

COPD Case Study: Patient Diagnosis and Treatment (2024)
by John Landry, BS, RRT | Updated: Oct 15, 2024
Chronic obstructive pulmonary disease (COPD) is a progressive lung condition affecting millions worldwide, primarily linked to smoking. It is marked by a persistent reduction in airflow that gradually worsens, making it increasingly difficult to breathe.
Common symptoms of COPD include chronic coughing, wheezing, shortness of breath, and chest tightness, all of which can severely affect an individual’s daily life and overall well-being .
This case study explores the diagnosis and treatment of an adult patient presenting with classic signs and symptoms of COPD, providing insight into effective management strategies for this challenging condition.
25+ RRT Cheat Sheets and Quizzes
Get instant access to 25+ premium quizzes, mini-courses, and downloadable cheat sheets for FREE.
COPD Clinical Scenario
A 56-year-old male presents to the ER with increased work of breathing. He reported feeling mildly short of breath upon waking, which worsened significantly after climbing several flights of stairs. Upon arrival, the patient was unable to speak in full sentences due to severe dyspnea. His wife, accompanying him, disclosed that he has a history of liver failure, is allergic to penicillin, and has a 15-pack-year smoking history. She also mentioned that he works as a cabinet maker, frequently exposed to fine dust and debris in his workplace.
Physical Findings
- Pupils equal and reactive to light
- Alert and oriented
- Breathing through pursed lips
- Trachea midline, no jugular venous distention
Vital Signs
- Heart rate: 92 beats/min
- Respiratory rate: 22 breaths/min
Chest Assessment
- Increased anterior-posterior chest diameter (barrel chest)
- Bilateral chest expansion present
- Prolonged expiratory phase with diminished breath sounds upon auscultation
- Subcostal retractions observed
- No tactile fremitus on chest palpation
- Chest percussion reveals increased resonance
- Abdomen soft and non-tender
- No distention
Extremities
- Capillary refill time: 2 seconds
- Digital clubbing observed in fingertips
- No pedal edema
- Skin appears jaundiced
ABG Results
- PaCO2: 59 mmHg
- HCO3: 30 mEq/L
- PaO2: 64 mmHg
Chest X-ray
- Flattened diaphragm
- Increased retrosternal air space
- Dark lung fields
- Slight right ventricular hypertrophy
- Narrow heart silhouette
- RBC: 6.5 million/mm³
- Hb: 19 g/dL
Based on the clinical presentation, lab results, and radiology findings, the patient is highly likely to have chronic obstructive pulmonary disease (COPD).
Key indicators supporting this diagnosis include:
- Barrel-shaped chest
- Tachypnea with prolonged expiratory time
- Diminished breath sounds
- Use of accessory muscles during breathing
- Digital clubbing
- Pursed-lip breathing
- History of significant smoking exposure
- Occupational exposure to dust
Note: These findings are consistent with advanced COPD, requiring immediate intervention to manage symptoms and prevent further progression.
The primary goal of initial treatment for this patient is to correct hypoxemia while minimizing the risk of oxygen-induced hypercapnia, a concern in patients with COPD. The use of low-flow oxygen is recommended to carefully manage oxygen levels.
It’s acceptable to begin with a nasal cannula at 1–2 L/min, but it’s often more precise to use an air-entrainment mask for COPD patients, as it delivers an exact FiO2.
Regardless of the method, oxygen therapy should always start with the lowest possible FiO2 that maintains adequate oxygenation, adjusting as needed based on the patient’s response.
Example Scenario
Suppose you initiate oxygen therapy with an FiO2 of 28% using an air-entrainment mask, but after no improvement, you increase it to 32%. Initially, the patient’s SpO2 was 84%, but it has now dropped to 80%, with worsening retractions. The patient remains in a tripod position, showing signs of increased respiratory effort, including pursed-lip breathing. A repeat arterial blood gas (ABG) reveals a PaCO2 of 65 mmHg and a PaO2 of 59 mmHg.
Recommended Next Steps
The patient is exhibiting increasing signs of respiratory distress, with a rising PaCO2 and worsening hypoxemia despite supplemental oxygen. These ABG results confirm that the patient requires additional support for both ventilation and oxygenation .
Although mechanical ventilation is generally avoided in COPD patients due to the difficulty of weaning them off, noninvasive ventilation (NIV) , such as BiPAP, is the most appropriate intervention at this point.
BiPAP provides ventilatory assistance while avoiding the need for intubation , helping to improve both oxygenation and carbon dioxide removal.
Note: By applying noninvasive ventilation, you can reduce the patient’s work of breathing, improve gas exchange, and hopefully prevent further deterioration without the complications associated with mechanical ventilation.
Initial BiPAP Settings
For adult patients, the most commonly recommended initial BiPAP settings are as follows:
- IPAP (Inspiratory Positive Airway Pressure): 8–12 cmH2O
- EPAP (Expiratory Positive Airway Pressure): 5–8 cmH2O
- Rate: 10–12 breaths per minute
- FiO2: Based on the patient’s previous oxygen requirements
For instance, in this case, you could initiate BiPAP with the following settings:
- IPAP: 10 cmH2O
- EPAP: 5 cmH2O
- Rate: 12 breaths/min
- FiO2: 32%, matching the previous oxygen level.
Adjusting BiPAP Based on ABG Results
After 30 minutes on BiPAP, an arterial blood gas (ABG) analysis shows acute respiratory acidosis with mild hypoxemia.
This indicates two issues:
- Elevated PaCO2 (carbon dioxide retention)
- Decreased PaO2 (low oxygen levels)
Recommended BiPAP Adjustments
Improving oxygenation.
To increase the patient’s PaO2, you can adjust either the FiO2 or EPAP. Since EPAP functions like PEEP (positive end-expiratory pressure), increasing it will improve oxygenation by preventing alveolar collapse.
Recommendation: Increase the EPAP from 5 cmH2O to 7 cmH2O, which will help boost oxygenation.
Since EPAP and IPAP together determine pressure support (the difference between them), increasing EPAP without changing IPAP will reduce the pressure support, which could affect ventilation.
To maintain the same pressure support, it’s important to increase IPAP by the same amount as EPAP.
Improving Ventilation
To address the high PaCO2, the focus should be on increasing IPAP. This will enhance the patient’s tidal volume and, in turn, help to blow off more CO2.
Recommendation: Increase the IPAP to 14 cmH2O. This adjustment will improve ventilation, allowing the patient to exhale more CO2 and bring the PaCO2 down.
Final BiPAP Settings After Adjustment:
- IPAP: 14 cmH2O
- EPAP: 7 cmH2O
After making these changes, reassess the patient’s condition . In this scenario, the patient’s ABG and clinical signs should improve, indicating more effective ventilation and oxygenation.
Patient Outcome and Discharge
Two days later, the patient’s condition has improved significantly, and they have successfully been weaned off BiPAP.
Their oxygenation has stabilized, and they no longer require supplemental oxygen. The patient is now ready for discharge.

Home Therapy and Treatment Recommendations
For patients with COPD, home oxygen therapy may be recommended if their PaO2 falls below 55 mmHg or if their SpO2 drops below 88% on more than two occasions within a three-week period.
However, it’s essential to take a conservative approach when administering oxygen therapy to COPD patients to avoid oxygen-induced hypercapnia.
Pharmacological Recommendations
The following pharmacological agents can be considered for long-term management of COPD:
- Short-acting bronchodilators (e.g., Albuterol): Useful for quick relief of acute symptoms.
- Long-acting bronchodilators (e.g., Formoterol): Help maintain airway patency over time, reducing the frequency of exacerbations.
- Anticholinergic agents (e.g., Ipratropium bromide): These provide sustained bronchodilation, especially useful in combination with bronchodilators.
- Inhaled corticosteroids (e.g., Budesonide): Help reduce airway inflammation and decrease the frequency of flare-ups.
- Methylxanthine agents (e.g., Theophylline): Can be used in cases where other therapies are insufficient, though close monitoring is needed due to potential side effects.
Additional Recommendations
- Smoking cessation support : For patients who smoke, quitting is critical. Smoking cessation programs and nicotine replacement therapy can be very effective.
- Bronchial hygiene therapy : To help with secretion clearance, recommend therapies such as positive expiratory pressure (PEP) therapy or other airway clearance techniques.
- Physical activity and diet: Encourage the patient to stay active, as regular exercise improves lung function and overall health. A balanced, healthy diet can also support their recovery and energy levels.
- Infection prevention: Stress the importance of avoiding infections, particularly respiratory infections. The patient should get an annual flu vaccine and possibly a pneumonia vaccine.
- Cardiopulmonary rehabilitation : Some patients may benefit from a structured rehabilitation program that includes supervised exercise and education to improve breathing techniques and physical endurance.
Note: By incorporating these home therapies and lifestyle modifications, the patient’s COPD can be better managed, helping to prevent exacerbations and significantly improve their quality of life.
Final Thoughts
When treating a patient with COPD, there are two essential principles to keep in mind:
- Oxygen management: Always be cautious with the amount of oxygen administered, aiming to keep the FiO2 as low as possible to maintain adequate oxygenation without suppressing the patient’s drive to breathe.
- Noninvasive ventilation preference: Whenever feasible, opt for noninvasive ventilation (e.g., BiPAP) before resorting to intubation and conventional mechanical ventilation. Intubation can lead to prolonged ventilator dependence, making it more challenging to wean COPD patients .
Additionally, as the patient approaches discharge, it’s crucial to ensure they leave with the appropriate medications and home treatments to minimize the risk of readmission.
Proper management at home—including oxygen therapy, bronchodilators , and pulmonary rehabilitation—can greatly improve outcomes. By considering these key points, you can effectively manage COPD and help improve your patient’s quality of life.

Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
- Agarwal AK, Raja A, Brown BD. Chronic Obstructive Pulmonary Disease. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
- Faarc, Kacmarek Robert PhD Rrt, et al. Egan’s Fundamentals of Respiratory Care. 12th ed., Mosby, 2020.
- Rrt, Cairo J. PhD. Pilbeam’s Mechanical Ventilation: Physiological and Clinical Applications. 7th ed., Mosby, 2019.
- Faarc, Gardenhire Douglas EdD Rrt-Nps. Rau’s Respiratory Care Pharmacology. 10th ed., Mosby, 2019.
- Faarc, Heuer Al PhD Mba Rrt Rpft. Wilkins’ Clinical Assessment in Respiratory Care. 8th ed., Mosby, 2017.
- Rrt, Des Terry Jardins MEd, and Burton George Md Facp Fccp Faarc. Clinical Manifestations and Assessment of Respiratory Disease. 8th ed., Mosby, 2019.
Recommended Reading
Epiglottitis scenario: clinical simulation exam (practice problem), guillain barré syndrome case study: clinical simulation scenario, how to prepare for the clinical simulations exam (cse), faqs about the clinical simulation exam (cse), drugs and medications to avoid if you have copd, 7+ mistakes to avoid on the clinical simulation exam (cse), the 50+ diseases to learn for the clinical sims exam (cse).
Chronic obstructive pulmonary disease (COPD)
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Case history
Case history #1.
A 66-year-old man with a smoking history of one pack per day for the past 47 years presents with progressive shortness of breath and chronic cough, productive of yellowish sputum, for the past 2 years. On examination he appears cachectic and in moderate respiratory distress, especially after walking to the examination room, and has pursed-lip breathing. His neck veins are mildly distended. Lung examination reveals a barrel chest and poor air entry bilaterally, with moderate inspiratory and expiratory wheezing. Heart and abdominal examination are within normal limits. Lower extremities exhibit scant pitting edema.
Case history #2
A 56-year-old woman with a history of smoking presents to her primary care physician with shortness of breath and cough for several days. Her symptoms began 3 days ago with rhinorrhea. She reports a chronic morning cough productive of white sputum, which has increased over the past 2 days. She has had similar episodes each winter for the past 4 years. She has smoked 1 to 2 packs of cigarettes per day for 40 years and continues to smoke. She denies hemoptysis, chills, or weight loss and has not received any relief from over-the-counter cough preparations.
Other presentations
Some patients report chest tightness, which often follows exertion and may arise from intercostal muscle contraction. Weight loss, muscle loss, and anorexia are common in patients with severe and very severe COPD. [1] Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. 2024 [internet publication]. https://goldcopd.org/2024-gold-report Other presentations include fatigue, hemoptysis, cyanosis, and morning headaches secondary to hypercapnia. Chest pain and hemoptysis are uncommon symptoms of COPD and raise the possibility of alternative diagnoses. [2] National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Jul 2019 [internet publication]. https://www.nice.org.uk/guidance/ng115
Physical examination may demonstrate hypoxia, use of accessory muscles, paradoxical rib movements, distant heart sounds, lower-extremity edema and hepatomegaly secondary to cor pulmonale, and asterixis secondary to hypercapnia.
