz – 2024 : IASbaba’s Daily Current Affairs Quiz 16th September 2024
- DAILY CURRENT AFFAIRS IAS हिन्दी | UPSC प्रारंभिक एवं मुख्य परीक्षा –14th September 2024
- DAILY CURRENT AFFAIRS IAS | UPSC Prelims and Mains Exam – 14th September 2024
- UPSC Quiz – 2024 : IASbaba’s Daily Current Affairs Quiz 14th September 2024
- DAILY CURRENT AFFAIRS IAS हिन्दी | UPSC प्रारंभिक एवं मुख्य परीक्षा –13th September 2024
- DAILY CURRENT AFFAIRS IAS | UPSC Prelims and Mains Exam – 13th September 2024
- UPSC Quiz – 2024 : IASbaba’s Daily Current Affairs Quiz 13th September 2024
- DAILY CURRENT AFFAIRS IAS हिन्दी | UPSC प्रारंभिक एवं मुख्य परीक्षा –12th September 2024
- DAILY CURRENT AFFAIRS IAS | UPSC Prelims and Mains Exam – 12th September 2024
- UPSC Quiz – 2024 : IASbaba’s Daily Current Affairs Quiz 12th September 2024
Search now.....
Sign up to receive regular updates.
Sign Up Now !

- Our Selections
- About NEXT IAS
- Director’s Desk
- Advisory Panel
- Faculty Panel
- General Studies Courses
- Optional Courses
- Interview Guidance Program
- Postal Courses
- Prelims Test Series
- Mains Test Series (GS & Optional)
- ANUBHAV (All India Open Mock Test)
Daily Current Affairs
- Current Affairs MCQ
- Monthly Current Affairs Magazine
- Previous Year Papers
- Down to Earth
- Kurukshetra
- Union Budget
- Economic Survey
- Download NCERTs
- NIOS Study Material
- Beyond Classroom
- Toppers’ Copies
- Student Portal
Healthcare Sector in India
Syllabus: GS2/Health/GS3/Indian Economy
- Credit rating agency ICRA has released a research report on the Indian hospital industry.
Key Highlights of the Report
- Post Covid, the government healthcare expenditure has increased from 1.2-1.4 percent to 1.6-2.2 percent of GDP.
- Average revenue per occupied bed day (ARPOB) increased from ₹34,277 to ₹49,836 during FY20-H1 FY24.
- India has one of the lowest per capita bed counts in the world.
Healthcare Sector of India
- Healthcare Sector: It comprises hospitals, medical devices, clinical trials, outsourcing, telemedicine, medical tourism, health insurance and medical equipment.
- India’s healthcare delivery system is categorised into two major components – public and private.
- Public Sector: It comprises limited secondary and tertiary care institutions in key cities and focuses on providing basic healthcare facilities in the form of Primary Healthcare Centers (PHCs) in rural areas.
- Private Sector: The private sector provides the majority of secondary, tertiary, and quaternary care institutions with a major concentration in metros, tier-I, and tier-II cities.
- Medical Tourism: India ranks 10th in Medical Tourism Index (MTI) for 2020-2021 out of 46 destinations in the world.
- The Indian medical tourism market was valued at US$ 2.89 billion in 2020 and is expected to reach US$ 13.42 billion by 2026.
Major Challenges Faced by Healthcare Sector in India:
- The government mandated that private medical colleges must be built on at least five acres of land hence, they were built in rural areas, where there was a lack of adequately qualified, full-time doctors due to living conditions, besides low pay scales.
- The National Medical Commission (NMC) has put forward the idea to do away with the requirement of minimum five acres of land.
- The doctor-to-patient ratio remains low, which is merely 0.7 doctors per 1,000 people whereas the World Health Organisation (WHO) average is 2.5 doctors per 1,000 people.
- Aging population and the associated increase in chronic diseases add to the healthcare burden.
- High out-of-pocket Expenditure: While public hospitals offer free health services, these facilities are understaffed, poorly equipped, and located mainly in urban areas leaving no alternatives but to access private institutions and incurring high out-of-pocket expenses in healthcare.
- Every year, roughly 5.8 million Indians die from heart and lung diseases, stroke, cancer and diabetes.
- Shortage of hygiene infrastructure, lack of awareness, limited access to facilities, lack of trained medical personnel, dearth of medicines and good doctors are the challenges faced by more than 70 percent of India’s population living in rural areas.
- Ensuring that the private healthcare sector serves the larger public health goals.
Measures Needed for India to become Global Healthcare Provider:
- India spends the least among BRICS countries: Brazil spends the most (9.2%), followed by South Africa (8.1%), Russia (5.3%), China (5%).
- Infrastructure Development: Invest in building and upgrading healthcare infrastructure, including hospitals, clinics, and research facilities.
- Healthcare Education and Training: Strengthen medical education and training programs to produce skilled healthcare professionals.
- Research and Innovation: Foster a culture of research and innovation in healthcare. Provide incentives for pharmaceutical and biotech companies to conduct research and develop new treatments.
- Telemedicine and Digital Health: Promote the use of telemedicine and digital health solutions to increase access to healthcare services, especially in rural areas.
- Ensure a transparent and efficient regulatory framework.
- Public-Private Partnerships (PPPs): Encourage collaborations between the government, private sector, and non-profit organizations to leverage resources and expertise.
- Develop innovative financing models to fund healthcare projects and initiatives.
- Disease Prevention and Health Promotion: Focus on preventive healthcare measures to reduce the burden of diseases.
- Encourage healthcare facilities to obtain international accreditation to enhance their credibility.
- Improve visa and travel infrastructure to attract patients from other countries.
Recent steps Taken by the Government for the Growth of Healthcare Sector
- National Digital Health Mission (NDHM): Launched in 2020, NDHM aims to create a digital health ecosystem, including health IDs for citizens and the establishment of a national digital health infrastructure.
- Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY): AB-PMJAY, launched in 2018, is a national health protection scheme that provides financial protection to over 100 million families for secondary and tertiary care hospitalization.
- National Health Policy 2017: The National Health Policy outlines the government’s vision to achieve the highest possible level of health and well-being for all and emphasizes preventive and promotive healthcare.
- Health and Wellness Centers (HWCs): The government is working towards transforming primary health centers into HWCs to provide comprehensive primary healthcare services, including preventive and promotive care.
- Pradhan Mantri Swasthya Suraksha Yojana (PMSSY): PMSSY aims to enhance tertiary care capacities and strengthen medical education in the country by setting up new AIIMS (All India Institutes of Medical Sciences) institutions and upgrading existing government medical colleges.
- Research and Development Initiatives: The government has been encouraging research and development in healthcare, including support for the development of vaccines, drugs, and medical technologies.
- National Medical Commission (NMC) Act: The NMC Act, passed in 2019, aims to bring reforms in medical education and practice by replacing the Medical Council of India (MCI) and promoting transparency and accountability.
- Jan Aushadhi Scheme: The Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP) aims to provide quality generic medicines at affordable prices through Jan Aushadhi Kendras.
- There is a need to adopt technology wherever possible to streamline the operational and clinical processes for healthcare facilities in order to manage efficient patient flow.
- In addition, there is the challenge to think beyond the obvious and promote virtual care protocols, and telehealth services, which can be leveraged to reduce the patient-load burden to a large extent.
- To sum it up, there is an urgency to make healthcare service and service providers more transparent operationally.
- This will help ensure people and processes can be made easily accountable to provide better healthcare services.
- News In Short-14-09-2024
- Issue of Manpower Shortages in Indian Railways
- Modification of Scheme of Budgetary Support for Hydro Electric Projects
- Delay in Appointment of NHRC Chairperson
- NITI Aayog on Future Pandemic Preparedness
Headlines of the Day
- Headlines of the Day 16-09-2024
- Headlines of the Day 14-09-2024
- Headlines of the Day 13-09-2024
- Headlines of the Day 12-09-2024
- Headlines of the Day 11-09-2024
Other News of the Day
- India’s Critical Mineral Mission and Africa’s Role
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
UPSC Coaching, Study Materials, and Mock Exams
Enroll in ClearIAS UPSC Coaching Join Now Log In
Call us: +91-9605741000
Indian Health Sector Problems: Can the National Health Policy 2017 Make a Change?
Last updated on August 18, 2024 by ClearIAS Team
The health sector in India faces numerous problems. With the new national health policy, the government aims to achieve better and more inclusive health standards for all. But can the National Health Policy 2017 make a change? This article is an analysis of the problems of the health sector, solutions, and new initiatives.
Table of Contents
A background study of the Indian health scenario