Patients may also present with signs and symptoms of COPD complications. These include severe shortness of breath, severely decreased air entry, and chest pain secondary to an acute COPD exacerbation or spontaneous pneumothorax. [1] Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. 2024 [internet publication]. https://goldcopd.org/2024-gold-report [3] Garcia-Pachon E. Paradoxical movement of the lateral rib margin (Hoover sign) for detecting obstructive airway disease. Chest. 2002 Aug;122(2):651-5. http://www.ncbi.nlm.nih.gov/pubmed/12171846?tool=bestpractice.com Patients with COPD often have other comorbidities, including cardiovascular disease, skeletal muscle dysfunction, metabolic syndrome and diabetes, osteoporosis, depression, anxiety, lung cancer, gastroesophageal reflux disease, bronchiectasis, obstructive sleep apnea, and cognitive impairment. [1] Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. 2024 [internet publication]. https://goldcopd.org/2024-gold-report [4] Morgan AD, Rothnie KJ, Bhaskaran K, et al. Chronic obstructive pulmonary disease and the risk of 12 cardiovascular diseases: a population-based study using UK primary care data. Thorax. 2018 Sep;73(9):877-9. http://www.ncbi.nlm.nih.gov/pubmed/29438071?tool=bestpractice.com [5] Maltais F, Decramer M, Casaburi R, et al; ATS/ERS Ad Hoc Committee on Limb Muscle Dysfunction in COPD. An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014 May 1;189(9):e15-62. https://www.atsjournals.org/doi/10.1164/rccm.201402-0373ST http://www.ncbi.nlm.nih.gov/pubmed/24787074?tool=bestpractice.com
One UK study found that 14.5% of patients with COPD had a concomitant diagnosis of asthma, whereas a global meta-analysis estimated the pooled prevalence of asthma in patients with COPD to be 29.6% (range: 12.6% to 55.5%). [6] Nissen F, Morales DR, Mullerova H, et al. Concomitant diagnosis of asthma and COPD: a quantitative study in UK primary care. Br J Gen Pract. 2018 Nov;68(676):e775-82. https://bjgp.org/content/68/676/e775 http://www.ncbi.nlm.nih.gov/pubmed/30249612?tool=bestpractice.com [7] Hosseini M, Almasi-Hashiani A, Sepidarkish M, et al. Global prevalence of asthma-COPD overlap (ACO) in the general population: a systematic review and meta-analysis. Respir Res. 2019 Oct 23;20(1):229. https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-019-1198-4 http://www.ncbi.nlm.nih.gov/pubmed/31647021?tool=bestpractice.com
Use of this content is subject to our disclaimer
Log in or subscribe to access all of BMJ Best Practice
Log in to access all of bmj best practice, help us improve bmj best practice.
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.
LOGIN
Annual Report
- Board of Directors
- Nomination Process
- Organizational Structure
- ATS Policies
- ATS Website
- MyATS Tutorial
- ATS Experts
- Press Releases
Member Newsletters
- ATS in the News
- ATS Conference News
- Embargo Policy
ATS Social Media
Breathe easy podcasts, ethics & coi, health equity, industry resources.
- Value of Collaboration
- Corporate Members
- Advertising Opportunities
- Clinical Trials
- Financial Disclosure
In Memoriam
Global health.
- International Trainee Scholarships (ITS)
- MECOR Program
- Forum of International Respiratory Societies (FIRS)
- 2019 Latin American Critical Care Conference
Peer Organizations
Careers at ats, affordable care act, ats comments and testimony, forum of international respiratory societies, tobacco control, tuberculosis, washington letter.
- Clinical Resources
- ATS Quick Hits
- Asthma Center
Best of ATS Video Lecture Series
- Coronavirus
- Critical Care
- Disaster Related Resources
- Disease Related Resources
- Resources for Patients
- Resources for Practices
- Vaccine Resource Center
- Career Development
- Resident & Medical Students
- Junior Faculty
- Training Program Directors
- ATS Reading List
- ATS Scholarships
- ATS Virtual Network
ATS Podcasts
- ATS Webinars
- Professional Accreditation
Pulmonary Function Testing (PFT)
- Calendar of Events
Patient Resources
- Asthma Today
- Breathing in America
- Fact Sheets: A-Z
- Fact Sheets: Topic Specific
- Patient Videos
- Other Patient Resources
Lung Disease Week
Public advisory roundtable.
- PAR Publications
- PAR at the ATS Conference
Assemblies & Sections
- Abstract Scholarships
- ATS Mentoring Programs
- ATS Official Documents
- ATS Interest Groups
- Genetics and Genomics
- Medical Education
- Terrorism and Inhalation Disasters
- Allergy, Immunology & Inflammation
- Behavioral Science and Health Services Research
- Clinical Problems
- Environmental, Occupational & Population Health
- Pulmonary Circulation
- Pulmonary Infections and Tuberculosis
- Pulmonary Rehabilitation
- Respiratory Cell & Molecular Biology
- Respiratory Structure & Function
- Sleep & Respiratory Neurobiology
- Thoracic Oncology
- Joint ATS/CHEST Clinical Practice Committee
- Clinicians Advisory
- Council of Chapter Representatives
- Documents Development and Implementation
- Drug/Device Discovery and Development
- Environmental Health Policy
- Ethics and Conflict of Interest
- Health Equity and Diversity Committee
- Health Policy
- International Conference Committee
- International Health
- Members In Transition and Training
- View more...
- Membership Benefits
- Categories & Fees
- Special Membership Programs
- Renew Your Membership
- Update Your Profile
- ATS DocMatter Community
- Respiratory Medicine Book Series
- Elizabeth A. Rich, MD Award
- Member Directory
- ATS Career Center
- Welcome Trainees
- ATS Wellness
- Thoracic Society Chapters
- Chapter Publications
- CME Sponsorship
Corporate Membership
Clinical cases, professionals.
- Respiratory Health Awards
- Clinicians Chat
- Ethics and COI
- Pulmonary Function Testing
- ATS Resources

The ATS Clinical Cases are a series of cases devoted to interactive clinical case presentations on all aspects of pulmonary, critical care and sleep medicine. They are designed to provide education to practitioners, faculty, fellows, residents, and medical students in the areas of pulmonary, critical care and sleep medicine.
Currently, we are not accepting new cases for this series, as there are several other venues for publishing cases. For cases that can be written as brief, image-based quesitons, consider submitting them as to Quick Hits . For other cases, please contact your assembly web director regarding other opportunities to publish or highlight cases.
ATS Clinical Cases Designated by the Assemblies
Assembly on Allergy, Immunology, and Inflammation
- A Case Of Diffuse Miliary Pulmonary Infiltrates In A 35 Year-Old Man
- The Mighty Eosinophil
- Persistent Dyspnea in a Patient with Down’s Syndrome
- A 20 Year-Old with a Mediastinal Mass
- A Transsexual with Acute Dyspnea and Diffuse Infiltrates
- Use of Endobronchial Ultrasound to Diagnose an Incidental Lung Nodule
- Persistent Dyspnea Despite Maximal Medical Therapy in COPD
- Uncontrolled asthma, recurrent rhinosinusitis, and infertility in a young woman
- A case of progressive dyspnea and abnormal chest x-ray
- A 27 year old with a non resolving cavitary lung lesion
- ARDS Following Autologous Hematopoietic Stem Cell Transplantation for Multiple Myeloma
- Sudden Onset of Wheezing at Work
- Difficult-to-Control Asthma in a 49-Year-Old Man
- Dyspnea and wheezing in a pregnant patient
- Mediastinal Lymphadenopathy and Interstitial Lung Disease in a Cancer Patient
- Diffuse Infiltrates Following Hematopoietic Stem Cell Transplantation
- Difficult-to-control asthma in 13-year-old boy
- Stable Mild Persistent Asthma in a Young Adult
- Dyspnea in a college athlete
Assembly on Behavioral Science and Health Services Research
- Challenges in Caring for the Child with Asthma: Enlisting Community Services
- A 60-Year-Old Man with Acute Respiratory Failure and Mental Status Changes
- Young Man with Recent Onset Hypertension and Acute Onset Dyspnea
- Hoarseness and Hemoptysis in a 28-Year-Old Pregnant Woman
Assembly on Critical Care
- 60-Year-Old Man with Non-resolving Pneumonia
- Egg Shell Calcifications in a 69 Year Old Woman
- Cavitating Lung Lesion in a 59 year-old man.
- Intracerebral Hemorrhage in a Young Adult Male Patient
- A 39 Year Old Woman with Fever and Myalgia
- Septic Shock Following an Ulcerative Colitis Flare
- A 67-Year-Old Man with Massive Hemoptysis
- Chest Pain After Sexual Intercourse
- Liver dysfunction and severe lactic acidosis in a previously healthy man
Assembly on Clinical Problems
- Clinical Considerations for Individuals with Cystic Fibrosis
- An Unusual Cause of Chest Pain
- A 5 year old girl with Prader-Willi syndrome and worsening snoring during growth hormone therapy
- Dry Cough and Clubbing in a 45-Year-Old Woman
- Near-Complete Opacification of the Right Hemithorax
- Sudden Onset Chest Pain in a Young Man
- Intrapulmonary Shunting Through Tumor Causing Refractory Hypoxemia
Assembly on Environmental, Occupational and Population Health
- Progressive Dyspnea in an Appalachian Coal Miner
- Workplace Spirometry: Early Detection Benefits Individuals, Worker Groups and Employers
- “Horse play and the Lung” – a possible cobalt effect?
- Nonspecific Interstitial Pneumonitis or Hypersensitivity Pneumonitis?
Assembly on Microbiology, Tuberculosis and Pulmonary Infections
- Acute Respiratory Distress Syndrome Secondary to an Unusual Infection
- A Pregnant Woman with Fever and Respiratory Failure
- Cavitating Lung Lesion and Recurrent Chest Infections
- Bronchiectasis and recurrent pulmonary infections
Assembly on Pediatrics
- A six year-old child with cough and facial swelling
Assembly on Pulmonary Circulation
- A Cystic Fibrosis Patient with Hemoptysis From an Unusual Cause
- A 57 Year Old Woman with Pulmonary Hypertension Suffering Worsening Dyspnea on Endothelin Receptor Antagonist Therapy
- 70- Year-Old Woman with Progressive Dyspnea and Dilated Pulmonary Arteries
- An 18-year-old woman with severe dyspnea, hypoxia and abnormal chest findings
Assembly on Pulmonary Rehabilitation
- Pre- and Postoperative Pulmonary Rehabilitation for a COPD Patient Undergoing Bilateral Lung Transplant
Assembly on Sleep and Respiratory Neurobiology
- Central Hypersomnolence: History is the Key
- Persistent Sleepiness in Obstructive Sleep Apnea
- A case of Sleep Disordered Breathing after Coronary Artery Bypass Graft Surgery.
- Postoperative Respiratory Failure in a Child — A Diagnostic Dilemma
- A Case of “Complex” Sleep Apnea?
- Hypersomnolent, Hypercapnic, and Morbidly Obese
- Sleepy Since Adolescence

The American Thoracic Society improves global health by advancing research, patient care, and public health in pulmonary disease, critical illness, and sleep disorders. Founded in 1905 to combat TB, the ATS has grown to tackle asthma, COPD, lung cancer, sepsis, acute respiratory distress, and sleep apnea, among other diseases.
AMERICAN THORACIC SOCIETY 25 Broadway New York, NY 10004 United States of America Phone: +1 (212) 315-8600 Fax: +1 (212) 315-6498 Email: [email protected]
Privacy Statement | Term of Use | COI Conference Code of Conduct

Clinical Simulation Exam Scenario: COPD Patient Case Study
Here is a case study for students and medical practitioners aimed at providing a clinical simulation exam scenario in patients with COPD.
A COPD case study
The 56-year-old patient presents with a difficulty in breathing. The patient complained of feeling short of breath in the morning upon waking up. The breathlessness became worse after climbing just a few steps. He is too short of breath even while talking and has difficulty in finishing sentences.
His wife has revealed that the patient has a history of hepatic failure and allergy to penicillin. He also has a smoking history of 15 pack-year. His occupation involves building cabinets for which he is constantly required to work around fine dust and debris.
Physical examination
The patient's pupils are equal and reactive and he appears alert and oriented. He also has a pursed-lip pattern of breathing. His trachea is in the midline and there is no jugular venous distension.
The vital parameters of the patient are as follows:
- Heart rate: 92 beats per min
- Respiratory rate: 22 breaths per min
Chest assessment:
- The patient presents with a larger than the normal anterior-posterior (AP) diameter of the chest.
- An equal and bilateral chest expansion is noted.
- The chest auscultation reveals diminished breath sounds and a prolonged expiratory phase
- Palpation does not reveal any tactile fremitus
- Percussion of the chest reveals increased resonance
- Subcostal retractions are need
Per abdomen examination
- The abdomen is soft and tender
- Distension: Not present
Extremities:
- The skin appears to be slightly yellowish
- There is no pitting edema in the legs
- Digital clubbing is noted in the fingertips
Laboratory and radiology findings
- ABG Results: PaCO2 59 mm of Hg, pH 7.35 mm of Hg, PaO2 64 mm of Hg, and HCO3 30 mEq/L
- Chest X-ray: Revealed a flat diaphragm, dark lung fields, increase in the retrosternal space, a narrow heart, and mild hypertrophy of the right ventricle
- Blood tests: Hemoglobin 19 gm per 100 mL, RBC 6.5 mill per m3, and hematocrit value 57%
Based on the medical history of the patient, his symptoms, and physical examination, he is suspected to have Chronic Obstructive Pulmonary Disease (COPD).
What are the key findings from the patient’s medical history and assessment in view of the diagnosis?
Here are some important signs and symptoms the patient has complained of that are common in those suffering from COPD:
- A prolonged expiratory time
- Barrel-shaped chest
- Use of accessory muscles of breathing
- Diminished breath sounds
- Pursed lip breathing
- Digital clubbing
- Exposure to dust at the workplace
- History of smoking
How do the abnormal laboratory findings and radiology results justify the diagnosis of COPD in this patient?
The chest x-ray of the patient has revealed the classic signs of COPD such as hyperextension, a narrow heart, and dark lung fields.
It is important to note that though the patient does not have a history of cor pulmonale, congestive heart failure is very common in patients with COPD. Also, the right ventricle of the patient is hypertrophied. It needs to be brought to the attention of the cardiologist for further investigation and assessment of the heart functions.
The laboratory values such as the increased RBC, hematocrit, and hemoglobin levels also point to the diagnosis of COPD. These levels often increase in response to chronic hypoxemia experienced commonly by COPD patients.
The ABG results of the patient also indicate the possibility of COPD as the interpretation suggests compensated respiratory acidosis with hypoxemia. Compensated blood gas levels indicate an issue that could have existed for an extended duration of time.
Which other tests could be helpful in confirming the diagnosis of COPD?
A series of PFT (pulmonary function tests) can be recommended to assess the lung volumes, functions, and capacities of the patient. This would help to confirm or rule out the diagnosis of COPD and provide insights into the severity of the condition.
Generally, the PFT of COPD patients shows the FEV1:FVC ratio to be lower than 70% and an FEV1 value to be less than 80%.
Treatment of COPD
What is the initial treatment for the patient.