Indian Health Sector Data: Budget Spending and Insurance Levels
- The public expenditure on the health sector remains a dismal show of only around 1.4% of the GDP.
- The investment in health research has been low with a modest rate of 1% of the total public health expenditure.
- Insurance coverage remains low as per the latest NSSO reports over 80% of India’s population remains uncovered by any health insurance scheme.
- Under the centre-run Rashtriya Swyasthya Bima Abhiyan , only 13% of the rural and 12% of the urban population had access to insurance coverage.
- There has been a stark rise in out-of-pocket expenditure (6.9% in rural areas and 5.5% in urban areas – OOP in proportion to monthly expenditure). This led to an increasing number of households facing catastrophic expenditures due to health costs.
Indian Health Sector Data: IMR, MMR, Hunger, Non-Communicable diseases, and Mental Diseases
- India missed by close margins in achieving the millennium development goals of maternal mortality (India – 167, MDG – 139) and under 5 child mortality rate (India 49, MDG – 42). The rate of decrements in stillbirths and neonatal death cases has been slow.
- Nutrition status has been dismal and is one of the causes of child mortality and morbidity. As per the global hunger index (by IFPRI), India ranks 78th among 118 developing countries (with 15% of our population being undernourished; about 15% under-5 children who are ‘wasted’ while the share of children who are `stunted’ is a staggering 39% and the under-5 mortality rate is 4.8% in India.)
- While communicable diseases contribute 28% of the entire disease burden, non-communicable diseases (60%) show ample rise, and injuries at (12%) now constitute the bulk of the country’s disease burden.
- India ironically has to cater to two extreme healthcare situations. They are (1) one arising out of exclusions (out of poverty or lack of proper healthcare facilities) (2) while the other is lifestyle diseases like diabetes and cardiac-related problems.
- There has been a steady rise in mental illnesses in the country. According to a recent publication, one in every four women and 10% of men suffer from depression in India.
- At the same time, progress has been marked in the field of communicable diseases as such. Polio has been eradicated, leprosy has been curtailed and HIV – AIDS cases have met the MDG target of being reduced by half in number.
Indian Health Sector Data: Personnel Status
- Health workforce density in India remains low .
- India’s ratio of 7 doctors and 1.5 nurses per 1,000 people is dramatically lower than the WHO average of 2.5 doctors and nurses per 1,000 people .
- The majority of the health workforce is concentrated in urban areas.
- Furthermore, there is an acute shortage of paramedical and administrative professionals too.
Note: Taking cognizance of the prevailing situations, the Government of India has been aiming to improve the health system via various policies and initiatives. The latest National Health Policy, 2017 highlights the future aims and agendas of the government which can be summarised as follows:
What do we aim for in our current National Health policy?
The national health policy 2017.
The main objectives of the National Health Policy 2017 are as follows:
- To achieve Universal Health Coverage by assuring the availability of free, comprehensive primary health care services, ensuring improved access and affordability, of quality secondary and tertiary care, and achieving a significant reduction in out-of-pocket expenditure due to health care costs.
- To make a predictable, efficient, patient-centric, affordable, and effective health care system.
- Bringing in healthy and vital private sector contributions.
- By increasing public investment (raising it to 5% of the GDP ).
- To coordinate various non-health departments to improve the environment for health (by linking areas like – Swatch Bharath, balanced diet, reduced stress at the workplace, Yatri Suraksha, etc.).
- Incorporating health education as part of the curriculum, promoting hygiene and safe health practices within the school environs by acting as a site of primary health care, and promoting healthy practices via AYUSH and Yoga at workplaces and schools.
- Organizing public health care delivery.
- To enhance National health programs .
- Utilizing the potential of AYUSH and mainstreaming it.
- Improving women’s health and addressing gender violence. Initiatives like Janani Suraksha Yojana, new norms of addressing domestic violence, family planning programs,s, etc. can go a long way.
- Enhancing tertiary care services – via specialized consultative and intensive care facilities, tertiary services via advanced medical colleges, and health institutes.
- providing better health education
- incentivizing doctors for rural services
- enhancing nursing and other paramedical services
- developing and encouraging ASHA volunteers.
- Collaborating with non-governmental organizations and the private sector too –
- Train, and encourage skill development programs
- Utilise and direct Corporate social responsibility into health investments
- Encourage personnel training in mental health care and disaster management etc.
- Establishing a strong regulatory framework to include regulation of clinical establishments, professional and technical education, food safety, medical technologies, medical products, clinical trials, research, and implementation of other health-related laws.
- Involving and providing more role to local self-governments, bringing in decentralization and enhancing the accountability of government institutions to ensure effective efficient delivery of services.
Out of these the key and specific objectives remain to
Strengthen health system
- Increase Life Expectancy at birth from 67.5 to 70 by 2025.
- Establish regular tracking of the Disability Adjusted Life Years (DALY) Index as a measure of the burden of disease and its trends by major categories by 2022.
- Reduction of TFR to 2.1 at national and sub-national levels by 2025.
- Reduce under Five Mortality to 23 by 2025 and MMR from current levels to 100 by 2020.
- Reduce infant mortality rate to 28 by 2019.
- Reduce neonatal mortality to 16 and stillbirth rate to “single digit” by 2025.
- Achieve the global target of 2020 which is also termed as the target of 90:90:90 , for HIV/AIDS i. e,- 90% of all people living with HIV know their HIV status, – 90% of all people diagnosed with HIV infection receive sustained antiretroviral therapy and 90% of all people receiving antiretroviral therapy will have viral suppression.
- Achieve and maintain the elimination status of Leprosy by 2018 , Kala-Azar by 2017, and Lymphatic Filariasis in endemic pockets by 2017.
- To achieve and maintain a cure rate of >85% in new sputum-positive patients for TB and reduce the incidence of new cases, to reach elimination status by 2025.
- To reduce the prevalence of blindness to 0.25/ 1000 by 2025 and disease burden by one-third from current levels.
- To reduce premature mortality from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases by 25% by 2025.
Also read: Healthcare Sector in India
👉 Which year are YOU targeting for success in the IAS/IPS/IFS Exam? 🚀
(1) ⇒ UPSC 2025: Prelims cum Mains
(2) ⇒ UPSC 2026: Prelims cum Mains
(3) ⇒ UPSC 2027 Prelims cum Mains
Tip: Know more about ClearIAS Courses (Online/Offline)
Improve health system performance
- Increase utilization of public health facilities by 50% from current levels by 2025.
- More than 90% of the newborns are fully immunized by one year of age by 2025
- The relative reduction in the prevalence of current tobacco use by 15% by 2020 and 30% by 2025.
- Reduction of 40% in the prevalence of stunting of under-five children by 2025.
- Access to safe water and sanitation to all by 2020 (Swachh Bharat Mission).
- Reduction of occupational injury by half from current levels of 334 per lakh agricultural workers by 2020.
Enhance health status and program impact
- Increase health expenditure by the Government as a percentage of GDP from the existing 1.15% to 2.5 % by 2025.
- Ensure availability of paramedics and doctors as per the Indian Public Health Standard (IPHS) norm in high-priority districts by 2020.
- Establish primary and secondary care facilities as per norms in high-priority districts (population as well as time to reach norms) by 2025.
- Ensure district-level electronic database of information on health system components by 2020.
- Strengthen the health surveillance system and establish registries for diseases of public health importance by 2020.
Also read: Global Tobacco Epidemic
Major national programs in this sector
The following highlights of recent initiatives in this field showcase our renewed effort to achieve global standards.

National Health Mission
- This mission is targeting universal health care, to achieve IMR, MMR, TFR targets, family welfare, infrastructure maintenance, etc.
- The major components of the program are:
- RMNCH+A services – which stands for reproductive, maternal, newborn, child, and adolescent health care. Programs like Janani Suraksha Yojana, the program for adolescents like addressing the problem of anemia among adolescent girls and boys, etc.
- Communicable Diseases : The National Health Policy 2017 recognizes the interrelationship between communicable disease control programs and public health system strengthening . Different programs like the National Aids Control Program, National Leprosy Eradication Program, Revised Tuberculosis Control Program, and National Vector Borne Disease Control Program.
- Non-Communicable Diseases : The National Health Policy 2017 recognizes the need to halt and reverse the growing incidence of chronic diseases. Different programs through the involvement of AYUSH are taking forth to address these situations, for instance , Mission Madhumeha through Ayurveda is an example of efforts to address the issue of diabetes among people.
- Health system improvement at rural and urban levels.
- Universal Immunisation Programme – to provide life-saving vaccines to all children across the country free of cost to protect them against Tuberculosis, Diphtheria, Pertussis, Tetanus, Polio, Hepatitis B, Pneumonia and Meningitis, Measles, Rubella, Japanese Encephalitis (JE) and Rotavirus diarrhea. via Mission Indra Dhanush
- Mental Health : via new mental health policy.
Also read: Palliative Care in India
Other global initiatives in health involving India

International Vaccine Institute (IVI)
- India has taken full membership of the International Vaccine Institute.
- Initially a UNDP initiative, IVI began formal operations as an independent international organization, in Seoul, South Korea.
- It is devoted to developing and introducing new and improved vaccines to protect people, especially children, against deadly infectious diseases.
- The Institute has a unique mandate to work exclusively on vaccine development and introduction specifically for people in developing countries, with a focus on neglected diseases affecting these regions
- India has to contribute $50,000 annually to the institute.
The Global Promotion of the Traditional System of Medicines
- Ministry of AYUSH, the Government of India, and the World Health Organization (WHO) have signed a historic Project Collaboration Agreement (PCA) for the same.
- PCA is titled ‘Co-operation on promoting the quality, safety, and effectiveness of service provision in traditional and complementary medicine between WHO and AYUSH, India, 2016-2020’.
- It will help build and strengthen national capacities.
The Network to Improve Quality of Care for Mothers, Newborns, and Children
- India is among nine countries that will be part of a global health network focused on improving the quality of care for new mothers and babies and strengthening national efforts to end preventable deaths of pregnant women and newborns by 2030.
- The nine countries are India, Bangladesh, A Cote d’Ivoire, Ethiopia, Ghana, Malawi, Nigeria, Tanzania, and Uganda.
- The new ‘Network for Improving Quality of Care for Maternal, Newborn and Child Health’ is supported by the World Health Organisation (WHO), UN International Children’s Fund (Unicef) and other partners.
India and SDG Goal 3 Commitment
- India’s National Health Mission is making striding efforts in ensuring the goal of good health and well-being of the sustainable development goal.
- We have strengthened the implementation of the WHO framework convention on tobacco control
- To enhance the research and development of medicines for communicable and non-communicable diseases, provide access to essential medicines and vaccines in accordance with the Doha Declaration on TRIPS agreement and public health regarding flexibility to protect public health.
- We are aiming to increase our spending in this field and also strengthen institutions to target the achievement of the goal.
Also read: Anti-Microbial Resistance (AMR) and the Red Line Campaign
- Health plays a vital role in ensuring the rights of people and in facilitating social justice. A healthy and strong India can reap the best from the future world.
- Developments in the health sector enhance the human resource and also open avenues for revenue and employment generation.
- Digital Health: Latest developments
- Violence against healthcare workers (VAHCW) in India
Article by: Honey Mathew.

Best-Selling ClearIAS Courses
Upsc prelims cum mains (pcm) gs course: unbeatable batch 2025 (online), rs.75000 rs.29000, upsc prelims cum mains (pcm) gs course: ultimate batch 2025 (online), rs.95000 rs.49000, upsc prelims cum mains (pcm) gs course: ultimate batch 2026 (online), rs.115000 rs.59000, upsc prelims cum mains (pcm) gs course: ultimate batch 2027 (online), rs.125000 rs.69000.
About ClearIAS Team
ClearIAS is one of the most trusted learning platforms in India for UPSC preparation. Around 1 million aspirants learn from the ClearIAS every month.
Our courses and training methods are different from traditional coaching. We give special emphasis on smart work and personal mentorship. Many UPSC toppers thank ClearIAS for our role in their success.
Download the ClearIAS mobile apps now to supplement your self-study efforts with ClearIAS smart-study training.
Reader Interactions
June 23, 2017 at 7:12 am
This to notify that according to the above article under National Health Policy 2017 it is stated that the rise of public investment in health care would be of 5%. If you scroll two sections down in the ENHANCE HEALTH STATUS AND PROGRAMME IMPACT it is again mentioned that government spending will increase from 1.5% to 2.5% by 2025. This is slightly confusing and is not helping me understand which one to follow. Please help and its a request to clarify the above doubt.
July 10, 2017 at 11:52 pm
Good effort sir..thank you very much..
May 10, 2018 at 3:47 am
I think doctor nurse to patient ratio need correction….. please read the sentence
October 19, 2018 at 3:05 pm
Spreading awareness about non-communicable diseases like hypertension, diabetes. For all kind of disease treatments please visit online portal meddco.com which introduced affordable healthcare service packages
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Don’t lose out without playing the right game!
Follow the ClearIAS Prelims cum Mains (PCM) Integrated Approach.
Join ClearIAS PCM Course Now
UPSC Online Preparation
- Union Public Service Commission (UPSC)
- Indian Administrative Service (IAS)
- Indian Police Service (IPS)
- IAS Exam Eligibility
- UPSC Free Study Materials
- UPSC Exam Guidance
- UPSC Prelims Test Series
- UPSC Syllabus
- UPSC Online
- UPSC Prelims
- UPSC Interview
- UPSC Toppers
- UPSC Previous Year Qns
- UPSC Age Calculator
- UPSC Calendar 2025
- About ClearIAS
- ClearIAS Programs
- ClearIAS Fee Structure
- IAS Coaching
- UPSC Coaching
- UPSC Online Coaching
- ClearIAS Blog
- Important Updates
- Announcements
- Book Review
- ClearIAS App
- Work with us
- Advertise with us
- Privacy Policy
- Terms and Conditions
- Talk to Your Mentor
Featured on

and many more...
ClearIAS Programs: Admissions Open
Thank You 🙌
UPSC CSE 2025: On May 25, 2025
Subscribe ClearIAS YouTube Channel

Get free study materials. Don’t miss ClearIAS updates.
Subscribe Now
IAS/IPS/IFS Online Coaching: Target CSE 2025
Cover the entire syllabus of UPSC CSE Prelims and Mains systematically.