As this patient has COPD, the initial line of treatment could be low-flow oxygen to manage hypoxemia. A nasal cannula at 1 to 2 L/min is often recommended along with the air-entrainment mask to ensure the exact FiO2 supply to the lungs.
The patient may be treated with the lowest possible FiO2. The FiO2 can be titrated later based on how he responds to the oxygen being delivered.
What is the next treatment recommendation?
The recent ABG results have revealed a rise in the PaCO2 levels and a decline in the PaO2 levels. This suggests that the patient needs further treatment with ventilation and oxygenation.
Mechanical ventilation needs to be avoided in COPD patients as much as possible as they often have a difficulty in weaning from the device. So, the most appropriate treatment for this patient could be BiPAP (Bilevel Positive Airway Pressure).
Which drug therapies are recommended?
Home oxygen therapy can be recommended if the PaO2 reduces below 55 mm of Hg or the SpO2 reduces below 88% more than twice in a 3-week period.
Other than these, the patient may be prescribed a short-acting or long-acting bronchodilator, an anticholinergic agent, inhaled corticosteroids, and methylxanthines.
Smoking cessation is critical for all patients who smoke. Nicotine replacement therapy could also be indicated in this case.
During the treatment of a patient with COLD, the amount of oxygen being delivered needs to be kept at the lowest possible for maintaining the correct levels of FiO2. Non-invasive ventilation before conventional mechanical ventilation or intubation may also be helpful in emergency situations.
Medical students and doctors can attend our AARC Approved Live Respiratory CEUs to learn more about similar cases. Our Respiratory Therapy Continuing Education CEUs are aimed at providing a clinical simulation of a range of pulmonary conditions to help you improve your knowledge and skills needed for the management of acute and chronic lung diseases.
If you already created an account with us. Please just sign in. If you need to create an account with us just follow the instructions.
Please enter your email to forgot password.
Already a member? Login
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Understanding of COPD among final-year medical students
Javier mohigefer, carmen calero-acuña, eduardo marquez-martin, francisco ortega-ruiz, jose luis lopez-campos.
- Author information
- Article notes
- Copyright and License information
Correspondence: Javier Mohigefer, Hospital Universitario Virgen del Rocío, Universidad de Sevilla, Avenida Manuel Siurot, s/n, 41013 Seville, Spain, Email [email protected]
Collection date 2018.
The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License ( http://creativecommons.org/licenses/by-nc/3.0/ ). By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed.
Several previous studies have shown a suboptimal level of understanding of COPD among different population groups. Students in their final year of Medicine constitute a population that has yet to be explored. The evaluation of their understanding provides an opportunity to establish strategies to improve teaching processes. The objective of the present study is to determine the current level of understanding of COPD among said population.
A cross-sectional observational study was done using digital surveys given to medical students in their final year at the Universidad de Sevilla. Those surveyed were asked about demographic data, smoking habits as well as the clinical manifestation, diagnosis and treatment of COPD.
Of the 338 students contacted, responses were collected from 211 of them (62.4%). Only 25.2% had an accurate idea about the concept of the disease. The study found that 24.0% of students were familiar with the three main symptoms of COPD. Tobacco use was not considered a main risk factor for COPD by 1.5% of students. Of those surveyed, 22.8% did not know how to spirometrically diagnose COPD. Inhaled corticosteroids were believed to be part of the main treatment for this disease among 51.0% of the students. Results show that 36.4% of respondents believed that home oxygen therapy does not help COPD patients live longer. Only 15.0% considered the Body-mass index, airflow Obstruction, Dyspnea, and Exercise (BODE) index to be an important parameter for measuring the severity of COPD. Giving up smoking was not believed to prevent worsening COPD among 3.4% of students surveyed. Almost half of students (47.1%) did not recommend that those suffering from COPD undertake exercise.
The moderate level of understanding among the population of medical students in their final year shows some strengths and some shortcomings. Teaching intervention is required to reinforce solid knowledge among this population.
Keywords: COPD, knowledge, surveys and questionnaires, students, medical
Introduction
COPD, a disease characterized by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases, 1 is one of the diseases with the greatest impact on world health. There are currently an estimated 328 million people suffering from COPD around the world. 2 The Global Burden of Disease Study underscores that COPD was the sixth leading cause of death in 1990, has been the fourth since 2000 and is expected to be the third by 2020. 3 Furthermore, the underdiagnosis of COPD poses a major challenge. In the EPI-SCAN study, 73% of individuals with irreversible airflow obstruction compatible with COPD were not diagnosed. 4
In this context, it is important for both the population and health professionals to have a good knowledge about this disease as a necessary step to avoiding such high underdiagnostic percentages. Unfortunately, the available evidence suggests that the lack of knowledge about the disease is high among a variety of populations. Studies have been done among patients with varying conditions, 5 among patients with COPD, 6 , 7 among doctors 8 and among the general population, 9 demonstrating suboptimal knowledge about COPD.
Studying disease understanding among final-year medical student population constitutes an especially relevant line of research for public health as it allows us to understand this population’s notions about the disease, which will help to identify weaknesses and, at the same time, allow us to design strategies for health education among this population. In the case of COPD, this information is especially relevant given its importance in epidemiology, clinical manifestation and health management. 10 Furthermore, the study of the medical student population represents an especially relevant niche since they have recently studied the disease and are close to receiving a license to practice medicine in society. 11
The benefits of the population having appropriate knowledge about the disease are clear. On one hand, for the general population, doctor–patient contact is made sooner, increasing the likelihood of earlier treatment with a potential impact on disease prognosis. 12 On the other hand, for students, better education implies lower underdiagnosis, better control and better information for the patients about their disease.
One population that has yet to be explored in this sense is that of medical students. Specifically, students in the final year of Medicine constitute an especially interesting population in the study of knowledge about the disease as they have recently studied the disease and will receive a license to practice medicine in society in a few months. However, until now, medical students’ knowledge about COPD has never been evaluated. Consequently, the objective of this study is to analyze the knowledge final-year medical students have about this disease.
The results of this study will give us the opportunity to take a closer look at the level of knowledge the students have regarding this disease and help to identify areas of improvement and to establish strategies to improve teaching for this disease.
This is a cross-sectional observational study which was done using a survey about the understanding of COPD among a population of medical students in their final year at the Universidad de Sevilla (348 students). Per protocol, we set 200 surveys (58% of the total number of students) as the appropriate limit to obtain an adequate number of surveys to allow us to explore the current situation, keeping in mind an estimated loss of 8% due to surveys which were incorrectly completed or considered incomplete.
Survey content
The questions included on the survey were selected based on previous papers published about knowledge surveys 5 , 9 , 13 and based on the research team’s experience and knowledge about the disease ( Supplementary material ). The format of the questions differed according to the objective of each item. The survey included the following types of questions: multiple choice, true/false, Likert-type scales from 0 to 10 and open questions. The questions were divided into six sections: sociodemographic data about the respondent, the concept of COPD, clinical manifestation, diagnosis, non-pharmacological treatment, and pharmacological treatment. Among the sociodemographic data, respondents were asked about their degree of affinity for Pneumology, being asked to rate it on a scale of 0–10 with 10 being the greatest affinity. The questions about diagnosis were aimed at covering three concepts: the need for the spirometric criterion forced expiratory volume in 1 second (FEV 1 )/forced vital capacity <0.7 to diagnose obstruction, evaluating the severity of the obstruction with spirometry, and evaluating the severity according to the Global Initiative for Obstructive Lung Disease (GOLD) 1 and the national Spanish guidelines for COPD management (GesEPOC) documents. 14
For true/false and multiple-choice questions, 80% correct or higher was considered a suitable result. There were three open questions: briefly define what COPD is, list the main risk factors for COPD, and list the primary symptoms of COPD. To analyze the first, the minimum elements that should appear in the answer were identified in order to consider it valid. In this way, respondents were required to identify three ideas: tobacco exposure, irreversible bronchial obstruction, and pulmonary disease. Expressing the meaning of the acronym COPD, was also evaluated. The definition was considered correct if the three concepts appeared and incorrect if one was missing, and it was noted if the answer was missing two or more concepts but the meaning of the acronym COPD was correctly defined. In the case of the second question, which requires a list, a weighted description of the different indicated answers was made. For the last question, we evaluated whether the three main symptoms (cough, expectoration and dyspnea) were identified and, at the same time, we studied what symptom was described most frequently.
Data collection
The survey was done using the Google Forms tool (Google, Mountain View, CA, USA). Once the survey was created, the URL to access it was sent to the target population using the messaging application WhatsApp (Facebook, Inc., Menlo Park, CA, USA). The period for data collection was December 26, 2015, through February 26, 2016. During this time, a reminder was sent to those students who had not yet responded every two weeks. Participation was voluntary, confidential and anonymous.
This study was carried out in accordance with the principles of the Declaration of Helsinki for research involving human subjects. During the study, no personal data were collected about the participants in the study which would allow them to be identified. The data obtained was kept strictly confidential (Spanish Organic Law 15/1999 on the protection of personal data), and only the principal investigator for the project had access to it. Each case was anonymized and numbered with a code to guarantee data confidentiality. Ethical approval was granted by the Research Ethics Committee of the University Hospitals Virgen Macarena-Virgen del Rocío. Before initially completing the survey, students accessed an information sheet ( Supplementary material ) which specified that the survey was being done in the context of a research project and the answers would not influence their final grade as students. Accordingly, the participants provided informed consent for participation in the survey.
Statistical analysis
The quality of the data was evaluated before completing a statistical analysis. To do so, we transferred the data to the program IBM SPSS Statistics version 24.0 (IBM Corporation, Armonk, NY, USA). The quality analysis of data was done variable by variable, searching for missing, extreme and inconsistent values. Those surveys which were considered to be of insufficient quality were excluded from the analysis. Once the final database was obtained, a descriptive analysis of data was done using the absolute and relative frequencies for the categorical variables and the mean and standard variation in parentheses for the continuous variables. Comparison between groups (gender, tobacco use and affinity) for the subject was done using the chi-square test. In cases of 2×2 tables, the Fisher exact test was applied when the expected frequencies were less than 5 in one of the categories. To study the influence of active tobacco use on the results, habitual and occasional smokers were categorized as active smokers. Comparisons on the importance of the different diseases were done by using the unpaired t -test. The α error was set at 0.05.

Sociodemographic data
The selection of completed surveys is shown in Figure 1 . The study population comprised 348 medical students, of whom 211 (60.6%) completed the survey. After evaluating the quality of the surveys, five were discarded. Consequently, there remained 206 surveys. Participants were students, primarily females (62.6%), and had an average age of 23.3 (0.7) years. With regard to habitual tobacco use, the sample included 167 (81.1%) participants who had never smoked, nine (4.4%) former smokers, 19 (9.2%) occasional smokers and 11 (5.3%) habitual smokers. In terms of affinity for the subject, the sample comprised 30 (14.6%) respondents with a high affinity, 112 (54.4%) with an intermediate affinity, and 64 (31.1%) with a low affinity.
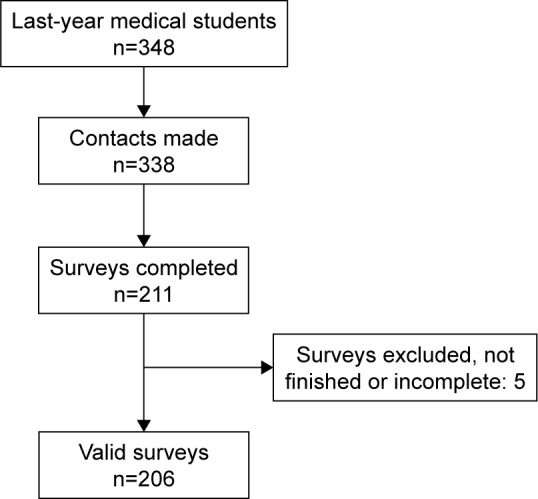
Selection of surveys.
Concept of COPD
The results for the survey items referring to the concept of COPD are summarized in Table 1 . Only 25.2% were able to correctly define the disease. Although before beginning the degree 72.9% had heard of the disease through different means (primarily the media, doctors and the Internet), only 17% admitted they were familiar with it before beginning their studies.
Survey results regarding understanding of COPD
Results are expressed as absolute (relative) frequency or mean (standard deviation), according to the nature of the variable.
p <0.05 for comparison between groups.
p <0.05 for comparison between diseases.
Those surveyed classified COPD as the second most severe disease after ischemic heart disease. The stance on the anti-smoking law was appropriate with a very favorable stance among active smokers (63.3%) and nonsmokers (81.3%), this difference being significant. There was also an association between familiarity with the national strategy for COPD as well as its content and an affinity for the subject ( p =0.042 and p =0.003, respectively). None of those surveyed listed the five risk factors for COPD. A relationship was observed between smokers and nonsmokers with regard to identifying tobacco use as a risk factor for COPD ( Table 1 ).
Due to lack of knowledge, 15% decided not to respond to the question about the contributing biological pathways. The most commonly indicated biological pathway was the participation of inflammatory mediators (proteins) (46.6%), followed by an increase in inflammatory cells (46.1%) and respiratory infections (42.2%).
Clinical manifestation
The results for the survey items referring to the clinical manifestation of COPD are summarized in Table 2 . Of the students surveyed, 34% recognized the symptomatology of the disease (cough, expectoration and dyspnea). With regard to these three symptoms, dyspnea was the answer most frequently given by respondents (80.6%). Only 37.9% knew that expectoration is a symptom of COPD. The identification of chronic bronchitis as a clinical finding and emphysema as a morphological finding was correctly made by just over half of the respondents, mostly females. Interestingly, 76 (36.9%) of those surveyed responded that both chronic bronchitis and emphysema are clinical concepts.
Survey results regarding clinical manifestations of COPD
Results are expressed as absolute (relative) frequencies.
The results for the survey items referring to the diagnosis of COPD are summarized in Table 3 . Although the diagnostic criteria were identified by the majority of participants, the evaluation of obstruction severity with spirometry or according to current documents was fairly poor, being worse among men and active smokers. The questions about the degree of obstruction in spirometry were answered correctly by approximately 50%, and the questions about the GOLD document classification were answered correctly by 65%, while severity evaluation according to GesEPOC was correctly done by less than 20%. When a case of obstruction with FEV 1 >80% was presented, 83 (40.3%) respondents answered that the patient did not suffer from COPD as there was no obstruction. Furthermore, 102 (49.5) participants confused moderate and severe COPD. With regard to the clinical phenotypes of COPD, those surveyed identified more phenotypes than those recognized in the GesEPOC document. 14 As for the evaluation of severity, 141 (68.4%) respondents indicated that the severity according to GesEPOC is determined by the FEV 1 .
Survey results regarding the diagnosis of COPD
Abbreviations: BODE, Body-mass index, airflow Obstruction, Dyspnea, and Exercise; FEV 1 , forced expiratory volume in 1 second; FVC, forced vital capacity; MMEF, maximal mid-expiratory flow; GOLD, Global Initiative for Obstructive Lung Disease; OSA, obstructive sleep apnea.
Non-pharmacological treatment
The results for the survey items referring to non-pharmacological treatment are summarized in Table 4 . With regard to non-pharmacological treatment, 80% of successful answers was only achieved in two questions: the importance of giving up smoking and pneumococcal vaccination. However, the recommendations regarding exercise and the indication for oxygen therapy had a lower response. The indication for oxygen therapy was confused with the concept of respiratory distress by 64 (31.1%) respondents.
Survey results regarding non-pharmacological treatment
Pharmacological treatment
The results for the survey items referring to pharmacological treatment are summarized in Table 5 . The exploratory questions about pharmacological treatment had a correct response rate far from 80%, with the exception of the question about not abandoning treatment when symptoms improve. A higher affinity for the subject correlates to the correct use of corticosteroids ( p =0.033) as well as the appropriate use of long-acting bronchodilators during exacerbations ( p =0.038). It is worrying that 105 (51.0%) of those surveyed thought a combination of inhaled corticosteroid (ICS) and long-acting β 2 -agonist was the primary pharmacological treatment for COPD.
Survey results regarding pharmacological treatment
Abbreviations: GOLD, Global Initiative for Obstructive Lung Disease; LABA, long-acting β 2 -agonist; LAMA, long-acting muscarinic agonist.
This study provides information regarding knowledge about COPD among the population of medical students in their final year of study. The results indicate a moderate level of understanding among this population with notable areas of improvement including aspects regarding diagnosis, characterization and the treatment of patients suffering from the disease. Additionally, this moderate level of understanding is slightly influenced by the respondents’ gender, tobacco use, and affinity for respiratory diseases in some of the aspects evaluated.
There are similar previous experiences in the general population. Specifically, two previous studies have been done in Spain at the national level, 9 , 15 both in the national sphere and among general population. Of these, the CONOCEPOC study 9 recently obtained a total of 6,528 surveys at a 13.1% response rate with representation from every region of the country. Although there is a similar percentage of active smokers (habitual and occasional) in both studies (19.4% in CONOCEPOC vs 14.5% in the present study) with a similar evaluation of COPD severity (8.3 points in CONOCEPOC vs 7.8 in the present study), some of the results differ. In the general population, the main means of hearing about the disease is through the media (39.8% in CONOCEPOC). However, in our sample, although still the main means, this percentage is considerably lower (19.9%) with a slight difference from other surveyed sources of information. The spontaneous knowledge about COPD evaluated by CONOCEPOC (17.0%) could not be verified in our case as spontaneous knowledge has not been analyzed. However, only 44.1% of respondents knew the correct concept or were able to identify the meaning of the acronym COPD. The identification of the respiratory symptoms associated with the disease (dyspnea, cough and expectoration) was similar to the general population in the CONOCEPOC study (81.1%, 29.0% and 10.6%, respectively). The fact that in a population like ours only 37.9% identified expectoration as part of the clinical manifestation of the disease stands out. Finally, the stance on the anti-smoking law was similar in both studies, with a considerable improvement in knowledge about the national strategy for COPD in our survey (4.7% vs 34.0%).
The results of subgroup analysis should be treated with caution. This study was not intended to evaluate the differences between groups, and the results are thus informative. With regard to the gender of respondents, men showed worse identification of the concepts of chronic bronchitis and emphysema and worse identification of mild COPD by spirometry. However, they tended to recommend triple therapy more frequently. The overprescription of triple therapy for COPD treatment currently constitutes a problem in managing the disease in diverse areas of health care. In this sense, this overuse of triple therapy has recently been described in all stages of the disease, 16 including as an initial treatment. 17 Given that ICSs are not innocuous and their side effects are dose-dependent, there is an international call for the rational use of these pharmaceuticals in COPD treatment. 18
In terms of tobacco use, active smokers (habitual and occasional) were less likely to be in favor of the anti-smoking law, less commonly identified tobacco use as a risk factor for COPD and less correctly identified severe COPD by spirometry. These data seem to suggest a different attitude toward the disease. These results reinforce the need to transmit the relationship between tobacco use and COPD to the population in order for tobacco users to be aware of the potential effects tobacco use has on respiratory health. Recently, the literature has indicated that even low-intensity smokers have a higher mortality risk than nonsmokers. 19 With regard to affinity for the subject, those surveyed who indicated a high affinity heard about the disease through the Internet more frequently and provided better answers to some of the survey questions; an expected result.
In the light of these findings, it follows that initiatives for improvement in undergraduate medical education are always welcome. Different initiatives including reinforcing concepts or problem-based learning can be alternatives available for this purpose. 20 , 21
To correctly interpret our results, some methodological considerations must be kept in mind. Participation in the survey was voluntary which may imply a selection bias. Although the study was not based on a study population sample to guarantee the representiveness of the selected sample, the response rate provides a sample size that suggests that the data presented may be a reflection of the reality for students at our university. On the other hand, given the intrinsic limitations in completing a survey, the number of evaluated concepts was limited. Finally, this survey was done at a specific university within a geographical framework and set time frame. It would be ideal for future studies to confirm our findings in other geographic areas and to be completed over time in order to identify teaching processes to improve knowledge about the disease among future doctors.
Our final-year medical students identify COPD as a serious disease, and the evaluation of their knowledge about COPD highlights some areas of improvement. This study identifies the main weaknesses in diagnosis, clinical characterization and treatment. We hope these results will be useful to improve university teaching which will help in appropriately preparing doctors to diagnose and treat COPD in the community.
Acknowledgments
The authors would like to thank the final-year students at the Faculty of Medicine, Universidad de Sevilla, during the academic year 2015–2016, for their generous participation in this study.
The authors report no conflicts of interest in this work.
- 1. Vogelmeier CF, Criner GJ, Martínez FJ, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 report: GOLD executive summary. Arch Bronconeumol. 2017;53(3):128–149. doi: 10.1016/j.arbres.2017.02.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349(9064):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Miravitlles M, Soriano JB, García-Río F, et al. Prevalence of COPD in Spain: impact of undiagnosed COPD on quality of life and daily life activities. Thorax. 2009;64(10):863–868. doi: 10.1136/thx.2009.115725. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. de Queiroz MC, Moreira MA, Jardim JR, et al. Knowledge about COPD among users of primary health care services. Int J Chron Obstruct Pulmon Dis. 2014;10:1–6. doi: 10.2147/COPD.S71152. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Ray SM, Helmer RS, Stevens AB, Franks AS, Wallace LS. Clinical utility of the chronic obstructive pulmonary disease knowledge questionnaire. Fam Med. 2013;45(3):197–200. [ PubMed ] [ Google Scholar ]
- 7. White R, Walker P, Roberts S, Kalisky S, White P. Bristol COPD Knowledge Questionnaire (BCKQ): testing what we teach patients about COPD. Chron Respir Dis. 2006;3(3):123–131. doi: 10.1191/1479972306cd117oa. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Davis KJ, Landis SH, Oh YM, et al. Continuing to Confront COPD International Physician Survey: physician knowledge and application of COPD management guidelines in 12 countries. Int J Chron Obstruct Pulmon Dis. 2014;10:39–55. doi: 10.2147/COPD.S70162. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Soriano JB, Calle M, Montemayor T, Álvarez-Sala JL, Ruiz-Manzano J, Miravitlles M. The general public’s knowledge of chronic obstructive pulmonary disease and its determinants: current situation and recent changes. Arch Bronconeumol. 2012;48(9):308–315. doi: 10.1016/j.arbr.2012.07.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21(1):14–23. doi: 10.1111/resp.12660. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Griffin MF, Hindocha S. Publication practices of medical students at British medical schools: experience, attitudes and barriers to publish. Med Teach. 2011;33(1):e1–e8. doi: 10.3109/0142159X.2011.530320. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Welte T, Vogelmeier C, Papi A. COPD: early diagnosis and treatment to slow disease progression. Int J Clin Pract. 2015;69(3):336–349. doi: 10.1111/ijcp.12522. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Wong CK, Yu WC. Correlates of disease-specific knowledge in Chinese patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:2221–2227. doi: 10.2147/COPD.S112176. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish guidelines for management of chronic obstructive pulmonary disease (GesEPOC) 2017. Pharmacological treatment of stable phase. Arch Bronconeumol. 2017;53(6):324–335. doi: 10.1016/j.arbres.2017.03.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Miravitlles M, de la Roza C, Morera J, et al. Chronic respiratory symptoms, spirometry and knowledge of COPD among general population. Respir Med. 2006;100(11):1973–1980. doi: 10.1016/j.rmed.2006.02.024. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Brusselle G, Price D, Gruffydd-Jones K, et al. The inevitable drift to triple therapy in COPD: an analysis of prescribing pathways in the UK. Int J Chron Obstruct Pulmon Dis. 2015;10:2207–2217. doi: 10.2147/COPD.S91694. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Simeone JC, Luthra R, Kaila S, et al. Initiation of triple therapy maintenance treatment among patients with COPD in the US. Int J Chron Obstruct Pulmon Dis. 2016;12:73–83. doi: 10.2147/COPD.S122013. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Hinds DR, DiSantostefano RL, Le HV, Pascoe S. Identification of responders to inhaled corticosteroids in a chronic obstructive pulmonary disease population using cluster analysis. BMJ Open. 2016;6(6):e010099. doi: 10.1136/bmjopen-2015-010099. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the National Institutes of Health–AARP Diet and Health Study. JAMA Intern Med. 2017;177(1):87–95. doi: 10.1001/jamainternmed.2016.7511. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Nendaz MR, Tekian A. Assessment in problem-based learning medical schools: a literature review. Teach Learn Med. 1999;11(4):232–243. [ Google Scholar ]
- 21. Dolmans DHJM, Loyens SMM, Marcq H, Gijbels D. Deep and surface learning in problem-based learning: a review of the literature. Adv Health Sci Educ Theory Pract. 2016;21(5):1087–1112. doi: 10.1007/s10459-015-9645-6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (428.5 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 07 May 2015
Four patients with a history of acute exacerbations of COPD: implementing the CHEST/Canadian Thoracic Society guidelines for preventing exacerbations
- Ioanna Tsiligianni 1 , 2 ,
- Donna Goodridge 3 ,
- Darcy Marciniuk 4 ,
- Sally Hull 5 &
- Jean Bourbeau 6
npj Primary Care Respiratory Medicine volume 25 , Article number: 15023 ( 2015 ) Cite this article
61k Accesses
11 Altmetric
Metrics details
- Respiratory tract diseases
The American College of Chest Physicians and Canadian Thoracic Society have jointly produced evidence-based guidelines for the prevention of exacerbations in chronic obstructive pulmonary disease (COPD). This educational article gives four perspectives on how these guidelines apply to the practical management of people with COPD. A current smoker with frequent exacerbations will benefit from support to quit, and from optimisation of his inhaled treatment. For a man with very severe COPD and multiple co-morbidities living in a remote community, tele-health care may enable provision of multidisciplinary care. A woman who is admitted for the third time in a year needs a structured assessment of her care with a view to stepping up pharmacological and non-pharmacological treatment as required. The overlap between asthma and COPD challenges both diagnostic and management strategies for a lady smoker with a history of asthma since childhood. Common threads in all these cases are the importance of advising on smoking cessation, offering (and encouraging people to attend) pulmonary rehabilitation, and the importance of self-management, including an action plan supported by multidisciplinary teams.
Similar content being viewed by others

Diagnostic spirometry in COPD is increasing, a comparison of two Swedish cohorts
Phenotype and management of chronic obstructive pulmonary disease patients in general population in China: a nationally cross-sectional study

Cardiovascular predictors of mortality and exacerbations in patients with COPD
Case study 1: a 63-year-old man with moderate/severe copd and a chest infection.
A 63-year-old self-employed plumber makes a same-day appointment for another ‘chest infection’. He caught an upper respiratory tract infection from his grandchildren 10 days ago, and he now has a productive cough with green sputum, and his breathlessness and fatigue has forced him to take time off work.
He has visited his general practitioner with similar symptoms two or three times every year in the last decade. A diagnosis of COPD was confirmed 6 years ago, and he was started on a short-acting β 2 -agonist. This helped with his day-to-day symptoms, although recently the symptoms of breathlessness have been interfering with his work and he has to pace himself to get through the day. Recovering from exacerbations takes longer than it used to—it is often 2 weeks before he is able to get back to work—and he feels bad about letting down customers. He cannot afford to retire, but is thinking about reducing his workload.
He last attended a COPD review 6 months ago when his FEV 1 was 52% predicted. He was advised to stop smoking and given a prescription for varenicline, but he relapsed after a few days and did not return for the follow-up appointment. He attends each year for his ‘flu vaccination’. His only other medication is an ACE inhibitor for hypertension.
Managing the presenting problem. Is it a COPD exacerbation?