Issues with Mental Health and Mental Healthcare in India – Explained, pointwise
Current Affairs Classes Pre cum Mains 2025, Batch Starts: 11th September 2024 Click Here for more information
- 1 Introduction
- 2 What is the status of Mental Health in India?
- 3 What are the harmful effects of poor Mental Health?
- 4 What are the reasons for poor status of Mental Health in India?
- 5.1 Legal Measures
- 5.2 Schemes and Initiatives
- 6 What steps can be taken further?
- 7 Conclusion
| For Archives click → |
Introduction
Mental disorders are now among the top leading causes of health burden worldwide, with no evidence of global reduction since 1990. Suicides rates in India are amongst the highest when compared to other countries at the same socio-economic level. The latest survey by India’s National Institute of Mental Health and Neurosciences (NIMHANS) found that nearly 150 million Indians are in need of mental healthcare services, but fewer than 30 million are seeking care. This shows several issues with mental healthcare in India including access and social attitude to mental health. The Government has taken several initiatives to improve access to mental healthcare services in addition to gradually changing the discourse on mental health. However, as evident in the data, there is a need for further effort to address the issues.
What is the status of Mental Health in India?
The WHO defines Mental Health as, “ Mental health is a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community. It is an integral component of health and well-being that underpins our individual and collective abilities to make decisions, build relationships and shape the world we live in “.
The WHO calls Mental health as a basic human right. And it is crucial to personal, community and socio-economic development.
According to the WHO, mental illness makes about 15% of the total disease conditions around the world. In 2019, India’s suicide rate was at 12.9 per 1,00,000 persons. This was higher than the regional average of 10.2 and the global average of 9.0. Suicide has become the leading cause of death among those aged 15–29 in India.
In 2017, an estimation of the burden of mental health conditions for the States across India revealed that as many as 197.3 million people (~14% of the population) required care for mental health conditions . This included around 45.7 million people with depressive disorders and 44.9 million people with anxiety disorders .
According to the National Mental Health Survey conducted by NIMHANS in 12 States, the prevalence of mental morbidity is high in urban metropolitan areas. Nearly 1 in 20 persons suffer from depression. 0.9 % of the surveyed population were at high risk of suicide.
According to the NCRB data, 1,64,033 people committed suicide in 2021, a 6.2% rise in comparison to 2020.
What are the harmful effects of poor Mental Health?
Impact on Physical Health : A study found that positive psychological well-being can reduce the risks of heart attack and stroke. On the other hand, poor mental status can lead to poor physical health or harmful behaviour. Depression has been linked to many chronic illnesses . These illnesses include diabetes, asthma, cancer, cardiovascular disease, and arthritis.
Impact on Relationships : Mental-health conditions during adolescence and young adulthood can have a significantly negative impact on the development of safe and healthy relationships with peers, parents, teachers, colleagues and partners.
Impact on Productivity : It impacts a person’s ability to concentrate and engage in productive activities.
The WHO Report on Mental Health and Development (2010) highlighted the risks of a cyclical relationship between vulnerability and poor mental health , in which people with such conditions are a vulnerable group subject to stigma, discrimination, violence, marginalization and other violations of their human rights.
What are the reasons for poor status of Mental Health in India?
Lack of Awareness and Sensitivity : In India, mental health issues are not considered as healthcare issues. Any person suffering from mental issues is considered weak. Stigma and discrimination often undermine social support structures. Persons suffering from such issues are often tagged as ‘lunatics’ by the society. This leads to a vicious cycle of shame, suffering and isolation of the patients .
A survey conducted in 2018 showed that while 87% of the respondents showed some awareness of mental illness, 71% also used terms associated with stigma .

Source: WEF
Lack of Mental Healthcare Personnel : There is a severe shortage of mental healthcare workforce in India. According to the WHO, in 2011, there were 0.301 psychiatrists and 0.047 psychologists for every 100,000 patients suffering from a mental health disorder in India. In contrast, the ratio in most developed countries is in excess of 10.
Gap in Treatment : At present, only 20-30% of people with mental illnesses receive adequate treatment. One major reason for such a wide treatment gap is the problem of inadequate resources.
Low budget Allocation : Developed countries allocate 5-18% of their annual healthcare budget on mental healthcare, while India allocates roughly 0.05% (Organization for Economic Co-operation and Development, 2014) of its healthcare budget. This is the lowest among all G20 countries. Despite a rise in mental illness issues, the Union Ministry of Health allocated less than 1% of its budget to directly deal with psychological illnesses in 2022.
Changed Lifestyle : Increased use of certain kinds of social media is exacerbating stress and mental illness, especially among the young people. Social media detracts from face-to-face relationships , which are healthier, and reduces investment in meaningful activities. More importantly, it erodes self-esteem through unfavourable social comparison. In addition, some experts contend that the shift to nuclear families has reduced the avenues of relieving one’s anxieties as family members are not emotionally available at most crucial times.
Income Inequalities : Mental issues are closely linked with poverty. People living in poverty are at greater risk of experiencing mental health conditions. On the other hand, people experiencing severe mental health conditions are more likely to fall into poverty through loss of employment and increased health expenditure.
What steps have been taken to improve Mental Health in India?
Legal measures.
The Mental Healthcare Act, 2017 : The Act makes several provisions to improve the state of mental health in India. The Act rescinds the Mental Healthcare Act, 1987 which was criticised for failing to recognise the rights and agency of those with mental illness. The Act seeks to ensure rights of the person with mental illness to receive care and to live a life with dignity . It provides the Right to Access to Healthcare : Every person shall have a right to access mental health care and treatment from mental health services run or funded by the appropriate Government. It also empowers person with mental illness to make an advance directive that states how he/she wants to be treated for the illness.
The Act decriminalised suicide stating that whoever attempts suicide will be presumed to be under severe stress , and shall not be punished for it.
Rights of Persons with Disabilities Act, 2017 : The Act acknowledges mental illness as a disability and seeks to enhance the Rights and Entitlements of the Disabled and provide an effective mechanism for ensuring their empowerment and inclusion in society.

Schemes and Initiatives
National Mental Health Programme (NMHP) : Keeping with the WHO’s recommendations, the programme was introduced in 1982 to provide mental health services as part of the general healthcare system. The District Mental Health Programme (DMHP) component of the NMHP has been sanctioned for implementation in 704 districts for which support is provided to States/UTs through the National Health Mission.
Facilities made available under DMHP at the Community Health Centre (CHC) and Primary Health Centre (PHC) levels, include outpatient services, assessment, counselling/ psycho-social interventions , continuing care and support to persons with severe mental disorders , drugs, outreach services, ambulance services etc. In addition to above services there is a provision of 10 bedded in-patient facility at the District level.
Generating Awareness : To generate awareness among masses about mental illnesses Information, Education and Communication (IEC) activities are an integral part of the NMHP . At the District level, sufficient funds are provided to each District under the DMHP (under the Non-communicable Diseases flexi-pool of National Health Mission) for IEC and awareness generation activities in the community, schools, workplaces, with community involvement.
Under the DMHP various IEC activities such as awareness messages in local newspapers and radio, street plays, wall paintings are undertaken by the States/UTs.
National Tele Mental Health Programme : The Government has announced a National Tele Mental Health Programme in the Budget of 2022-23, to further improve access to quality mental health counselling and care services in the country.
Kiran : A 24/7 toll-free helpline called Kiran was established by the Ministry of Social Justice and Empowerment in 2020 to offer support to those dealing with anxiety, stress, depression, suicide thoughts, and other mental issues.
Manodarpan : Students will receive psychosocial help as part of an effort under the Atmanirbhar Bharat Abhiyan , with the goal of improving the students’ mental health and overall well-being. Its components include Advisory Guidelines for students, teachers and faculty of School systems and Universities along with families; National level database and directory of counsellors; Toll-free helpline; Handbook on Psychosocial Support etc.
Issuance of Guidelines/Advisories : Guidelines/ advisories on management of mental illness have been issued by the Government. All the guidelines, advisories and advocacy material can be accessed on the website of the Union Ministry of Health and Family Welfare under ‘Behavioural Health – Psychosocial Helpline’.
What steps can be taken further?
There is a need of an urgent and well-resourced ‘whole-of-society’ approach to protect, promote and care for the mental health of people. This should be based on the following pillars.
First , there is a need to address the deep stigma s urrounding such issues which prevents patients from seeking timely treatment and makes them feel shameful, isolated and weak.
Second , mental health should be made an integral part of the public health programme to reduce stress, promote a healthy lifestyle, screen and identify high-risk groups and strengthen interventions like counselling services. Special emphasis should be given to schools. In addition, special focus should be on groups that are highly vulnerable to mental health issues such as victims of domestic or sexual violence, unemployed youth, marginal farmers, armed forces personnel and personnel working under difficult conditions.
Third , Infrastructure should be improved for mental health care and treatment. Innovative models are required to deepen the penetration of services and staff . ASHAs can be trained for this purpose. Community health workers (ASHAs) can not only educate and sensitize women and children about mental diseases but also guide them to reach the right expert in their locality.
Fourth , The above interventions will require enhanced allocation to mental healthcare in the Budget. Substantial investment will be needed to address the wide treatment gap in the health infrastructure and human resources.
Fifth , Careful mapping and research needs to be undertaken to produce quality data , that is essential to understand the size of the problem. This in turn should be utilised to implement a comprehensive approach, supported by heightened political commitment, scientific understanding and a citizen driven movement.
Sixth , the WHO has recommended Three Paths to transformation towards better Mental Health.

Source: WHO
The status with respect to mental issues has worsened since COVID-19 pandemic. The mental healthcare system in India is under-equipped to deal with the crisis. Urgent interventions, in terms of enhanced budget, increased workforce, and improved awareness are necessary to address the challenge.
Syllabus : GS II, Issues relating to development and management of Social Sector/Services relating to Health.
Source : Indian Express , Indian Express , Economic Times , PIB

Type your email…
Search Articles
Prelims 2024 current affairs.
- Art and Culture
- Indian Economy
- Science and Technology
- Environment & Ecology
- International Relations
- Polity & Nation
- Important Bills and Acts
- International Organizations
- Index, Reports and Summits
- Government Schemes and Programs
- Miscellaneous
- Species in news
The Last Webinar on Mains 2024 | Session by Mr. Ayush Sinha
Explore Our Affordable Courses
- UPSC Offline
- UPSC Online
- UPSC (Live From Classroom)
- UPSC Optional
- UPPSC Offline
- BPSC Offline
- UPPCS Online
- BPSC Online
- MPSC Online
- MPPSC Online
- WBPSC Online
- OPSC Online
- BPSC (Live from Classroom)
- UPPSC (Live From Classroom)
- UPSC Test Series
- State PSC Test Series
- DAILY CURRENT AFFAIRS
- SUBJECT WISE CURRENT AFFAIRS
- DAILY EDITORIAL ANALYSIS
- DAILY CURRENT AFFAIRS QUIZ
- Daily Prelims(MCQs) Practice
- Daily Mains Answer Writing
- Prahaar (Mains Wallah) 2024
- Prahaar Summary 2024
- Mains Marks Booster 2024
- Mains Wallah (Q&A)
- Monthly Current Wallah
- Daily Editorial Summary
- NCERT Wallah
- Prelims PYQs
- Optionals PYQs
- NCERT Notes
- Udaan Notes
- UPSC Prelims Answer Key
- UPSC Syllabus
- Topper's Copies
- Delhi – Mukherjee Nagar Centre
- Delhi – Old Rajinder Nagar Centre
- UP – Lucknow Centre
- UP – Prayagraj Centre
- Bihar – Patna Centre
- Galgotia University Centre