A COPD exacerbation is defined as ‘an acute event characterised by a worsening of the patient’s respiratory symptoms that is beyond normal day-to-day variation and leads to change in medications’. 1 , 2 The worsening symptoms are usually increased dyspnoea, increased sputum volume and increased sputum purulence. 1 , 2 All these symptoms are present in our patient who experiences an exacerbation triggered by a viral upper respiratory tract infection—the most common cause of COPD exacerbations. Apart from the management of the acute exacerbation that could include antibiotics, oral steroids and increased use of short-acting bronchodilators, special attention should be given to his on-going treatment to prevent future exacerbations. 2 Short-term use of systemic corticosteroids and a course of antibiotics can shorten recovery time, improve lung function (forced expiratory volume in one second (FEV 1 )) and arterial hypoxaemia and reduce the risk of early relapse, treatment failure and length of hospital stay. 1 , 2 Short-acting inhaled β 2 -agonists with or without short-acting anti-muscarinics are usually the preferred bronchodilators for the treatment of an acute exacerbation. 1
Reviewing his routine treatment
One of the concerns about this patient is that his COPD is inadequately treated. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) suggests that COPD management be based on a combined assessment of symptoms, GOLD classification of airflow limitation, and exacerbation rate. 1 The modified Medical Research Council (mMRC) dyspnoea score 3 or the COPD Assessment Tool (CAT) 4 could be used to evaluate the symptoms/health status. History suggests that his breathlessness has begun to interfere with his lifestyle, but this has not been formally asssessed since the diagnosis 6 years ago. Therefore, one would like to be certain that these elements are taken into consideration in future management by involving other members of the health care team. The fact that he had two to three exacerbations per year puts the patient into GOLD category C–D (see Figure 1 ) despite the moderate airflow limitation. 1 , 5 Our patient is only being treated with short-acting bronchodilators; however, this is only appropriate for patients who belong to category A. Treatment options for patients in category C or D should include long-acting muscarinic antagonists (LAMAs) or long-acting β 2 -agonists (LABAs), which will not only improve his symptoms but also help prevent future exacerbations. 2 Used in combination with LABA or LAMA, inhaled corticosteroids also contribute to preventing exacerbations. 2
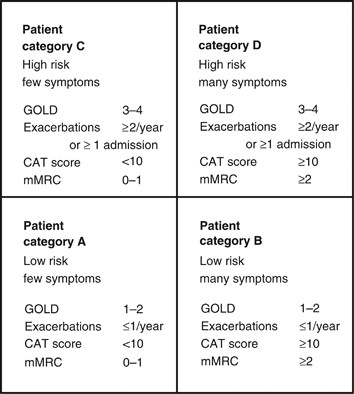
The four categories of COPD based on assessment of symptoms and future risk of exacerbations (adapted by Gruffydd-Jones, 5 from the Global Strategy for Diagnosis, Management and Prevention of COPD). 1 CAT, COPD Assessment Tool; COPD, chronic obstructive pulmonary disease; mMRC, modified Medical Research Council Dyspnoea Scale.
Prevention of future exacerbations
Exacerbations should be prevented as they have a negative impact on the quality of life; they adversely affect symptoms and lung function, increase economic cost, increase mortality and accelerate lung function decline. 1 , 2 Figure 2 summarises the recommendations and suggestions of the joint American College of Chest Physicians and Canadian Thoracic Society (CHEST/CTS) Guidelines for the prevention of exacerbations in COPD. 2 The grades of recommendation from the CHEST/CTS guidelines are explained in Table 1 .

Decision tree for prevention of acute exacerbations of COPD (reproduced with permission from the CHEST/CTS Guidelines for the prevention of exacerbations in COPD). 2 This decision tree for prevention of acute exacerbations of COPD is arranged according to three key clinical questions using the PICO format: non-pharmacologic therapies, inhaled therapies and oral therapies. The wording used is ‘Recommended or Not recommended’ when the evidence was strong (Level 1) or ‘Suggested or Not suggested’ when the evidence was weak (Level 2). CHEST/CTS, American College of Chest Physicians and Canadian Thoracic Society; COPD, chronic obstructive pulmonary disease; FEV 1 , forced expiratory volume in one second; FVC, forced vital capacity; LABA, long-acting β-agonist; LAMA, long-acting muscarinic antagonist; ICS, inhaled corticosteroids; SAMA, short-acting muscarinic antagonist; SABA, short-acting β-agonist; SM, self-management.
Pharmacological approach
In patients with moderate-to-severe COPD, the use of LABA or LAMA compared with placebo or short-acting bronchodilators is recommended to prevent acute exacerbations (Grades 1B and 1A, respectively). 2 , 6 , 7 LAMAs are associated with a lower rate of exacerbations compared with LABAs (Grade 1C). 2 , 6 The inhaler technique needs to be checked and a suitable device selected. If our patient does not respond to optimizing inhaled medication and continues to have two to three exacerbations per year, there are additional options that offer pulmonary rehabilitation and other forms of pharmacological therapy, such as a macrolide, theophylline, phosphodieseterase (PDE4) inhibitor or N -acetylocysteine/carbocysteine, 2 although there is no information about their relative effectiveness and the order in which they should be prescribed. The choice of prescription should be guided by the risk/benefit for a given individual, and drug availability and/or cost within the health care system.
Non-pharmacological approach
A comprehensive patient-centred approach based on the chronic care model could be of great value. 2 , 8
This should include the following elements
Vaccinations: the 23-valent pneumococcal vaccine and annual influenza vaccine are suggested as part of the overall medical management in patients with COPD. 2 Although there is no clear COPD-specific evidence for the pneumococcal vaccine and the evidence is modest for influenza, the CHEST/CTS Guidelines concur with advice of the World Health Organization (WHO) 9 and national advisory bodies, 10 – 12 and supports their use in COPD patients who are at risk for serious infections. 2
Smoking cessation (including counselling and treatment) has low evidence for preventing exacerbations (Grade 2C). 2 However, the benefits from smoking cessation are outstanding as it improves COPD prognosis, slows lung function decline and improves the quality of life and symptoms. 1 , 2 , 13 , 14 Our patient has struggled to quit in the past; assessing current readiness to quit, and encouraging and supporting a future attempt is a priority in his care.
Pulmonary rehabilitation (based on exercise training, education and behaviour change) in people with moderate-to-very-severe COPD, provided within 4 weeks of an exacerbation, can prevent acute exacerbations (Grade 1C). 2 Pulmonary rehabilitation is also an effective strategy to improve symptoms, the quality of life and exercise tolerance, 15 , 16 and our patient should be encouraged to attend a course.
Self-management education with a written action plan and supported by case management providing regular direct access to a health care specialist reduces hospitalisations and prevents severe acute exacerbations (Grade 2C). 2 Some patients with good professional support can have an emergency course of steroids and antibiotics to start at the onset of an exacerbation in accordance with their plan.
Finally, close follow-up is needed for our patient as he was inadequately treated, relapsed from smoking cessation after a few days despite varenicline, and missed his follow-up appointment. A more alert health care team may have been able to identify these issues, avoid his relapse and take a timely approach to introducing additional measures to prevent his recurrent acute exacerbations.
Case study 2: A 74-year-old man with very severe COPD living alone in a remote community
A 74-year-old man has a routine telephone consultation with the respiratory team. He has very severe COPD (his FEV 1 2 years ago was 24% of predicted) and he copes with the help of his daughter who lives in the same remote community. He quit smoking the previous year after an admission to the hospital 50 miles away, which he found very stressful. He and his family managed another four exacerbations at home with courses of steroids and antibiotics, which he commenced in accordance with a self-management plan provided by the respiratory team.
His usual therapy consists of regular long-acting β 2 -agonist/inhaled steroid combination and a long-acting anti-muscarinic. He has a number of other health problems, including coronary heart disease and osteoarthritis and, in recent times, his daughter has become concerned that he is becoming forgetful. He manages at home by himself, steadfastly refusing social help and adamant that he does not want to move from the home he has lived in for 55 years.
This is a common clinical scenario, and a number of important issues require attention, with a view to optimising the management of this 74-year-old man suffering from COPD. He has very severe obstruction, is experiencing frequent acute flare-ups, is dependent and isolated and has a number of co-morbidities. To work towards preventing future exacerbations in this patient, a comprehensive plan addressing key medical and self-care issues needs to be developed that accounts for his particular context.
Optimising medical management
According to the CHEST/CTS Guidelines for prevention of acute exacerbations of COPD, 2 this patient should receive an annual influenza vaccination and may benefit from a 23-valent pneumococcal vaccine (Grades 1B and 2C, respectively). Influenza infection is associated with greater risk of mortality in COPD, as well as increased risk of hospitalisation and disease progression. 1 A diagnosis of COPD also increases the risk for pneumococcal disease and related complications, with hospitalisation rates for patients with COPD being higher than that in the general population. 10 , 17 Although existing evidence does not support the use of this vaccine specifically to prevent exacerbations of COPD, 1 administration of the 23-valent pneumococcal vaccine is recommended as a component of overall medical management. 9 – 12
Long-term oxygen therapy has been demonstrated to improve survival in people with chronic hypoxaemia; 18 it would be helpful to obtain oxygen saturation levels and consider whether long-term oxygen therapy would be of benefit to this patient.
Even though this patient is on effective medications, further optimisation of pharmacologic therapy should be undertaken, including reviewing administration technique for the different inhaler devices. 19 Maintenance PDE4 inhibitors, such as roflumilast or theophyllines, long-term macrolides (i.e., azithromycin) or oral N -acetylcysteine are potential considerations. Each of these therapeutic options has demonstrated efficacy in preventing future acute exacerbations, although they should be used with caution in this frail elderly man. 2 This patient would benefit from a review of co-morbidities, including a chest X-ray, electrocardiogram, memory assessment and blood tests including haemoglobin, glucose, thyroid and renal function assessments.
Pulmonary rehabilitation, supported self-management and tele-health care
Pulmonary rehabilitation for patients who have recently experienced an exacerbation of COPD (initiated <4 weeks following the exacerbation) has been demonstrated to prevent subsequent exacerbations (Grade 1C). 2 Existing evidence suggests that pulmonary rehabilitation does not reduce future exacerbations when the index exacerbation has occurred more than 4 weeks earlier; 2 however, its usefulness is evident in other important patient-centred outcomes such as improved activity, walking distance and quality of life, as well as by reduced shortness of breath. It would be appropriate to discuss this and enable our patient to enrol in pulmonary rehabilitation.
The patient’s access to pulmonary rehabilitation in his remote location, however, is likely to be limited. Several reports have noted that only one to two percent of people with COPD are able to access pulmonary rehabilitation programmes within Canada, 20 the United States 21 and the United Kingdom. 22 Alternatives to hospital-based pulmonary rehabilitation programmes, such as home-based programmes or programmes offered via tele-health, may be options for this patient. 23 Home-based pulmonary rehabilitation programmes have been found to improve exercise tolerance, symptom burden and quality of life. 24 – 27 Outcomes of a pulmonary rehabilitation programme offered via tele-health have also been found to be comparable to those of a hospital-based programme, 28 and may be worth exploring.
Written self-management (action) plans, together with education and case management, are suggested in the CHEST/CTS guidelines as a strategy to reduce hospitalisation and emergency department visits attributable to exacerbations of COPD (Grade 2B). 2 Our patient has an existing action plan, which has enabled him and his family to manage some exacerbations at home. Although the patient has likely had some education on COPD and its management in the past, on-going reinforcement of key principles may be helpful in preventing future exacerbations.
The self-management plan should be reviewed regularly to ensure the advice remains current. The patient’s ability to use the self-management plan safely also needs to be assessed, given his daughter’s recent observation of forgetfulness and his living alone. Cognitive impairment is being increasingly recognised as a significant co-morbidity of COPD. 29 , 30 Patients who were awaiting discharge from hospital following an exacerbation of COPD were found to perform significantly worse on a range of cognitive functional measures than a matched group with stable COPD, a finding that persisted 3 months later. 29 Cognitive impairment may contribute independently to the risk for future exacerbations by increasing the likelihood of incorrect inhaler device use and failure to adhere to recommended treatments. 29
Given that this patient resides in a remote location, access to case management services that assist in preventing future exacerbations may be difficult or impossible to arrange. Although there is currently insufficient evidence that in general the use of telemonitoring contributes to the prevention of exacerbations of COPD, 2 tele-health care for this remotely located patient has potential to allow for case management at a distance, with minimal risk to the patient. Further study is needed to address this potential benefit.
Assessing for and managing frailty
Recognising this patient’s co-morbid diagnoses of coronary heart disease and osteoarthritis, careful assessment of functional and self-care abilities would be appropriate. Almost 60% of older adults with COPD meet the criteria for frailty. 31 Frailty is defined as a dynamic state associated with decline of physiologic reserves in multiple systems and inability to respond to stressful insults. 32 Frailty is associated with an increased risk for institutionalisation and mortality. 33 , 34 Given the complex needs of those who are frail, screening this patient for frailty would constitute patient-centred and cost-effective care. Frailty assessment tools, such as the seven-point Clinical Frailty Index, 35 may provide structure to this assessment.
Admission to a hospital 50 miles away from our patient’s home last year for an exacerbation was stressful. Since his hospitalisation, this patient has experienced four additional exacerbations that have been managed at home in his remote community. It would be appropriate to explore the patient’s treatment wishes and determine whether the patient has chosen to refuse further hospitalisations. Our patient’s risk of dying is significant, with risk factors increasing the risk of short-term mortality following an exacerbation of COPD (GOLD Stage 4, age, male sex, confusion). 36 Mortality rates between 22 and 36% have been documented in the first and second years, respectively, following an exacerbation, 37 , 38 which also increase with the frequency and severity of hospitalisations. 39
Our patient has refused social help and does not want to be relocated from his home. Ageing in their own home is a key goal of many older adults. 40 , 41 Efforts to ensure that adequate resources to support the patient are available (and to support the daughter who is currently providing a lot of his care) will form an important part of the plan of care.
Case study 3: A 62-year-old woman with severe COPD admitted with an exacerbation
A 62-year-old lady is admitted for the third time this year with an acute exacerbation of her severe COPD. Her FEV 1 was 35% predicted at the recent outpatient visit. She retired from her job as a shop assistant 5 years ago because of her breathlessness and now devotes her time to her grandchildren who ‘exhaust her’ but give her a lot of pleasure.