- Offline Centres
- UDAAN Notes
- UPSC Prelims PYQs
- UPSC Mains PYQs
How Swachh Bharat Mission advanced progress on safety and dignity, health and economy
A decade into the Swachh Bharat Mission (SBM) offers a timely opportunity to assess its progress and accomplishments.
About Swachh Bharat Mission (SBM)
- Announcement: The Mission was announced by Prime Minister Narendra Modi during his Independence Day speech from the Red Fort on August 15, 2014, the SBM was officially launched on October 2, 2014. This marked a historic moment, as it was the first time a head of government publicly committed to ending open defecation within a specified timeframe. The initiative was particularly significant because sanitation had previously been a taboo topic and rarely discussed openly.
- Goal: The SBM aimed to transform the sanitation behaviour of 550 million people within a five-year timeframe—a scale previously unimaginable. Additionally, the mission set a target to construct 100 million toilets.
- The program was executed through direct communication with the public via multiple platforms, including the Prime Minister’s monthly “Mann Ki Baat” radio address.
- Community Engagement: The SBM encouraged community and village-led initiatives , fostering a sense of pride and friendly competition among villages, districts, and states as they strived to achieve and declare ODF status. Villages celebrated their success with a “Gaurav Yatra” (pride tour).
By October 2, 2019, all states had declared themselves ODF, marking the successful completion of Phase 1. The focus then shifted to Phase 2, which emphasises sustaining these achievements. This includes ensuring that the toilets remain operational and preventing a return to open defecation.
Enroll now for UPSC Online Course
| Parameswaran Iyer is an Indian civil servant and currently serves as the Executive Director at the World Bank Group, representing Bangladesh, Bhutan, India, and Sri Lanka. Previously, Mr. Iyer was the Chief Executive Officer of , India’s National Think Tank, from July 2022 to February 2023. He is also the a campaign aimed at eradicating open defecation by constructing over 90 million toilets in rural India, and ensuring its success. |
|---|
Benefits of the Swachh Bharat Mission (SBM)
- Health: The Swachh Bharat Mission has led to significant health benefits, including a reduction in the spread of diseases such as diarrhoea. The mission has contributed to preventing child deaths under the age of five by improving sanitation and hygiene.
- Social: The SBM has enhanced dignity and security for women and girls. The importance of toilets for safety and dignity was highlighted in the film Toilet: Ek Prem Katha . The film emphasised how toilets were initially undervalued and demonstrated their crucial role in ensuring women’s safety and security.
- Economic: A UNICEF study estimated that achieving ODF status in a village saved each household approximately Rs 50,000 annually through reduced medical expenses and time savings. Additionally, a cartoon from the annual Sudhir Dar SBM calendar humorously depicted a bored doctor at a primary health centre, no longer seeing patients due to the reduction in diarrhoea cases.
| Prime Minister Modi, along with the Secretary-General of the United Nations, chaired the event, which was attended by 55 Health and Sanitation Ministers from developing countries. This inspired other nations to initiate similar programs in their own countries. , the Nigerian Minister for Water and Sanitation, inspired by the conference, launched the Clean Nigeria Campaign upon returning to his country. |
|---|
Reason behind the Success of the Swachh Bharat Mission (SBM)
The Success of the Swachh Bharat Mission is encapsulated in the Delhi Declaration, which highlights the four Ps:
- Political Leadership: PM Modi’s leadership demonstrated that strong willpower and decisive action can overcome challenges and drive progress. Effective leadership is crucial for making tough decisions and achieving goals.
- Public Financing: Government funding is essential for such initiatives. The SBM benefited from substantial financial support, which facilitated the construction of toilets and other infrastructure.
- Partnerships: Collaboration among all stakeholders is vital. The SBM succeeded due to partnerships with state governments, private sector players, and other entities.
- People’s Participation: No initiative can succeed without broad public support. The SBM’s effectiveness was largely due to high levels of community involvement and participation.
These principles are now globally recognized as essential for the success and full implementation of large-scale, transformational development programs. Many other states are adopting these principles to advance their own sanitation initiatives, contributing significantly to Sustainable Development Goal 6: Access to sanitation and water.
Check Out UPSC CSE Books From PW Store
The Swachh Bharat Mission is one of several successful government schemes aimed at improving the quality of life for ordinary Indians. Other notable initiatives include Ujjwala (providing cooking gas cylinders), Jan Dhan (offering bank accounts), the Awas Yojana (housing), Ayushman Bharat (medical insurance), and the Jal Jeevan Mission (supplying clean water to 180 million households). These programs exemplify how large-scale initiatives can drive substantial progress. The principles of Jan Bhagidari—along with key factors such as political leadership, public financing, and partnerships—are crucial and should be applied when launching similar large-scale initiatives.
|
|
|---|
To get PDF version, Please click on "Print PDF" button.

- Recent Post
- Related Post
- Most Viewed Post
Sources of Black Money
Weather gods: On Mission Mausam
Is it time for India to introduce a Universal Basic Income?
Why inequality between south and west india and north and ea....
Cyber Warfare (Fifth Domain of Warfare): Revision
On the extended coverage of the Ayushman Bharat Scheme

India’s Health Care Journey: Progress and Promise | PW...

Patient Safety Rights Charter: A Global Initiative for Safer...

ILO Report On Occupational Safety And Health (OSH)
Outreach to diaspora and statesmanship, india and the artemis accords, laying the foundation for a future-ready digital india, latest comments, recent editorial.
Is it time for India to introduce a Universal Basi...
Why inequality between South and West India and No...
On the extended coverage of the Ayushman Bharat Sc...
Popular current affairs
News In Shorts : 13 September 2024
Cholera Resurgence
India’s Proposal to Reduce Remittance Costs
Elephant Migration from Nilgiris to New York
Commission for Scientific and Technical Terminolog...
Our Courses

THE MOST LEARNING PLATFORM
Learn From India's Best Faculty
Our Initiatives
Beginner’s roadmap, quick links.

PW-Only IAS came together specifically to carry their individual visions in a mission mode. Infusing affordability with quality and building a team where maximum members represent their experiences of Mains and Interview Stage and hence, their reliability to better understand and solve student issues.
Subscribe our Newsletter
Sign up now for our exclusive newsletter and be the first to know about our latest Initiatives, Quality Content, and much more.
Contact Details
G-Floor,4-B Pusa Road, New Delhi, 110060
- +91 9920613613
- [email protected]
Download Our App
Biginner's roadmap, suscribe now form, fill the required details to get early access of quality content..
Join Us Now
(Promise! We Will Not Spam You.)
CURRENT AF.
<div class="new-fform">
Select centre Online Mode Hybrid Mode PWonlyIAS Delhi (ORN) PWonlyIAS Delhi (MN) PWonlyIAS Lucknow PWonlyIAS Patna Other
Select course UPSC Online PSC ONline UPSC + PSC ONLINE UPSC Offline PSC Offline UPSC+PSC Offline UPSC Hybrid PSC Hybrid UPSC+PSC Hybrid Other
</div>
- India’s Cultural Heritage: Preserving the past, Inspiring the future
- Threads of Transformation: India's Textile Industry Weaving a Modern Future
- Redefining Governance: India's Path to Administrative Reforms
- Beyond Metros: The Ascent Of India's Tier 2 and TIer 3 Cities
- Climate Change Negotiations (CCNs): From Rio (1992) to Dubai (2023)
- Changing Dynamics of Family Structure in India
- India's Creative Economy: From Imagination to Innovation
- India Abroad: Legacy of Indian Diaspora
- Social Identities and Structural Transformation in India
- Investment Ecosystem in India
- Digital Inclusion in India: Building a Connected and Empowered Nation
- Weekly Focus
Latest Edition
- Monthly Magazine
- Economic Survey
- Quarterly Revision Documents
- Year End Review of Ministries
- Previous Year Questions
- The Planet Vision
- Weekly Focus: In Conversation
- Simplified by VisionIAS
- Personality in Focus
- Schemes in Focus
August 2024
- Polity & Governance International Relations Economics (Indian Economy) Security Environment Geography Social Issues Science & Technology Modern India History Ethics Schemes In News Places In News Art & Culture Economics (Macroeconomics)
Table of Content
- 1.1 Sub-Classification of Scheduled Castes
- 1.2 Centrally Sponsored Schemes (CSSs)
- 1.3 Citizen Participation Towards Good Governance
- 1.4 Lateral Entry In Civil Services
- 1.5 Surrogate advertisements
- 1.6 Uniform Civil Code (UCC)
- 1.7 Legislative Impact Assessment
- 1.8 News in Shorts
- 2.1 India and Global South
- 2.2 Global Development Compact
- 2.3 India's Act East Policy
- 2.4 India Vietnam Relation
- 2.5 India Malaysia Relations
- 2.6 India-Central and Eastern Europe Relations
- 2.7 India-Poland Relationship
- 2.8 India-Ukraine Relationship
- 2.9 Para- Diplomacy
- 2.10 Tensions in South China Sea
- 2.11 News in Shorts
- 3.1 New Schemes for Agriculture Sector
- 3.2 Livestock Sector in India
- 3.3 Digital Agriculture Mission
- 3.4 Sustainable development of Horticulture
- 3.5 National Pest Surveillance System (NPSS)
- 3.6 Pradhan Mantri Mudra Yojana (PMMY)
- 3.7 LTCG & Indexation Benefit
- 3.8 Creative Economy
- 3.9 News in Shorts
- 4.1 India’s Nuclear doctrine
- 4.2 News in Shorts
- 5.1 Disaster Management (Amendment) Bill, 2024
- 5.2 Technology in DMRR
- 5.3 Renewable Energy (RE) in India
- 5.4 Sea Level Rise
- 5.5 News in Shorts
- 6.1 River Linking Project
- 7.1 Safety of Healthcare Professionals
- 7.2 Mental Health of Students
- 7.2.1 Why in the News?
- 7.2.2 More on news:
- 7.2.3 What is mental health?
- 7.2.4 Factors contributing to mental health problems among students:
- 7.2.5 Issues with handling mental care in India:
- 7.2.6 Way-forward
- 7.3 News in Shorts
- 8.1 BioE3 Policy
- 8.2 National Space Day
- 8.3 Fixed Dose Combination Drugs
- 8.4 A1 and A2 Milk
- 8.5 Directed Energy Weapons
- 8.6 News in Shorts
- 9.1 Hindustan Republican Association (HRA)
- 10.1 Emotional Intelligence
- 10.2 Social Influence and Persuasion using Social Media
- 11.1 Agri SURE Fund
- 11.2 PM KUSUM
- 13.1 News in Shorts
- 14.1 News in Shorts
Mental Health of Students
Posted 12 Sep 2024
Updated 14 Sep 2024
Why in the News?
National Task Force for Mental Health and Wellbeing of Medical Students submitted its report in response to alarming incidents of suicides by medical students in last five years.
More on news:
- Report emphasizes the high prevalence of depression among Indian medical students.
- The Commission’s online survey showed that a whopping 27.8 per cent of undergraduate students had mental-health conditions and 31.3 per cent of postgraduate students had suicidal thoughts.
- A study by the National Institute of Mental Health and Neurosciences (NIMHANS) found that 23 percent of school children in India have mental health problems.
- National Mental Health Survey (2015–2016) reported a 7% prevalence of psychiatric disorders in 13–17 years and was nearly equal among both the genders.
- A study conducted by schizophrenia research foundation (SCARF) in Chennai found that over 30% of students suffer from anxiety and depression.
What is mental health?
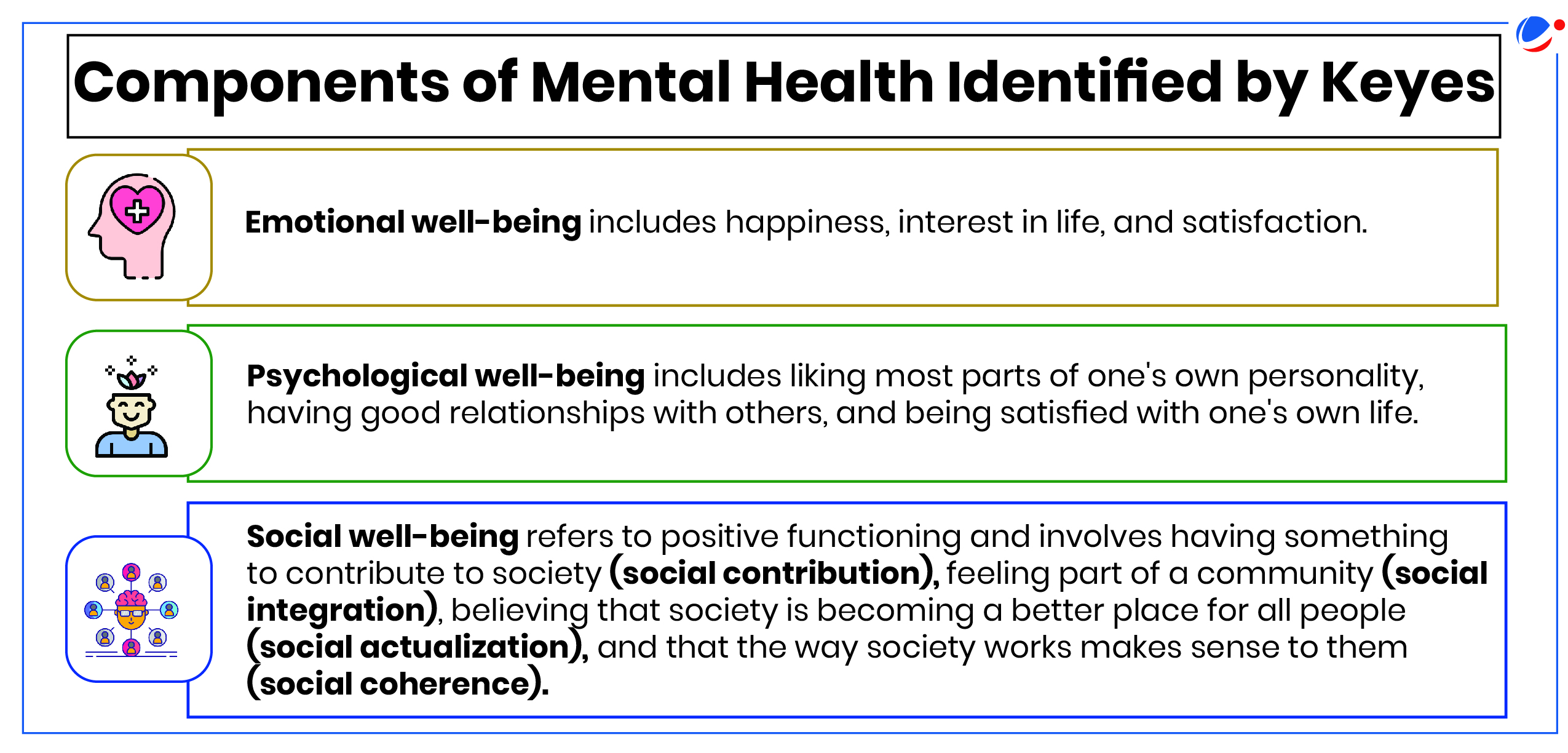
- Mental health is best understood as a resource , one that allows individuals to recognize and understand their skills and potential that they may use to pursue their passions and dreams within sport.
Factors contributing to mental health problems among students:
- Immediate triggers for mental health crises among students include f inancial loss, sudden grief, mental health deterioration, and adverse life events such as failing exams or public humiliation E.g. Suicides in IITs.
- Influence of Social Media: A 2018 British study tied social media use to decreased, disrupted, and delayed sleep, which is associated with depression, memory loss, and poor academic performance.
- Intense combination of relentless academic pressure, financial sacrifice, and high parental expectations are also key factors behind students suicide in places like Kota.
- Genetic predispositions, such as alterations in gene expression and family history of suicide , can increase suicide risk by affecting brain function and behavior.
- Certain personality traits like impulsivity, along with disabilities and major physical illnesses , may also elevate risk by contributing to feelings of isolation, stress, and depression.
- Stigmatization: Because of stigma against seeking mental health care issues are not identified at the initial stage.
Issues with handling mental care in India:
- Fragmented approach: Insufficient Integration into Primary Healthcare results in a fragmented approach to mental healthcare
- Geographical disparities in Infrastructure and Resources: Rural & remote areas, often lack necessary infrastructure
- Shortage of Mental Health Professionals: Only 0.75 psychiatrists/lakh population in India (Economic Survey 2023-24).
- Lack of Awareness and Stigma leads to discrimination, social isolation, and prejudice against individuals seeking help.
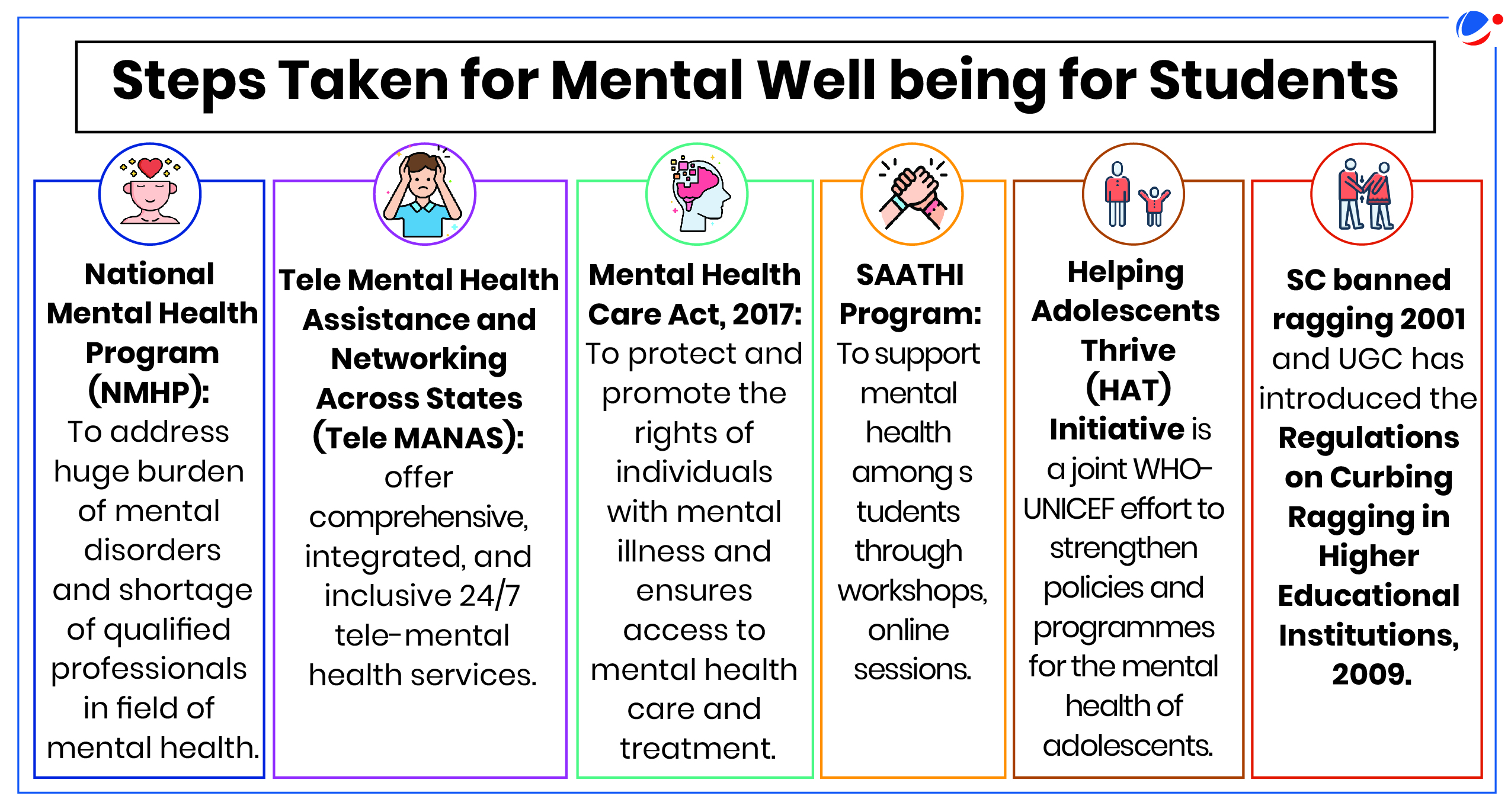
Way-forward
- Implement Regular Training Programs: Conduct regular training sessions for faculty to identify and support students at risk.
- Counseling Services: A 24/7 Support System should be implemented across schools and colleges. This can be done quickly by implementing TeleMANAS initiative using the toll-free number (14416) in all colleges.
- Children and adolescents require special attention considering that around half of all mental health disorders start by the age of fourteen years.
- Policy reforms and resource allocation: By Allocating Adequate Resources, Prioritizing Mental Health in the Healthcare Agenda and adopt an integrated approach that addresses mental health's biological, psychological, and social determinants.
- Digital Detox Programs: Encouraging students to balance digital activities with physical exercise, hobbies, and offline social interactions can help mitigate the negative impacts of excessive digital use.
- Practicing self-awareness: Students can improve mental well-being by practicing self-awareness, mindfulness, and regular exercise, while also maintaining healthy sleep and eating habits to reduce anxiety and build emotional resilience.
- Mental Health
- Components of Mental Health
- TeleMANAS initiative
- SAATHI Programme
Articles Sources
Economic Survey 2023-24 highlighted an increase in Mental Health Issues among Indians
Welcome Back !
Please login to your account for a personalized experience.
- Ground Reports
- 50-Word Edit
- National Interest
- Campus Voice
- Security Code
- Off The Cuff
- Democracy Wall
- Around Town
- PastForward
- In Pictures
- Last Laughs
- ThePrint Essential


New Delhi: There is nearly 80 percent shortage of specialist doctors at community health centres (CHCs) across rural India, according to a new government report, indicating that the rising number of seats in medicine has hardly had any impact on specialised healthcare delivery beyond cities.
Rural CHCs are 30-bed facilities below district hospitals and provide secondary-level healthcare services to approximately 1.6 lakh people on average. In addition to a general duty medical officer, anaesthetist and paramedics, these are manned generally by four medical specialists: surgeon, physician, gynaecologist, and paediatrician.
The Health Dynamics of India 2022-23 report released by the Union health ministry Monday showed that only 4,413 specialist doctors of the requisite 21,964 needed in CHCs in March 2023 were available—a shortfall of 17,551 or 79.9 percent. There are 5,491 rural CHCs in 757 districts of the country.
The data also showed that the availability of specialists at 868 CHCs in urban areas was slightly better at 56 percent.
Interestingly, the statistics reveal that the crisis of specialist doctors at rural CHCs may have worsened over the years.
In comparison, the numbers show that at the primary health centres—the first point of contact between the community and a medical officer (normally an MBBS)—there is a shortfall of 976, or less than 4 percent, of doctors. To be sure, these are overall numbers and there are some states and Union Territories that are not experiencing any shortfall.
These figures suggest that, owing to the gradual rise of medical colleges in the country, there may be more MBBS doctors now available to serve in the hinterlands, but a majority of those with post-graduate (MS and MD) degrees are still shying away from serving at government facilities in rural areas.
Experts said that the figures are an indication that CHCs are failing to serve their purpose.
“These dismal statistics are a message to the government that it either needs to revise its strategy to improve specialist care in rural areas or completely shut these centres,” said public health specialist Dr Antony K.R., who is independent monitor of the Centre’s National Health Mission.
The report also shows that there are 27,304 doctors and specialists employed across 714 district hospitals in the country, against a sanctioned strength of 33,964—which means that nearly 20 percent of these seats are vacant too.
Bleak numbers
The new report, which was earlier called the Rural Health Statistics, showed that in rural CHCs, there was a shortfall of 4,578 surgeons, or 83.3 percent; 4,078 obstetricians and gynaecologists, or 74.2 percent; 4,499 physicians, or 81.9 percent; and 4,425 paediatricians, or 80.5 percent.
The number of each of these specialists required in rural CHCs is 5,491.
The situation is particularly bleak in large states such as Madhya Pradesh, Bihar, Uttar Pradesh, Rajasthan, Gujarat, and Tamil Nadu which have a shortage of 94 percent, 80.9 percent, 74.4 percent, 80.3 percent, 88.1 percent, and 85.2 percent, respectively.
Experts underline that the lack of specialist doctors in CHCs often puts unnecessary burdens on district hospitals, which are often stretched to capacity, thus depriving a large number of the rural population of specialist care closer to their homes.
Also, this shortage of specialists seems to be worsening year after year. There was, for instance, a shortfall of 17,525 specialists at CHCs in 2014-15, 17,459 in 2018-19 and 17,519 in 2020-21. It has become 17,551 now. In 2005—used as a comparative in the document—there was a shortfall of 6,110 specialists, 44 percent, against the required 13,884 specialist doctors in rural areas.
“The picture is getting gloomier every year,” said Antony. He added that states should also stop the practice of upgrading PHCs into CHCs when they cannot ensure specialist care at these centres.
Data show that 2,145 CHCs were added between 2005 and 2023, with Uttar Pradesh, Tamil Nadu, Bihar, Rajasthan, and West Bengal adding most of these facilities.
Mismatch in demand & supply
Last month, the health ministry presented statistics in Parliament that showed that India’s doctor-population ratio now is 1:836—higher than the World Health Organisation (WHO) prescribed ratio of 1 doctor per 1000 population.
The total number of registered modern medicine doctors, according to the statistics, is 13,86,136.
The data also showed that India now has 731 medical colleges offering 1,12,112 MBBS seats and 72,627 post-graduate or post-graduate equivalent seats in medicine.
In comparison, according to the details shared by the government, there were 51,348 MBBS seats and 31,185 PG seats in medicine before 2014.
The major initiatives that have led to more seats in medicine are relaxing the norms for opening and running MBBS course and allowing 1 teacher for every 3 PG students, as opposed to 1:2 ration that was prevalent earlier.
Also, diplomate degree after MBBS—Diplomate of National Board—which are run by hospitals, including large corporate hospitals, and not necessarily medical colleges, are now considered PG equivalent.
But clearly, said Dr T. Sundararaman, who has previously headed the Union government’s National Health System Resource Centre, and is now associated with Jan Swasthya Abhiyan, very few PG doctors are interested in working in rural areas.
“It is a problem that has persisted for 25 years—from the design of the health facility pyramid to a push towards privatisation, there may be a lot of reasons for the specialist crisis beyond cities,” he said.
“On many occasions, while CHCs have sanctioned posts for specialists, they are not equipped to provide specialist care, which is why PG doctors are not interested in working at such centres.”
Also, Sundararaman said, as a large number of speciality and super-speciality seats are pursued in the private sector where doctors have to spend lakhs to secure a degree, they are unlikely to see serving in a rural hospital as a lucrative prospect.
“In my view, providing for the post of a single surgeon in a CHC is not helpful as they often find it difficult to operate,” he said, adding that the functioning of CHCs needs to be reevaluated.
“It may be helpful to deploy doctors in family medicine with an upgraded skill in basic surgeries at CHCs,” he said, adding that the unified test for entrance into PG medicine (National Eligibility-cum-Entrance Test or NEET-PG) should incentivise those who commit to work in rural areas.
Antony, who has previously worked as health and nutrition specialist with UNICEF India, suggested that the national medical regulator should see that post graduate seats are increased in specialties whose pass-outs will serve at the CHCs.
“The country needs more PG seats in paediatrics, obs-gynae and general surgery as compared to other specialities because these specialists are more needed in rural areas to provide specialist care to people closer to their homes,” Antony said.
(Edited by Sanya Mathur)
Also Read: NMC’s U-turn on norms that listed lesbianism as sexual offence not its first. Here’s what happened
Subscribe to our channels on YouTube , Telegram & WhatsApp
Support Our Journalism
India needs fair, non-hyphenated and questioning journalism, packed with on-ground reporting. ThePrint – with exceptional reporters, columnists and editors – is doing just that.
Sustaining this needs support from wonderful readers like you.
Whether you live in India or overseas, you can take a paid subscription by clicking here .
- Community health centres
- Health Ministry
- Rural India
LEAVE A REPLY Cancel
Save my name, email, and website in this browser for the next time I comment.
Most Popular
Chin leader rejects mizoram cm’s appeal to build ties with ‘strong’ arakan army. ‘might cannot decide it’, onam inside a nair tharavad—sadhya made easy in a new cookbook.
Required fields are marked *
Copyright © 2024 Printline Media Pvt. Ltd. All rights reserved.
- Terms of Use
- Privacy Policy