She quit smoking 5 years ago. Over the years, her medication has increased, as nothing seemed to relieve her uncomfortable breathlessness, and, in addition to inhaled long-acting β 2 -agonist/ inhaled steroid combination and a long-acting anti-muscarinic, she is taking theophylline and carbocysteine, although she is not convinced of their beneficial effect. Oral steroid courses help her dyspnoea and she has taken at least six courses this year: she has an action plan and keeps an emergency supply of medication at home.
A secondary care perspective on the management strategy for this woman
Acute exacerbations of COPD have serious negative consequences for health care systems and patients. The risk of future events and complications, such as hospital admission and poor patient outcomes (disability and reduced health status), can be improved through a combination of non-pharmacological and pharmacological therapies. 2
Evaluation of the patient, risk assessment and adherence to medication
The essential first step in the management of this lady (as for any patient) includes a detailed medical evaluation. Our patient has a well-established diagnosis of COPD with severe airflow obstruction (GOLD grade 3), significant breathlessness that resulted in her retiring from her job, and recurrent exacerbations. She does not have significant co-morbidity, although this requires to be confirmed. Further to the medical evaluation, it is important to assess her actual disease management (medication and proper use) as well as making sure she has adopted a healthy lifestyle (smoking cessation, physical activities and exercise). Does she live in a smoke-free environment? Effect of and evidence for smoking cessation in the prevention of acute exacerbations of COPD is low, but evidence exists for a reduction in cough and phlegm after smoking cessation and less lung function decline upon sustained cessation. With respect to the medication, never assume that it is taken as prescribed. When asking the patient, use open questions such as ‘I would like to hear how you take your medication on a typical day?’ instead of ‘Did you take the medication as prescribed’. Open questions tend to elicit more useful and pertinent information, and invite collaboration. Asking the patient to demonstrate her inhalation technique shows you the way she uses her different inhalation devices.
Optimising the pharmacological therapy
The second step is to assess whether the patient is on optimal treatment to prevent exacerbations. In other words, can we do better helping the patient manage her disease and improving her well-being. As in the previous cases, vaccination, in particular, annual administration of the influenza vaccine, should be prescribed for this lady. We should evaluate other alternatives of pharmacological therapy that could improve symptoms, prevent exacerbations and reduce the use of repeated systemic corticosteroids with their important adverse effects (such as osteoporosis, cataracts, diabetes). Prescribing a PDE4 inhibitor (Grade 2A) or a long-term macrolide (Grade 2A) once a day would be a consideration for this lady. 2 As there is no superiority trial comparing these two medications, our preference will be based on potential side effects, as well as cost and access to treatment. For PDE4 inhibitors, there are limited data on supplemental effectiveness in patients with COPD and chronic bronchitis concurrently using inhaled therapies, and they potentially have side effects such as diarrhoea, nausea, headache and weight loss. The side effects tend to diminish over time, but some patients may have to discontinue the therapy. Long-term macrolides have been studied in COPD patients already treated with inhaled therapies and shown to be effective, although clinicians need to consider in their individual patients the potential for harm, such as prolongation of the QT interval, hearing loss and bacterial resistance. Furthermore, the duration (beyond 1 year) and exact dosage of macrolide therapy (for example, once daily versus three times per week) are unknown.
Making non-pharmacological therapy an essential part of the management
The third step, often neglected in the management of COPD patients, is non-pharmacological therapy. For this lady, we suggest self-management education with a written action plan and case management to improve how she deals with exacerbations (Grade 2B). 2 The expectation will not be to reduce exacerbations but to prevent emergency department visits and hospital admissions. However, despite general evidence of efficacy, 42 not all self-management interventions have been shown to be effective or to benefit all COPD patients 43 , 44 (some have been shown to be potentially harmful 44 ). The effectiveness of any complex intervention such as self-management in COPD critically depends on the health care professionals who deliver the intervention, as well on the patient and the health care system. The patient may not have the motivation or desire to change or to commit to an intensive programme. The individual patient’s needs, preferences and personal goals should inform the design of any intervention with a behavioural component. For this lady, it is essential to apply integrated disease management and to refer the patient to a pulmonary rehabilitation programme. Pulmonary rehabilitation has high value, including reducing the risk for hospitalisation in COPD patients with recent exacerbations (Grade 1C). 2 The most important benefits our patient can expect from participating in structured supervised exercise within pulmonary rehabilitation are improved health status, exercise tolerance and a reduction in dyspnoea (Grade 1A). 2 , 15 Pulmonary rehabilitation programmes provide clinicians with an opportunity to deliver education and self-management skills to patients with COPD, and are well established as a means of enhancing standard therapy to control and alleviate symptoms, optimise functional capacity and improve health-related quality of life.
Case study 4: A 52-year-old lady with moderate COPD—and possibly asthma
A 52-year-old lady attends to discuss her COPD and specifically the problem she is having with exacerbations and time ‘off sick’. She is a heavy smoker, and her progressively deteriorating lung function suggests that she has moderate COPD, although she also has a history of childhood asthma, and had allergic rhinitis as a teenager. Recent spirometry showed a typical COPD flow-volume loop, although she had some reversibility (250 ml and 20%) with a post-bronchodilator FEV 1 of 60% predicted.
She has a sedentary office job and, although she is breathless on exertion, this generally does not interfere with her lifestyle. The relatively frequent exacerbations are more troublesome. They are usually triggered by an upper respiratory infection and can take a couple of weeks to recover. She has had three exacerbations this winter, and as a result her employer is not happy with her sickness absence record and has asked her to seek advice from her general practitioner.
She has a short-acting β 2 -agonist, although she rarely uses it except during exacerbations. In the past, she has used an inhaled steroid, but stopped that some time ago as she was not convinced it was helping.
It is a welcome opportunity when a patient comes to discuss her COPD with a particular issue to address. With a history of childhood asthma, and serial COPD lung function tests, she has probably been offered many components of good primary care for COPD, but has not yet fully engaged with her management. We know that ~40% of people with COPD continue to smoke, and many are intermittent users of inhaled medications. 45 It is easy to ignore breathlessness when both job and lifestyle are sedentary.
Understanding her diagnosis and setting goals
Her readiness to engage can be supported by a move to structured collaborative care, enabling the patient to have the knowledge, resources and support to make the necessary changes. Much of this can be done by the primary care COPD team, including the pharmacist. Regular recall to maintain engagement is essential.
The combination of childhood asthma, rhinitis and a long history of smoking requires diagnostic review. This might include serial peak flows over 2 weeks to look for variability, and a chest X-ray, if not done recently, to rule out lung cancer as a reason for recent exacerbations. Her spirometry suggests moderate COPD, 1 , 46 but she also has some reversibility, not enough to place her in the asthma camp but, combined with her past medical history, being enough to explore an asthma COPD overlap syndrome. This is important to consider as it may guide decisions on inhaled medication, and there is evidence that lung function deteriorates faster in this group. 47 It is estimated that up to 20% of patients have overlap diagnoses, although the exact prevalence depends on the definition. 48
Reducing the frequency of exacerbations
Exacerbations in COPD are debilitating, often trigger hospital admission and hasten a progressive decline in pulmonary function. 2 Written information on interventions that can slow down the course of COPD and reduce the frequency and impact of exacerbations will help to support progressive changes in management.
Smoking cessation
Few people are unaware that cessation of smoking is the key intervention for COPD. Reducing further decline in lung function will slow down the severity of exacerbations. Finding a smoking cessation programme that suits her working life, exploring previous attempts at cessation, offering pharmacotherapy and a non-judgemental approach to further attempts at stopping are crucial.
Immunisations
Many, but not all, exacerbations of COPD are triggered by viral upper respiratory tract infections. Annual flu immunisation is a part of regular COPD care and reduces exacerbations and hospitalisation when flu is circulating (Grade 1B). Pneumococcal immunisation should be offered, although evidence for reducing exacerbations is weak; those with COPD will be at greater risk for pneumococcal infection. 2
Pulmonary rehabilitation
Pulmonary rehabilitation improves symptoms, quality of life and reduces hospital admission. 49 It is most efficacious in patients who are symptomatic (MRC dyspnoea scale 3 and above) and in terms of reducing exacerbations is most effective when delivered early after an exacerbation (Grade 1C). 2 The major hurdle is encouraging patients to attend, with most programmes showing an attrition rate of 30% before the first appointment, and high rates of non-completion. 45 , 50 Effective programmes that maintain the gains from aerobic exercise are more cost-effective than some of the inhaled medications in use (see Figure 3 ). 50
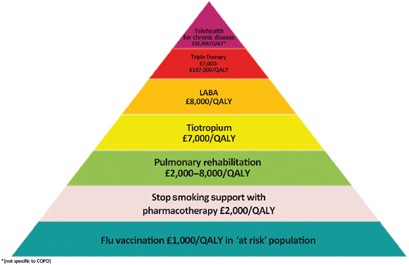
The COPD value pyramid (developed by the London Respiratory Network with The London School of Economics and reproduced with permission from the London Respiratory Team report 2013). 48 This 'value' pyramid reflects what we currently know about the cost per QALY of some of the commonest interventions in COPD. It was devised as a tool for health care organisations to use to promote audit and to ensure adequate commissioning of non-pharmacological interventions. COPD, chronic obstructive pulmonary disease; LABA, long-acting β-agonist; QALY, quality-adjusted life-year.
Inhaled medication is likely to improve our patient’s breathlessness and contribute to a reduction in exacerbation frequency. Currently, she uses only a short-acting β 2 -agonist. One wonders if she has a spacer? How much of the medicine is reaching her lungs? Repeated observation and training in inhaler use is essential if patients are to benefit from expensive medications.
With her history of asthma and evidence of some reversibility, the best choice of regular medication may be a combination of inhaled corticosteroid and a LABA. Guidelines suggest the asthma component in asthma COPD overlap syndrome should be the initial treatment target, 48 and a LABA alone should be avoided. Warn about oral thrush, and the increased risk for pneumonia. 46 If she chooses not to use an inhaled steroid, then a trial of a LAMA is indicated. Both drugs reduce exacerbation rates. 2 , 51
Finally, ensuring early treatment of exacerbations speeds up recovery. 52 Prescribe rescue medication (a 5–7-day course of oral steroids and antibiotic) to be started when symptomatic, and encourage attendance at a post-exacerbation review.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD. Updated 2014. http://www.goldcopd.org. Accessed January 2015.
Criner GJ, Bourbeau J, Diekemper RL, Ouellette DR, Goodridge D, Hernandez P et al. Prevention of acute exacerbations of chronic obstructive pulmonary disease: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest 2015; 147 : 894–942.
Article Google Scholar
Fletcher CM . Standardised questionnaire on respiratory symptoms: a statement prepared and approved by the MRC Committee on the Aetiology of Chronic Bronchitis (MRC breathlessness score). BMJ 1960; 2 : 1665.
Google Scholar
Jones PW, Harding G, Berry P, Wiklund I, Chen W-H, Leidy NK . Development and first validation of the COPD Assessment Test. Eur Respir J 2009; 34 : 648–654.
Article CAS Google Scholar
Gruffydd-Jones K . GOLD guidelines 2011: what are the implications for primary care? Prim Care Respir J 2012; 21 : 437–441.
Chong J, Karner C, Poole P . Tiotropium versus long-acting beta-agonists for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 9 : CD009157.
Cheyne L, Irvin-Sellers MJ, White J . Tiotropium versus ipratropium bromide for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2013; 9 : CD009552.
Bodenheimer T, Wagner EH, Grumbach K . Improving primary care for patients with chronic illness. JAMA 2002; 288 : 1775–1779.
World Health Organization. 23-valent pneumococcal polysaccharide vaccine. WHO position paper. Wkly Epidemiol Rec 2008; 83 : 373–384.
Center for Disease Control and Prevention Pneumococcal vaccination. http://www.cdc.gov/vaccines/vpd-vac/pneumo/ . Accessed January 2015.
Public Health England (2014a) Immunisation against infectious disease - "The Green Book". Chapter 19 - Influenza. https://www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book . Accessed January 2015.
Public Health Agency of Canada. Canadian immunization guide: Pneumococcal vaccine, 2014. http://www.phac-aspc.gc.ca/publicat/cig-gci/p04-pneu-eng.php . Accessed January 2015.
Fletcher C, Peto R . The natural history of chronic airflow obstruction. Br Med J 1977; 1 : 1645–1648.
Hersh CP, DeMeo DL, Al-Ansari E, Carey VJ, Reilly JJ, Ginns LC et al. Predictors of survival in severe, early onset COPD. Chest 2004; 126 : 1443–1451.
Lacasse Y, Goldstein R, Lasserson TJ, Martin S . Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006; (4): CD003793.
Lacasse Y, Wong E, Guyatt GH, King D, Cook DJ, Goldstein RS . Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. Lancet 1996; 348 : 1115–1119.
Lee T, Weaver F, Weiss K . Impact of pneumococcal vaccination on pneumonia rates in patients with COPD and asthma. J Gen Intern Med 2007; 22 : 62–67.
Crockett AJ, Cranston JM, Moss JR, Allpers JH . A review of long-term oxygen therapy for chronic obstructive pulmonary disease. Respir Med 2001; 95 : 437–443.
Newman SP . Inhaler treatment options in COPD. Eur Respir Rev 2005; 96 : 102–108.
Brooks D, Sottana R, Bell B, Hanna M, Laframboise L, Selvanayagarajah S et al. Characterization of pulmonary rehabilitation programs in Canada in 2005. Can Respir J 2007; 14 : 87–92.
Bickford LS, Hodgkin JE, McInturff SL . National pulmonary rehabilitation survey. Update. J Cardiopulm Rehabil 1995; 15 : 406–411.
Yohannes AM, Connolly MJ . Pulmonary rehabilitation programmes in the UK: a national representative survey. Clin Rehabil 2004; 18 : 444–449.
Marciniuk DD, Brooks D, Butcher S, Debigare R, Dechman G, Ford G et al. Optimizing pulmonary rehabilitation in chronic obstructive pulmonary disease – practical issues: a Canadian Thoracic Society Clinical Practice Guideline. Can Respir J 2010; 17 : 159–168.