- Insights IAS Brochure |
- OUR CENTERS Bangalore Delhi Lucknow Mysuru --> Srinagar Dharwad Hyderabad
Call us @ 08069405205

Search Here

- An Introduction to the CSE Exam
- Personality Test
- Annual Calendar by UPSC-2025
- Common Myths about the Exam
- About Insights IAS
- Our Mission, Vision & Values
- Director's Desk
- Meet Our Team
- Our Branches
- Careers at Insights IAS
- Daily Current Affairs+PIB Summary
- Insights into Editorials
- Insta Revision Modules for Prelims
- Current Affairs Quiz
- Static Quiz
- Current Affairs RTM
- Insta-DART(CSAT)
- Insta 75 Days Revision Tests for Prelims 2024
- Secure (Mains Answer writing)
- Secure Synopsis
- Ethics Case Studies
- Insta Ethics
- Weekly Essay Challenge
- Insta Revision Modules-Mains
- Insta 75 Days Revision Tests for Mains
- Secure (Archive)
- Anthropology
- Law Optional
- Kannada Literature
- Public Administration
- English Literature
- Medical Science
- Mathematics
- Commerce & Accountancy
- Monthly Magazine: CURRENT AFFAIRS 30
- Content for Mains Enrichment (CME)
- InstaMaps: Important Places in News
- Weekly CA Magazine
- The PRIME Magazine
- Insta Revision Modules-Prelims
- Insta-DART(CSAT) Quiz
- Insta 75 days Revision Tests for Prelims 2022
- Insights SECURE(Mains Answer Writing)
- Interview Transcripts
- Previous Years' Question Papers-Prelims
- Answer Keys for Prelims PYQs
- Solve Prelims PYQs
- Previous Years' Question Papers-Mains
- UPSC CSE Syllabus
- Toppers from Insights IAS
- Testimonials
- Felicitation
- UPSC Results
- Indian Heritage & Culture
- Ancient Indian History
- Medieval Indian History
- Modern Indian History
- World History
- World Geography
- Indian Geography
- Indian Society
- Social Justice
- International Relations
- Agriculture
- Environment & Ecology
- Disaster Management
- Science & Technology
- Security Issues
- Ethics, Integrity and Aptitude
- Insights IAS Brochure

- Indian Heritage & Culture
- Enivornment & Ecology

- How to Study Art & Culture?
- What is Art and Culture? What is the difference between the two?
- Indus Civilization
- Evolution of rock-cut architecture in India
- Important rock-cut caves
- The contribution of Pallavas to Rock-cut architecture
- Comparision of art form found at Ellora and Mahabalipuram
- Buddhist Architecture
- Early Temples in India
- Basic form of Hindu temple
- Dravida style of temple architecture
- Nagara Style or North India Temple style
- Vesara style of temple architecture
- Characteristic features of Indo-Islamic form of architecture
- Styles of Islamic architecture in the Indian subcontinent
- Types of buildings in Islamic architecture in the Indian subcontinent
- Evolution of this form of architecture during the medieval period
- Modern Architecture
- Post-Independence architecture
- Indus Civilization Sculpture
- Bharhut Sculptures
- Sanchi Sculptures
- Gandhara School of Sculpture
- Mathura School of Sculpture
- Amaravati School of Sculpture
- Gupta Sculpture
- Medieval School of Sculpture
- Modern Indian Sculpture
- Pre Historic Painting
- Mural Paintings & Cave Paintings
- Pala School
- Mughal Paintings
- Bundi School of Painting
- Malwa School
- Mewar School
- Basohli School
- Kangra School
- Decanni School of Painting
- Madhubani Paintings or Mithila paintings
- Pattachitra
- Kalighat Painting
- Modern Indian Paintings
- Personalities Associated to Paintings
- Christianity
- Zoroastrianism
- Six Schools of Philosophy
- Lokayata / Charvaka
- Hindustani Music
- Carnatic Music
- Folk Music Tradition
- Modern Music
- Personalities associated with Music
- Bharatanatyam
- Mohiniattam
- Folk Dances
- Modern Dance in India
- Sanskrit Theatre
- Folk Theatre
- Modern Theatre
- Personalities associated with Theatre
- History of Puppetry
- String Puppetry
- Shadow Puppetry
- Rod Puppetry
- Glove Puppetry
- Indian Cinema and Circus
- Shankaracharya
- Ramanujacharya (1017-1137AD)
- Madhvacharya
- Vallabhacharya
- Kabir (1440-1510 AD)
- Guru Nanak (1469-1538 AD)
- Chaitanya Mahaprabhu
- Shankar Dev
- Purandaradasa
- Samard Ramdas
- Classical Languages
- Scheduled Languages
- Literature in Ancient India
- Buddhist and Jain Literature
- Tamil (Sangam) Literature
- Malayalam Literature
- Telugu Literature
- Medieval Literature
- Modern Literature
- Important characteristics of Fairs and Festivals of India
- Some of the major festivals that are celebrated in India
- Art & Crafts
- Ancient Science & Technology
- Medieval Science & Technology
- Famous Personalities in Science & Technology
- Tangible Cultural Heritage
- Intangible Cultural Heritage
- Cultural Heritage Sites
- Natural Heritage Sites
- Important Institutions
- Important programmes related to promotion and preservation of Indian heritage
- Ochre Colored Pottery (OCP)
- Black and Red Ware (BRW)
- Painted Grey-Ware (PGW)
- Northern Black Polished Ware (NBPW)
- Origin of Martial arts in India
- Various forms of Martial arts in India
- Situation of Child Labour in India
- Poverty and Child labour- a vicious cycle
- Impact of the pandemic
- Government measures undertaken to eradicate child labour in India
- Challenges before policy makers with respect to child labour.
- Way Forward
- Facts and figures about the prevalence of Child marriage in India
- Factors leading to child marriage in India
- Interlinkages of poverty and child marriages in India
- Impact of child marriage on Indian economy
- Government measures undertaken so far to curb Child Marriages in India
- Measures needed to prevent child marriages
- The Poor state of Hunger and Malnutrition in India
- Multi-dimensional determinants of malnutrition
- Covid-19 impact on malnutrition in children in India
- Government effort to fight malnutrition
- Addressing malnutrition: Measures needed
- Procedure in place to protect children
- Government measures needed
- Role of NCPCR
- Shortcomings of NCPCR
- Way forward
- Key findings of the report in India
- Impact of COVID-19
- Government Measures undertaken
- Measures needed
- Constitutional Provisions to safeguard children
- Child Abuse in India
- Impacts of child abuse
- Government initiatives undertaken
- On children
- On families
- On individual
- Challenges to ban child pornography
- Causes for child mortality
- Government initiatives
- Geographic spread of minorities in India
- Socio-economic status of minorities in India
- Importance of recognition of rights of minorities
- Parameters to define minority in India
- Lack of uniformity in determining minorities
- Prejudice & Discrimination
- Problem of Identity
- Problem of Security
- Problem Relating to Equity
- Problem of Communal Tensions and Riots
- Lack of Representation in Civil Service and Politics
- Problem of Providing Protection
- Failure to Stick on Strictly to Secularism
- Problem of Lack of Representation in Civil Service and Politics
- Key findings related to minorities
- Various factors responsible for under-representation of enrolled minorities
- Problem of Separatism
- Problem Relating to the Introduction of Common Civil Code
- Problems faced by minority women in India
- Factors leading to anger against minorities
- Constitutional Safeguard for Minorities
- Government Welfare Measures for Minorities
- Composition
- Lacunae in NCM
- Measures needed to make NCM more effective
- Major Findings
- Main Recommendations
- Review of the implementation of recommendations of Sachar committee report after Ten Years
- Status of Education in India
- Importance of Education for India
- Contemporary challenges in education sector in India
- Other existing issues
- Measures Needed for Issues related to Education Sector
- Way forward for Issues related to Education Sector
- Feature of Right to Education (RTE) Act, 2009
- Significance of RTE Act, 2009
- Achievements of RTE Act,2009
- Limitations of RTE Act, 2009
- Measures needed foe Right to Education
- Importance of Education as a necessary public good
- Challenges faced by Government schools
- Measures needed for Public Education System in India
- Way forward for Public Education System in India
- Key highlights of the NEP
- Significance of National Education Policy 2020
- Issues with the NEP- 2020
- Measures needed for effective implementation
- Way Forward for New Education Policy
- Three language policy
- Concerns associated over three language formula
- Way forward for Three language formula in India
- Significance of emphasizing native languages in the education system of India
- Way forward for Native language in education
- Significance of ECCE
- NEP 2020 and ECCE
- Challenges for Early Childhood Care and Education
- Way forward for Early Childhood Care and Education
- Need for reforms
- Findings of ASER Report 2019
- Challenges faced – Primary Education in India
- Government Schemes for Elementary Education
- Measures needed for Primary Education in India
- Government Schemes for Secondary Education
- Challenges facing higher education system
- Government schemes for Higher Education
- Measures needed for Higher Education in India
- Way forward for Higher Education in India
- Reasons behind poor quality of teachers
- Opportunities present
- Government Initiative so far
- Way forward for Teacher Education in India
- Present Status
- Advantages of Developing Female Education in India
- Challenges for Gender Imparity in Education
- Way Forward for Gender Imparity in Education
- Crisis of education in India in times of Pandemic
- Impacts on education due to COVID-19 pandemic
- Challenges posed by Online Education
- Online education as a supplement to Traditional Educational Institutes
- Challenges facing medical education in India
- Can private participating alleviate the concerns?
- Government proposal in this regard
- Way forward for Medical Education in India
- Need for value education
- Importance of value education
- Issues related to SC/ST
- Scheduled Caste
- Issues faced by Scheduled Castes
- Major reasons behind miserable conditions of Scheduled Castes
- Constitutional mechanism for upliftment of SC
- Government Initiatives taken for Scheduled Caste development
- Educational Empowerment
- Economic Empowerment
- Social Empowerment
- Evaluation of Government Schemes
- Failure of the Indian judiciary to protect the rights of the people
- Measures needed for Scheduled Caste
- Way forward for Scheduled Caste
- Dalit Women
- Challenges faced by Dalit Women
- Atrocities against Dalit women
- Role of Indian judiciary in protecting sexual violence victims
- Criticism against ignorance of caste-based violence
- Aspects which have improved so far
- Measures needed for Dalit Women
- Way forward for Dalit Women
- National Commission for Scheduled Castes
- Issues related to the role of National Commission for Scheduled Castes
- Measures need to be taken up by NCSC
- Scheduled Tribe
- Definition of Scheduled tribe
- Various problems of tribal communities in India
- Constitutional Safeguards for STs
- Educational & Cultural Safeguards
- Social Safeguard
- Economic Safeguards
- Political Safeguards
- Service Safeguards
- The Fifth Schedule of the Constitution
- The Sixth Schedule of the Constitution
- Need for Sixth Schedule
- Sixth Schedule areas: Benefits of devolving powers
- Issues related to sixth schedule areas
- Legislative measures
- The Scheduled Tribes and Other Traditional Forest Dwellers (Recognition of Forest Rights) Act, 2006
- Rights under the Act
- Eligibility
- Need for the law
- Issues with the law and its implementation
- Measures needed in FRA’s
- XAXA Committee
- Panchayats (Extension to Scheduled Areas) Act, 1996
- Problems with PESA
- Government Initiatives for ST
- Way Forward in women and health
- Way forward for ST
- Way forward for PVTGs
- Way forward in Violence/crime against Women
- Way forward in sex ratio
Home » Social Justice » Issues related to Health Sector » Privatization of healthcare in India
Privatization of healthcare in India
Will privatization of healthcare work in India?
- India opened up markets to private participation 30 years ago and reaped its benefits on multiple dimensions.
- As the general pattern shows, the value delivered for prices charged—or ‘value for money’—has risen in arenas that have come to be dominated by private players and also boast of a fair degree of competitive intensity.
- However, two critical sectors that have gone the private way, even as state provisions withered, should cause us profound unease: education and healthcare.
- Neither can operate on a laissez-faire model, given their special need for oversight, nor can our trend of service privatization be relied upon to give us the base of human capital needed for long-term economic success.
- At another level, both are welfare assurers and thus ought to have the government as their predominant both are welfare assurers and thus ought to have the government as their predominant provider.
- With state inadequacies exposed by the covid pandemic, our need to attain a balance is particularly acute in healthcare, where less than a fifth of all Indians avail of public facilities, as estimated.
Challenges associate with privatization of healthcare:
- Privatization will increase the gap between rich and poor which will encourage survival of the richest, which cannot be the goal of any civilized society.
- The public hospitals offer subsidized and other free services which makes most of the people move away from private hospitals.
- The uninsured patients will suffer from high bills of the treatment.
- The lack of regulation of private players is likely to exploit its clients and customers either financially or physically.
- There is no answerability of private sector to government regulatory board over their functioning and operations.
Measures needed:
- Government should make the guidelines regarding the provision of services provided, areas of involvement, quality of services provided and many more such factors before opting for privatization of healthcare sector.
- Multidisciplinary approach with public health experts taking the lead role can help in establishing a better healthcare environment in India.
- States should create a health advisory committee with experts from the faculty of public health, business management/health administration institutions, not-for-profit health NGOs, for-profit health organizations, and state health departments.
- Block-wise analysis up to sub-centre level should be done for each district in order to have a shared understanding of strengths and weaknesses of the health system, activate joint action plans, minimize duplication of efforts, and optimize scarce resources.
- Computerization of the health service input and output data according to the institutions shall be a primary requirement to identify better performing institutions/individuals based upon agreed minimum indicators for strengthening accountability in the system.
- A separate public health cadre at district level should be created with suitable avenues for upgradation of educational qualification to postgraduate level, i.e. Master of Public Health and MD in Community Medicine.
Way forward:
- The goal of the private firms should not involve only profit-making as their motivation for the provision of quality services but they should also focus on efficiency and effectiveness in healthcare.
- Privatization is beneficial if the structures are set properly, otherwise, it will defeat the purpose and goal of healthcare.
- For ensuring equitable representation of both private and public sector interests, it is necessary that the governing body includes members nominated from the private sector also.
- Government should study the breadth of the healthcare landscape and benchmark the standards with other developing and developed countries and identify critical areas and gaps.