Guell M, De-Lucas P, Galdiz J, Montemayor T, Rodriguez Gonzalez-Moro J, Gorostiza A . Home vs hospital-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: disease: a Spanish multicentre trial. Arch Bronconeumol 2008; 44 : 512–518.
Maltais F, Bourbeau J, Shapiro S, Lacasse Y, Perrault H, Baltzan M . Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2008; 149 : 869–878.
Puente-Maestu L, Sanz M, Sanz P, Cubillo J, Mayol J, Casaburi R . Comparison of effects of supervised versus self-monitored training programmes in patients with chronic obstructive pulmonary disease. Eur Respir J 2000; 15 : 517–525.
Strijbos J, Postma D, Van-Altena R, Gimeno F, Koeter G . A comparison between an outpatient hospital-based pulmonary rehabilitation program and a home-care pulmonary rehabilitation program in patients with COPD. A follow-up of 18 months. Chest 1996; 109 : 366–372.
Stickland M, Jourdain T, Wong EY, Rodgers WM, Jendzjowsky NG, MacDonald GF . Using Telehealth technology to deliver pulmonary rehabilitation in chronic obstructive pulmonary disease patients. Can Respir J 2011; 18 : 216–220.
Dodd JW, Getov SV, Jones PW . Cognitive function in COPD. Eur Respir J 2010; 35 : 913–922.
Cleutjens FA, Spruit MA, Ponds RW, Dijkstra JB, Franssen FM, Wouters EF et al. Cognitive functioning in obstructive lung disease: results from the United Kingdom biobank. J Am Med Dir Assoc 2014; 15 : 214–219.
Park SK, Richardson CR, Holleman RG, Larson JL . Frailty in people with COPD, using the National Health and Nutrition Evaluation Survey dataset (2003-2006). Heart Lung 2013; 42 : 163–170.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G . Untangling the concepts of disability, frailty and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004; 59 : 255–263.
Lahousse L, Maes B, Ziere G, Loth DW, Verlinden VJ, Zillikens MC et al. Adverse outcome of frailty in the elderly: the Rotterdam Study. Eur J Epidemiol 2014; 29 : 419–427.
Rockwood K, Howlett SE, MacKnight C, Beattie BL, Bergman H, Hebert R et al. Prevalence, attributes and outcomes of fitness and frailty in community-dwelling older adults: report from the Canadian study of health and aging. J Gerontol A Biol Sci Med Sci 2004; 59 : 1310–1317.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173 : 489–495.
Singanayagam A, Schembri S, Chalmers JD . Predictors or mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc 2013; 10 : 81–89.
Almagro P, Calbo E, Ochoa de Echaguen A, Barreiro B, Quintana S, Heredia JL et al. Mortality after hospitalization for COPD. Chest 2002; 121 : 1441–1448.
Groenewegen KH, Schols AM, Wouters EF . Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest 2003; 124 : 459–467.
Soler-Cataluna JJ, Martinez-Garcia MA, Sanchez PR, Salcedo E, Navarro M, Ochando R . Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005; 60 : 925–931.
Ball MM, Perkins MM, Whittington FJ, Connell BR, Hollingsworth C, King SV et al. Managing decline in assisted living: the key to aging in place. J Gerontol B Psychol Sci Soc Sci 2004; 59 : S202–S212.
Pynoos J, Caraviello R, Cicero C . Lifelong housing: the anchor in aging-friendly communities. Generations 2009; 33 : 26–32.
Zwerink M, Brusse-Keizer M, van der Valk PD, Zielhuis GA, Monninkhof EM, van der Palen J et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; 3 : CD002990.
Bucknall CE, Miller G, Lloyd SM, Cleland J, McCluskey S, Cotton M et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ 2012; 344 : e1060.
Fan VS, Gaziano JM, Lew R, Bourbeau J, Adams SG, Leatherman S et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med 2012; 156 : 673–683.
Hull S, Mathur R, Lloyd-Owen S, Round T, Robson J . Improving outcomes for people with COPD by developing networks of general practices: evaluation of a quality improvement project in east London. NPJ Prim Care Respir Med 2014; 24 : 14082.
National Institute of Health and Clinical Excellence. Management of chronic obstructive pulmonary disease in adults in primary and secondary care. Updated 2010. NICE CG101. http://www.nice.org.uk/ . Accessed January 2015.
Gibson PG, Simpson JL . The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax 2009; 64 : 728–735.
Global INitiative for Asthma. Asthma, COPD and asthma-COPD overlap syndromes (ACOS). GINA 2014. http://www.ginasthma.org/documents/14 . Accessed January 2015.
Ries AL, Bauldoff GS, Carlin BW, Casaburi R, Emery CF, Mahler DA et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007; 131 (5 Suppl): 4S–42S.
London Respiratory Team. Take a breath in, keep it in and now try to breathe again. NHS England, 2013. http://www.networks.nhs.uk/nhs-networks/london-respiratory-network . Accessed January 2015.
Guyatt G, Gutterman D, Baumann MH, Addrizzo-Harris D, Hylek EM, Phillips B et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians task force. Chest 2006; 129 : 174–181.
Wilkinson TM, Donaldson GC, Hurst JR, Seemungal TA, Wedzicha JA . Early therapy improves outcomes of exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004; 169 : 1298–1303.
Download references
Acknowledgements
The authors declare that no funding was received.
Author information
Authors and affiliations.
Agia Barbara Health Care Center, Heraklion, Crete, Greece
Ioanna Tsiligianni
Department of Thoracic Medicine, Clinic of Social and Family Medicine, University of Crete, Heraklion, Crete, Greece
Department of Medicine, College of Medicine, University of Saskatchewan, Saskatoon, SK, Canada
Donna Goodridge
Division of Respirology, Critical Care and Sleep Medicine, University of Saskatchewan, Saskatoon, SK, Canada
Darcy Marciniuk
Centre for Primary Care and Public Health, Blizard Institute, Queen Mary University of London, London, UK
Respiratory Epidemiology and Clinical Research Unit, Montreal Chest Institute, McGill University Health Centre, Montréal, QC, Canada
Jean Bourbeau
You can also search for this author in PubMed Google Scholar
Contributions
IT, DG and DM, JB, SH wrote the perspectives on case studies 1, 2, 3 and 4, respectively. The handling editor (Hilary Pinnock) collated and edited the individual sections.
Corresponding author
Correspondence to Jean Bourbeau .
Ethics declarations
Competing interests.
JB declares peer reviewed government grants (for conducting research in COPD self-management 'Living Well with COPD' and the longitudinal population-based Canadian Cohort Obstructive Lung Disease (CanCOLD) study) from Canadian Institute of Health Research Rx&D collaborative programme (Astra Zeneca, Boehringer- Ingelheim, GlaxoSmithKline, Merck, Nycomed, Novartis), Canadian Respiratory Research Network (CRRN), Respiratory Health Network of the FRQS and Research Institute of the MUHC. The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
Reprints and permissions
About this article
Cite this article.
Tsiligianni, I., Goodridge, D., Marciniuk, D. et al. Four patients with a history of acute exacerbations of COPD: implementing the CHEST/Canadian Thoracic Society guidelines for preventing exacerbations. npj Prim Care Resp Med 25 , 15023 (2015). https://doi.org/10.1038/npjpcrm.2015.23
Download citation
Received : 22 February 2015
Accepted : 24 February 2015
Published : 07 May 2015
DOI : https://doi.org/10.1038/npjpcrm.2015.23
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
It seems you are using an outdated browser. Please upgrade to a modern browser to improve your experience on this website.

A COPD Case Study: Jim B.

This post was written by Jane Martin, BA, LRT, CRT, Assistant Director of Education at the COPD Foundation .
We're interested in your thoughts on our latest COPD case study: Jim B., a 68-year-old man here for his Phase II Pulmonary Rehabilitation intake interview.
A bit more about Jim:
Medical history: COPD, FEV1 six weeks ago was 38% of normal predicted, recent CXR shows flattened diaphragm with increased AP diameter, appendectomy age 34, broken nose and broken right arm as a child.
Labs: Lytes plus and CBC all within normal limits.
Physical exam: Breath sounds markedly diminished bilaterally with crackles right lower lobe and wheeze left upper lobe. Visible use of accessory muscles. O2 Saturation 93% room air, 95% O2 on 2lpm. Respiratory rate 24 and shallow, HR 94, BP 150/88, 1+ pitting pedal edema.
Current Medications: Prednisone 10mg q day / DuoNeb q 4 hrs. / Ibuprofen 400mg BID / Tums prn (estimates he takes two per day).
Respiratory history: 80-pack-year cigarette history, quit last year. He has developed a dry, hacking, non-productive cough over the last six months. Had asthma as a child and was exposed to second-hand smoke and cooking fumes while working at family-owned restaurant as a child. Lately, he has noticed slight chest tightness and increased cough when visiting his wife’s art studio.
Family history: Father had emphysema, died at age 69, mother died of breast cancer at 62. Grandfather died at age 57, grandmother died in her 40s of suicide. Six adult children, alive and well.
Previous respiratory admissions: Inpatient admission for six days last winter for acute exacerbation of COPD with bacterial pneumonia requiring 24-hour intubation and mechanical ventilation.
Psych: Jim presents to his Phase II Pulmonary Rehab intake interview appearing disheveled, wearing a sweatshirt, pajama pants and bedroom slippers. He is accompanied by his wife and adult daughter who appear neat, clean and well dressed. Patient states, “I don’t think you people can do anything to help me. I’m only here because they (referring to wife and daughter) made me go.” Jim states that he has been doing less and less at home since discharged from the hospital last winter. Wife states, “He walked outside a little with our grandchildren last Sunday and got so short of breath, he almost collapsed.” Became emotional when saying, “It scared the kids. It tore me up for them to see me that way. Besides that, with this darn shoulder I can’t even pick up the little ones anymore.”

Social: Lives at home with his wife of 43 years who works as an artist. Two out of his six children live within 30 miles of Jim’s home.
Occupation: Building contractor, retired three years ago. Jim states, “I made a good living. All the kids were able to go to college. I was strong. I could work circles around anybody in my crew. And now look at me. I’m tied to that darn breathing machine (referring to nebulizer) and I might as well hang it up.” Wife states, “He used to have all kinds of energy. Now all he does is sit in his chair watching TV, eating potato chips and peanuts.”
Tell us your impressions!
- What co-morbidities should be explored?
- How would you change Jim’s medication regime?
- What psych/social recommendations would you make?
- What other medical disciplines should do a consult on this patient?
- This is a real case. What are your thoughts on what took place following Jim’s pulmonary rehab intake interview?
This page was reviewed on March 3, 2020 by the COPD Foundation Content Review and Evaluation Committee
15 Comments
Join Us on COPD360social
Join the Conversation
Already a Member?
Chronic Obstructive Pulmonary Disease in Older Adults: Part I: Case Study
- PMID: 29969136
- DOI: 10.3928/00989134-20180614-04
Chronic obstructive pulmonary disease (COPD) is a distressing respiratory disease that may greatly impact a patient's quality of life. Although many treatment options exist, the Global Initiative for Chronic Obstructive Lung Disease Guidelines outline management strategies based on severity of daily symptoms and exacerbations. Although it is important to weigh the risks and benefits of medication use, involvement of patients in their overall care plan is imperative to optimal outcomes. According to recent studies, the prevalence of COPD in older adults is increasing, along with the complexity of care due to comorbidities, drug interactions, and side effects. A thorough evaluation of a patient case provides insight into the everyday challenges of COPD management. [Journal of Gerontological Nursing, 44(7), 10-14.].
Copyright 2018, SLACK Incorporated.
- Aged, 80 and over
- Pulmonary Disease, Chronic Obstructive / complications
- Pulmonary Disease, Chronic Obstructive / diagnosis*
- Pulmonary Disease, Chronic Obstructive / therapy*
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
Art & Science Previous Next
Managing a patient with copd and comorbidities: a case study, rachel lucy mitten community matron, peninsula community health community matron service, newquay hospital, newquay, cornwall, england.
This case study provides a critical analysis of the management of a patient with long-term conditions in a community matron service. Particular attention is given to the effect of chronic obstructive pulmonary disease (COPD). The effect of COPD on health and wellbeing, quality of life and hospital admissions is examined, and outcomes are detailed that resulted from the implementation of evidence-based interventions and a case management approach.
Nursing Standard . 30, 13, 46-51. doi: 10.7748/ns.30.13.46.s46
All articles are subject to external double-blind peer review and checked for plagiarism using automated software.
Received: 13 February 2015
Accepted: 29 May 2015
case study - chronic obstructive pulmonary disease - community matron service - comorbidities - complex care - COPD - long-term conditions
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

25 November 2015 / Vol 30 issue 13
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Managing a patient with COPD and comorbidities: a case study
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Effect of Pranayama and Suryanamaskar on Pulmonary Functions in Medical Students
P shyam karthik, m chandrasekhar, kondam ambareesha.
- Author information
- Article notes
- Copyright and License information
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. P. Shaym Karthik, B-7, Cheran Nagar , Kovilpalayam, Pollachi- 642110, Coimbatore, India. Phone : 9790373715, E-mail: [email protected]
Received 2014 Jun 11; Revision requested 2014 Sep 2; Accepted 2014 Oct 13; Issue date 2014 Dec.
Background: Pranayama improved lung functions in numerous studies. Yoga involve isometric contraction and improves skeletal muscle strength. Yoga training improves the strength of expiratory as well as inspiratory muscles.
Aim: The present study is planned to find the effect of pranayama on pulmonary functions in medical students.
Materials and Methods: This study is conducted on 50 students doing lst year M.B.B.S. Consent form has been taken from them. They have been given yoga training 30 min daily for 2 mnth under the guidance of a trained yoga instructor. Vital capacity (VC), Tidal volume (TV), Expiratory Reserve volume (ERV), Breath holding time (BHT), 40 mm endurance, Peak expiratory flow rate (PEFR) are measured before & after yoga training.