- Our Mission, Vision & Values
- Director’s Desk
- Commerce & Accountancy
- Previous Years’ Question Papers-Prelims
- Previous Years’ Question Papers-Mains
- Environment & Ecology
- Science & Technology

- Classroom Programme
- Interview Guidance
- Online Programme
- Drishti Store
- My Bookmarks
- My Progress
- Change Password
- From The Editor's Desk
- How To Use The New Website
- Help Centre
Achievers Corner
- Topper's Interview
- About Civil Services
- UPSC Prelims Syllabus
- GS Prelims Strategy
- Prelims Analysis
- GS Paper-I (Year Wise)
- GS Paper-I (Subject Wise)
- CSAT Strategy
- Previous Years Papers
- Practice Quiz
- Weekly Revision MCQs
- 60 Steps To Prelims
- Prelims Refresher Programme 2020
Mains & Interview
- Mains GS Syllabus
- Mains GS Strategy
- Mains Answer Writing Practice
- Essay Strategy
- Fodder For Essay
- Model Essays
- Drishti Essay Competition
- Ethics Strategy
- Ethics Case Studies
- Ethics Discussion
- Ethics Previous Years Q&As
- Papers By Years
- Papers By Subject
- Be MAINS Ready
- Awake Mains Examination 2020
- Interview Strategy
- Interview Guidance Programme
Current Affairs
- Daily News & Editorial
- Daily CA MCQs
- Sansad TV Discussions
- Monthly CA Consolidation
- Monthly Editorial Consolidation
- Monthly MCQ Consolidation
Drishti Specials
- To The Point
- Important Institutions
- Learning Through Maps
- PRS Capsule
- Summary Of Reports
- Gist Of Economic Survey
Study Material
- NCERT Books
- NIOS Study Material
- IGNOU Study Material
- Yojana & Kurukshetra
- Chhatisgarh
- Uttar Pradesh
- Madhya Pradesh
Test Series
- UPSC Prelims Test Series
- UPSC Mains Test Series
- UPPCS Prelims Test Series
- UPPCS Mains Test Series
- BPSC Prelims Test Series
- RAS/RTS Prelims Test Series
- Daily Editorial Analysis
- YouTube PDF Downloads
- Strategy By Toppers
- Ethics - Definition & Concepts
- Mastering Mains Answer Writing
- Places in News
- UPSC Mock Interview
- PCS Mock Interview
- Interview Insights
- Prelims 2019
- Product Promos
Social Justice
Make Your Note
Mental Healthcare
- 12 Dec 2018
- 16 min read
- GS Paper - 2
- Issues Related to Disability
- Issues Arising Out of Design & Implementation of Policies
Last Updated: October 2022
For Prelims: World Mental Health Day, Mental HealthCare Act 2017, Kiran Helpline, Manodarpan Initiatives, MANAS
For Mains: Mental Health as a basic human right, Challenges associated to promoting mental health in India
What is Mental Health?
According to the World Health Organisation (WHO) , mental health is defined as a state of well-being in which every individual realizes his or her own potential , can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.
- Mental health is a basic human right and it is crucial to personal, community and socio-economic development.
What are the Determinants of Mental Health?
Multiple individual, social and structural determinants combine to protect/undermine our mental health and shift our position on the mental health continuum.
- Individual psychological and biological factors such as emotional skills , substance use and genetics can make people more vulnerable to mental health problems.
- Exposure to unfavourable social, economic, geopolitical and environmental circumstances – including poverty, violence, inequality and environmental deprivation – also increases people’s risk of experiencing mental health conditions.
- For example, harsh parenting and physical punishment is known to undermine child health and bullying is a leading risk factor for mental health conditions.
- Protective factors similarly occur throughout our lives and serve to strengthen resilience. They include our individual social and emotional skills and attributes as well as positive social interactions, quality education, decent work, safe neighbourhoods and community cohesion , among others.
What Steps have been Taken to Promote Mental Health?
- World Mental Health Day is observed on 10th October every year, with the overall objective of raising awareness of mental health issues around the world and mobilising efforts in support of mental health.
- WHO’s Comprehensive Mental Action Plan 2013-2020 was also adopted by the 66 th World Health Assembly.
- It is a compilation of data provided by countries around the world on mental health policies, legislation, financing, human resources, availability and utilization of services and data collection systems. It serves as a guide for countries for the development and planning of mental health services.
- Suicide prevention is a global priority and included in the Sustainable Development Goals (SDG 3.4).
- The Program was re-strategize in 2003 to include two schemes, viz. Modernization of State Mental Hospitals and Up-gradation of Psychiatric Wings of Medical Colleges/General Hospitals.
- District Mental Health Programme (DMHP), 1996 was also launched to provide community mental health services at the primary health care level.
- It has significantly reduced the scope for the use of Section 309 IPC and made the attempt to commit suicide punishable only as an exception.
- Kiran Helpline: In 2020, the Ministry of Social Justice and Empowerment launched a 24/7 toll-free helpline ‘Kiran’ to provide support to people facing anxiety, stress, depression, suicidal thoughts and other mental health concerns.
- Manodarpan Initiative : It is an initiative of the Ministry of Education aimed to provide psychosocial support to students, family members and teachers for their mental health and well-being during the times of Covid-19 pandemic.
- MANAS was endorsed as a national program by the Prime Minister’s Science, Technology, and Innovation Advisory Council (PM-STIAC).
What are the Important Points about Mental HealthCare Act 2017?
- Patient can state on how to be treated or not to be treated for the illness during a mental health situation.
- Right to access mental health care
- Right to free & quality services
- Right to get free medicines
- Right to community living
- Right to protection from cruel, inhuman and degrading treatment
- Right to live in an environment, safe and hygienic, having basic amenities
- Right to legal aid
- No Electroconvulsive Therapy (ECT) without anaesthesia
- This act brought changes in Section 309 of the Indian Penal Code (which criminalized attempted suicide).
- Now, a person who attempts to commit suicide will be presumed to be “suffering from severe stress’’ and shall not be subjected to any investigation or prosecution.
- The act envisages the establishment of Central Mental Health Authority and State Mental Health Authority.
What are the Challenges in Promoting Mental Health?
- High Public Health Burden: An estimated 150 million people across India are in need of mental health care interventions, according to India’s latest National Mental Health Survey 2015-16.
- Low financial resource allocation of just over a percent of GDP on healthcare has created impediments in public access to affordable mental healthcare.
- Loss to Economy: due to delayed or non treatment of mentally ill persons there is loss in terms of human capital and an overall loss to the economy in the form of lost man-days , plus the poor is stressed as most of mental healthcare is in urban areas and are unavailable in primary healthcare centres in rural areas, this increases out of pocket expenditure.
- Demographic Dividend: According to WHO, the burden of mental disorders is maximal in young adults. As most of the population is young (India has more than 50% of its population below the age of 25) so it requires a special focus in mental health of youth by the government to reap the benefits arising out of the demographic dividend in India.
- Post-Treatment Gap: There is need for proper rehabilitation of the mentally ill persons post his/her treatment which is currently not present.
- Reluctance on part of family members to seek treatment for the patient has resulted in a massive treatment gap , which further worsens the present mental illness of a person.
- Rise in Severity: Mental health problems, tend to increase during economic downturns, therefore special attention is needed during times of economic distress.
- Prone to Abuse: Mentally ill patients are vulnerable to and usually suffer from physical abuse, sexual abuse, wrongful confinement, even at homes and mental healthcare facilities which is a cause of concern and a gross human right violation.
What Should be the Way Forward?
- Increasing mental healthcare facilities and related infrastructure through more resource allocation in the budget.
- Adequate Mental healthcare professional availability.
- For patients to undertake timely treatment
- To breakdown societal prejudices/ stigma
- To discourage questionable treatment from faith healers.
- For eg. “The Live Love Laugh Foundation” which aims to reduce the stigma, spread awareness and change the way we look at Mental Health.
- There is only one primary healthcare centre for more than 51,000 people in India.
- The World Bank estimates that 90% of all health needs can be met at the primary healthcare level thus more investments are needed in order for patients to get easier, cheaper and faster access to services , plus, training at grass root level for ASHA , ANM, AWW centre workers on how to recognize common to severe mental health problems like schizophrenia, anxiety, depression, and alcohol abuse.
- By forming their self-help groups of carers families along with NGO’s which brings community participation and helps reduction in social stigma associated with mental illness.
- Delivery of services should be sensitive, compassionate and free from stigma and discrimination in public healthcare institutions plus there is need for police sensitization and training regarding recognition of acute mental disorders and undertaking of necessary action to protect the human rights of the mentally ill, his family and his fellow citizens.
India needs a constant stream of funds for educating and creating awareness about mental health and chronic issues around it.
If individuals continue to view mental illness with apprehension and resistance, it will remain difficult for people with mental health concerns to seek the support they require due to the fear of being labelled or judged.
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Q. Pawan is working as an officer in the State Government for the last ten years. As a part of routine transfer, he was posted to another department. He joined in a new office along with five other colleagues. The head of the office was a senior officer conversant with the functioning of the office. As a part of general inquiry, Pawan gathered that his senior officer carries the reputation of being difficult and insensitive person having his own disturbed family life. Initially, all seemed to go well. However, after some time Pawan felt that the senior officer was belittling him and at times unreasonable. Whatever suggestions given or views expressed by Pawan in the meetings were summarily rejected and the senior officer would express displeasure in the presence of others. It became a pattern of boss’ style of functioning to show him in bad light highlighting his shortcomings and humiliating publicly. It became apparent that though there were no serious work-related problems/shortcomings, the senior officer was always on one pretext or the other and would scold and shout at him. The continuous harassment and public criticism of Pawan resulted in loss of confidence, self-esteem and equanimity. Pawan realised that his relation with his senior officer was becoming more toxic and due to this, he felt perpetually tensed, anxious and stressed. His mind was occupied with negativity and caused him mental torture, anguish and agony. Eventually, it badly affected his personal and family life. He was no longer joyous, happy and contented even at home. Rather without any reason he would lose his temper with his wife and other family members. The family environment was no longer pleasant and congenial. His wife who was always supportive to him also became a victim of his negativity and hostile behaviour. Due to harassment and humiliation suffered by him in the office, comfort and happiness virtually vanished from his life. Thus, it damaged his physical and mental health. (2021)
(a) What are the options available with Pawan to cope with the situation?
(b) What approach Pawan should adopt for bringing peace,tranquility and congenial environment in the office and home?
(c) As an outsider, what are your suggestions for both boss and subordinate to overcome this situation and for improving the work performance, mental and emotional hygiene?
(d) In the above scenario, what type of training would you suggest for officers at various level sin the government offices?


IMAGES
VIDEO
COMMENTS
The healthcare industry in India includes hospitals, medical tourism, health insurance, medical equipment, telemedicine, outsourcing, clinical trials, and medical gadgets. The public and private sectors make up the two main components of India's healthcare delivery system. The Scenario of the Health Sector in India. Health Infrastructure.
In the Economic Survey of 2022, India's public expenditure on healthcare stood at 2.1% of GDP in 2021-22 against 1.8% in 2020-21 and 1.3% in 2019-20. In FY21, gross direct premium income underwritten by health insurance companies grew 13.3% YoY to Rs. 58,572.46 crore (USD 7.9 billion).
India will have about 50 clusters for faster clinical testing of medical devices to boost product development and innovation. As of 2021, the Indian healthcare sector is one of India's largest employers as it employs a total of 4.7 million people. The sector has generated 2.7 million additional jobs in India between 2017-22 - over 500,000 new ...
The healthcare sector in India is expected to grow to reach a size of $50 bn by 2025. The digital healthcare market is expected to more than 20% by 2023. The Telemedicine market is the maximum potential eHealth segment in India, which is expected to touch $5.4 Bn by 2025. In the Economic Survey of 2022, India's public expenditure on ...
Planning. This editorial is based on " Shaping India's path to inclusive health care " which was published in The Hindu on 08/04/2024. The article explains how India's health equity issues stem from a complex interplay of factors such as socioeconomic status, education, gender, geography, and access to healthcare services.
Status of India's Health Sector: Increase in healthcare expenditure by a massive 73% ( from 2.73 lakh cr in 2019-20 to 4.72 lakh cr in 2021-22) New missions: e-sanjeevani, Ayushman Bharat Digital Mission, National Digital Health Mission etc. Over 3+ mn requirement of doctors and nurses by 2025. Over 2000 HealthTech Start-ups (including 4 ...
increased from 79% to 89% in India and in rural areas around 87% births being delivered in institutions and the same is 94% in urban areas. Fully immunized. more than three-fourths (77%) children age 12-23 months, compared with 62% in NFHS-4. Level of stunting. declined from 38% to 36%.
Rs. 69,000 crores (US$ 9.87 billion) outlay announced for the health sector that is inclusive of Rs. 6,400 crore (US$ 915.72 million) for PMJAY in Union Budget 2020-21. The Government of India aims to increase healthcare spending to 3% of the Gross Domestic Product (GDP) by 2022.
Strengthening Primary Healthcare. One of the key strategies to address health equity in India is strengthening primary healthcare services, particularly in rural and underserved areas. This includes improving the availability and accessibility of primary care facilities, enhancing the skills and capacity of frontline healthcare workers, and ...
Low health workforce density - India's public system has a shortage of nurses. The ratio of 0.6 nurses per doctor while the World Health Organization specification is three nurses per doctor. 80:20 Rule - Only 20% of people can afford modern health care, 40% cannot afford it at all and the other 40%, the non-poor, pay with difficulty.
The National Health Mission was allotted Rs. 37,000 crore (US$ 4.84 billion). Ayushman Bharat - Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) was allotted Rs. 6,412 crore (US$ 840.32 million). In November 2021, the Government of India, the Government of Meghalaya and the World Bank signed a US$ 40-million health project for the state of Meghalaya.
Context: Recently the Government of India and World Bank signed two complimentary loans worth $1 billion to support and enhance India's healthcare infrastructure.. About India's healthcare sector at glance: In the Economic Survey of 2022, India's public expenditure on healthcare stood at 1% of GDP in 2021-22 against 1.8% in 2020-21 and 1.3% in 2019-20.
Medical Tourism: India ranks 10th in Medical Tourism Index (MTI) for 2020-2021 out of 46 destinations in the world. Future Projection: The hospital sector in India was valued at INR 7940.87 Bn in FY21 in terms of revenue & is expected to reach INR 18,348.78 Bn by FY 2027, growing at a CAGR of 18.24%. The Indian medical tourism market was valued ...
The consequences of neglecting primary health care are manifold, including high maternal and infant mortality rates, prevalence of communicable diseases, and limited healthcare-seeking behavior among marginalized populations. A 2019 study by the National Health Authority (NHA) found that in rural Madhya Pradesh, nearly 18% of the population ...
Indian Health Sector Data: Budget Spending and Insurance Levels. The public expenditure on the health sector remains a dismal show of only around 1.4% of the GDP. The investment in health research has been low with a modest rate of 1% of the total public health expenditure. Insurance coverage remains low as per the latest NSSO reports over 80% ...
Healthcare scenario in India. The World Health Organization defines health as a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. At present, India's health care system consists of a mix of public and private sector providers of health service s. Networks of health care facilities at ...
In 2023, Prime Minister Narendra Modi launched the National Sickle Cell Anaemia Elimination Mission, with the goal of eradicating sickle cell disease as a public health issue by 2047. India bears the second-largest global burden of the disease, affecting over a million people. The majority of cases are concentrated in the tribal regions of Odisha, Jharkhand, Chhattisgarh, Madhya Pradesh, and ...
Achieving Universal Health Care. 21 Mar 2023. 10 min read. Tags: GS Paper - 2. Health. Government Policies & Interventions. This editorial is based on "Moving forward with a newer concept of Universal Health Care" which was published in the Hindu on 20/03/2023. It discusses the issues with Universal Health Care/Coverage and ways to achieve it.
According to the WHO, mental illness makes about 15% of the total disease conditions around the world. In 2019, India's suicide rate was at 12.9 per 1,00,000 persons. This was higher than the regional average of 10.2 and the global average of 9.0. Suicide has become the leading cause of death among those aged 15-29 in India.
Health is a state subject, the Central Government supplements the efforts of the State Governments in delivery of health services through various schemes for primary, secondary, and tertiary care.. By 2025, the Government of India is planning to increase the expenditure on Health care to 2.5% of the GDP. In the Union Budget 2020-21, the Ministry of Health and Family Welfare was allocated a ...
Parameswaran Iyer: Parameswaran Iyer is an Indian civil servant and currently serves as the Executive Director at the World Bank Group, representing Bangladesh, Bhutan, India, and Sri Lanka. Previously, Mr. Iyer was the Chief Executive Officer of NITI Aayog, India's National Think Tank, from July 2022 to February 2023.He is also the driving force behind the Swachh Bharat Abhiyan, a campaign ...
Public Health System In India. This article is based on "Reset and reform" which was published in The Indian Express on 29/04/2020. It talks about the importance and challenges of the public health system amid Covid-19 pandemic. Contrary to the popular notion about India's Public health systems being inefficient and ineffective, it is ...
The Commission's online survey showed that a whopping 27.8 per cent of undergraduate students had mental-health conditions and 31.3 per cent of postgraduate students had suicidal thoughts. A study by the National Institute of Mental Health and Neurosciences (NIMHANS) found that 23 percent of school children in India have mental health problems.
India's current health expenditure stands at approximately 3.2% of its GDP, significantly lower than the average of around 5.2% observed among Lower- and Middle-Income Countries (LMIC). Lack of Financial Protection. Despite schemes like Janani Shishu Suraksha Karyakram, high out-of-pocket expenditure for deliveries, particularly in urban areas.
The Health Dynamics of India 2022-23 report released by the Union health ministry Monday showed that only 4,413 specialist doctors of the requisite 21,964 needed in CHCs in March 2023 were available—a shortfall of 17,551 or 79.9 percent. There are 5,491 rural CHCs in 757 districts of the country. Show Full Article
Challenges associate with privatization of healthcare: Privatization will increase the gap between rich and poor which will encourage survival of the richest, which cannot be the goal of any civilized society. The public hospitals offer subsidized and other free services which makes most of the people move away from private hospitals.
What are the Challenges in Promoting Mental Health? High Public Health Burden: An estimated 150 million people across India are in need of mental health care interventions, according to India's latest National Mental Health Survey 2015-16. Lack of Resources: Low proportion of mental health workforce in India (per 100,000 population) include psychiatrists (0.3), nurses (0.12), psychologists ...