Results: VC has increased from 2972 ± 213.151 to 3372 ± 528.7722. TV has increased from 496 ± 84.06347 to 588 ± 150.8863. ERV also shows increase in values from 888 ± 183.303 to 1096 ± 386.7385. BHT also shows increase in values from 33 ± 5.773503 to 58.6 ± 12.78019. 40 mm endurance also shows increase in values from 30.8 ± 5.139715 to 53.52 ± 15.68736. PEFR also shows increase in value from 388.8 ± 15.36229 to 425.2 ± 38.74274.
Conclusion: There is a statistically significant increase in all the above mentioned pulmonary functions following yoga training. Yoga practice can be advocated to improve pulmonary functions in healthy individuals and hence to prevent respiratory diseases in future.
Keywords: BHT, ERV, PEFR, Pranayama, Pulmonary functions, Surya namaskar, TV, 40mm endurance, VC
Introduction
The word yoga means 'union': union of mind, body and spirit - the union between us and the intelligent cosmic spirit of creation- 'the oneness of all things’ [ 1 ] . So pranayama—literally, "control of prana"—isn't just breathing exercises. Through pranayama, you use the breath to affect the constellation of energy that is your bodymind [ 2 ] .
Prana - "life force" or "life energy"
Yama - "discipline" or "control"
Ayama - "expansion", "non-restraint", or "extension
The five principles of yoga are relaxation, exercise (asanas), pranayama (breathing control), nourishing diet, and positive thinking and meditation, pranayama are yogic breathing techniques that increase the capacity of lungs. Pranayama which is control of inspiration and expiration [ 3 ] . The inspiration of prana-vayu is shwasa and expiration is prashwasa and cessation of both is characteristic of pranayama.
Pranayama improves overall performance of the body. The regular practice of pranayama increases chest wall expansion and almost all lung functions. The beneficial effect of different pranayama is well reported and has sound scientific basis [ 3 - 4 ] . Pranayama makes efficient use of abdominal and diaphragmatic muscles and improves the respiratory apparatus [ 5 ] . Yoga strengthens the respiratory musculature due to which chest and lungs inflate and deflate to fullest possible extent and muscles are made to work to maximal extent [ 6 - 7 ] .
Aim and Objectives
Effect of pranayama on pulmonary functions in adults has already been studied by various researchers. This study is done to find out the significant increase in respiratory functions in medical students under pranayama training. The primary purpose of this exploratory analysis is to study the importance of pranayama & surya namaskar on pulmonary functions.
Materials and Methods
Fifty medical students under the age 17-19 y from Meenakshi medical college, Kanchipuram were involved in this study under voluntary basis. The study was performed after obtaining approval from the institutional ethical committee and informed consent from all the subjects. Students who had already undergone yoga training, smokers and alcoholics, students with any disorders, students who had undergone any surgery are abstained from this study. This study was conducted in the Department of Physiology. They were given yoga practice for two months. They were instructed to do yoga for 30 min daily under the guidance of a trained yoga instructor. Parameters such as Vital Capacity (VC), Tidal Volume (TV), Expiratory Reserve Volume (ERV), Breath Holding Time (BHT), 40 mm endurance, Peak Expiratory Flow Rate (PEFR) were assessed before and after two months of yoga training. The parameters were measured using Spirometer and Wright’s expiratory flow meter. The results were compared using student’s paired t test. SPSS software is used for all statistical analysis.
The following yoga practices were given to the subjects daily for two months:
Nadisuddi: Close the right nostril with the right thumb. Now inhale slowly through the left nostril and fill your lungs. After inhalation, close the left nostril with ring finger of right hand. Open the right nostril, exhale slowly. After complete exhalation, again inhale through right nostril and close it with right thumb. Open the left nostril , breathe out slowly. This is one round of Nadisukthi Pranayama. Students were given Nadisuddi training for 5 mins daily for two months [ 8 ] .
Kapalbhati: Kapalbhati Pranayama is a type of breathing exercise that helps you rid of various ailments over a period of time [ 9 ] . "Kapal" means forehead and "bhati" means shining. Kapalabhati is done in a sitting posture [ 10 ] . Focus on "exhaling". Inhale as normal. Exhale and simultaneously contract the abdomen muscles with each exhalation. Students were given Kapalbhati training for 5 mins daily for 2 months.
Bhastrika: Bhastrika is a Sanskrit word which means bellows. In Bhastrika pranayama, the breathing pattern resembles the blowing of bellows. Bhastrika pranayama is all about inhaling and exhaling completely so that your body gets maximum amount of oxygen [ 11 ] . Students were given Bhastrika training for 5 mins daily for 2 months.
Bramhari: The word "Bramhari" comes from the Sanskrit name bhramar which is humming black bee [ 12 ] . The practice of bramhari breathing calms the mind, reduces the stress or fight - flight response. In this pranayama one needs to create a sound while exhaling and inhaling in the throat. The sound is similar to chanting of Om, especially the long mmm. in Omkar. The sound should be deep, steady and smooth. Students were given Bramhari training for 5 mins daily for 2 months.
Pranava Pranayama: The Pranava is the full cosmic Om (or AUM), represented as the three distinct vibratory sounds of 'A' (ah), 'U' (oh) and 'M' (mm). The 'Ahh' sound originating from the solar plexus is related to lower lung breathing [ 13 ] . The 'Ohh' sound originating from the chest region corresponds to mid-chest breathing. The 'Mmm' sound, as it moves upward and transcends its auditory character is associated with upper lung breathing. Students were given Pranava Pranayama training for 5 mins daily for 2 months.
Surya Namsakar: Surya Namaskar has a deep effect in detoxifying the organs through copious oxygenation and has a deeper relaxing effect. It is a series of 12 physical postures [ 14 ] . These alternating backward and forward bending postures flex and stretch the spinal column giving a profound stretch to the whole body [ 15 ] . Students were given Surya Namaskar training for 3 mins daily for 2 months.
OM Chanting was done at the end of the yoga session daily 2 mins for 2 months.
The results of this study demonstrated the beneficial effect of pranayama on pulmonary functions.
The post readings of parameters such as VC, TV, ERV are increased significantly (p<0.005) following yoga practice. This indicates that there is some degree of broncho-dilatation, which is leading to better oxygenation of the alveoli. The post yoga readings of BHT, 40 mm endurance are also statistically improved. Results are shown in [ Table/Fig-1 ].
[Table/Fig-1]:
Effect of pranayama and suryanamaskar on pulmonary functions in Medical students
* Data were mean ± SD , *Significant value for p<0.05
Following the yoga practice, PEFR values are also statistically improved (p<0.005). The increased peak expiratory flow rate might be a consequence of small airway opening in lungs. From the[ Table/Fig-1 ] we observed that there is a statistical improvement in the pulmonary functions following yoga practice. A p-value less than 0.005 was considered as statistically significant.
Pranayama helps in bringing the sympathetic and parasympathetic nervous system into harmony. Through breathing we can influence the nervous system. Pranayama may allow bronchio-dilatation by correcting abnormal breathing patterns & reducing muscle tone of respiratory muscles [ 16 - 18 ].
As shown in [ Table/Fig-1 ], all the parameters show statistically significant improvement with regular practice of yoga. These effects can be explained on the following basis:
Yoga training improves the strength of expiratory as well as inspiratory muscles [ 19 ]. Bhastrika Pranayama is a bellows type breathing in which one breath forcefully and rapidly and thus, exercises inspiratory as well as expiratory muscles [ 7 ].
In breathing exercises like Kapalbhati, short powerful strokes of exhalation in quick succession with contraction of abdominal and diaphragmatic muscles train the subject to make full use of diaphragm and abdominal muscles in breathing. It also helps in removal of secretions from bronchial tree, clearing up respiratory passages and the alveoli making room for more air [ 7 ].
There has been a case report [ 20 ] of occurrence of pneumothorax with practice of Kapalabhati pranayama but there was no such occurence in our study. Yoga strengthens the respiratory musculature due to which chest and lungs inflate and deflate to fullest possible extent and muscles are made to work to maximal extent. Abdominal breathing uses the diaphragm and performs respiration with least effort. While, chest breathing utilizes intercostal muscles [ 18 ]. It is less efficient [ 21 ]. With the regular practice of breath holding the individual’s central and peripheral chemoreceptor’s gets adapted to the anoxia, this result is achieved by the body by causing hypo metabolism. Thus, reflecting as prolonged breath hold and decreased urge to breathe while doing so. In addition to this, the training of the stretch receptors in the respiratory muscles, chest wall and also walls of the alveoli support the breath holding [ 22 ]. Pranayama training causes an increase in the voluntary breath holding time. This may be due to acclimatization of the chemoreceptors to hypercapnoea [ 23 ].
Lung inflation near to TLC is a major stimulus for release of lung surfactant into alveolar spaces which increases the lung compliance [ 3 ]. During pranayama, there is slow & prolonged inspiration and expiration. It stretches elastin & collagen fibres interwoven among lung parenchyma. Hence these fibres elongate to a greater extent [ 24 ]. During pranayama training, regular inspiration and expiration for longer duration would lead to acclimatization of central and peripheral chemoreceptors for both hypercapnoea and hypoxia [ 25 ]. A study by Bhargava MR et al., showed a statistically significant increased breath holding time after the pranayama practice[ 26 ]. Acclimatization of the stretch receptors increase the synchronization between the lung tissue and the cortex. Continous pranayama training causes increased breath holding time [ 26 , 27 ]. Another possible explanation for the role of yoga in improving the functioning of Lungs and in reducing the mast cell degranulation could be based on the frictional stress from air flowing through narrowed airways damaging the airway mucosa and thereby perpetuating airway inflammation and airway obstruction. The slow and gentle breathing in some of the Pranayamas may reverse the process by reducing the frictional stress, and thereby stabilizing the mast cell degranulation [ 28 ].
A growing number of literatures have confirmed that endotoxin is the main mediator in byssinosis and obstructive lung diseases [ 29 ]. The deep inspiration, retention of air and slow expiration increases the overall capacity of the lungs and gradually improves the ventilatory functioning of lungs. Due to the proper working of these organs, vital energy flows to maintain the normal homeostasis of the body and thus it helps in prevention, control and rehabilitation of many respiratory diseases [ 30 ].
Thus this present study indicates that the regular practice of pranayama improves pulmonary function and is beneficial to improve respiratory efficiency.
After 2 months of yoga training, the readings of VC, TV, ERV, BHT, 40mm endurance, PEFR show significant increase. From the present study we may conclude that yoga practice can be advocated to improve pulmonary functions in healthy individuals and hence to prevent respiratory diseases in future. These benificial effect of pranayama can be used as an adjuvant therapy for many respiratory diseases. The daily practice could also be parts of physical fitness and life style modification programs in maintaining better physical and mental health. Hence, it can be said that pranayama improves respiratory breathing capacity by increasing chest wall expansion and forced expiratory lung volumes.
Financial or Other Competing Interests
- [1]. Ruprai Reena Kaur, et al. Effect of yoga training on breathing rate and lung functions in patients of bronchial asthma. International Journal of Recent Trends in Science and Technology. 2013;5(3):127–29. ISSN 2277-2812 E-ISSN 2249-8109. [ Google Scholar ]
- [2]. briggs Tony, A Watts, lessons Breathing, M Addy. A longtime Iyengar Yoga teacher tells you why you should be holding your breath. Yoga journal. 2000;11/12:94. [ Google Scholar ]
- [3]. LN Joshi, VD Joshi, LV Gokhale. Effect of short term Pranayama on Ventilatory functions of lung. Indian J Physiol Pharmacol. 1992;36:105–08. [ PubMed ] [ Google Scholar ]
- [4]. S Bhattacharya, US Pandey, NS Verma. Improvement in oxidative status with yogic breathing in young healthy males. Indian J Physiol Pharmacol. 2002;46:349–54. [ PubMed ] [ Google Scholar ]
- [5]. K Makwana, et al. Effect of short term yoga practice on ventilatory function tests. Indian J Physiol Pharmacol. 1988;32(3):202–08. [ PubMed ] [ Google Scholar ]
- [6]. LN Joshi, VD Joshi, LV Gokhale. Effect of short term Pranayama practice on breathing rate and ventilatory functions of lung. Indian J Physiol Pharmacol. 1992;32:105–08. [ PubMed ] [ Google Scholar ]
- [7]. NK Subbalakshmi, SK Saxena, Urmimala, JA Urban. Immediate effect of nadi -shodhana pranayama on some selected parameters of cardiovascular, pulmo-nary and higher functions of brain. Thai Journal of Physiological Sciences. 2005;18(2):10–16. [ Google Scholar ]
- [8]. http://www.healthandyoga.com/html/pran/nadishudhi.aspx .
- [9]. http://yogafitnessedu.com/yoga-sutras-kapalbhati-pranayama/
- [10]. Yoga sutras: Kapalbhati pranayama, Yoga fitness. 2014 [ Google Scholar ]
- [11]. http://thecompleteyoga.com/pranayama/
- [12]. Saraswati, Lab manual health and physical education . Saraswati House Pvt Ltd. TetracyclineTeratology. 2000:79. [ Google Scholar ]
- [13]. Spiritual energy draws prana to preservation, The Jakarta post. 2012 [ Google Scholar ]
- [14]. Rao Nani. How to practice surya namaskar the right way. The health site. 2013 [ Google Scholar ]
- [15]. http://www.healthandyoga.com/html/news/surya.aspx .
- [16]. P Grover, VD Varma, D Pershad, SK Verma. Role of yoga in the treatment of psychoneuron’s bull. PGI. 1998;22(2):68–76. [ Google Scholar ]
- [17]. Jain Nidhi, RD Srivastava, As Singhal. The effect of the right and left nostril breathing on the cardiorespiratory and the autonomic parameters. Indian J Physiol Pharmacol. 2005;49(4):469–74. [ PubMed ] [ Google Scholar ]
- [18]. R Chanavirut, K Khaidjapho, P Jaree, P Pongnaratorn. Yoga exercise increases chest wall expansion and lung volumes. Thai Journal of Physiological Sciences. 2006;19(1):1–7. [ Google Scholar ]
- [19]. Mohan Madan, et al. Effect of yoga training on reaction time, respiratory endurance and muscle strength. Indian J Physiol Pharmacol. 1992;36(4):229–33. [ PubMed ] [ Google Scholar ]
- [20]. DB Johnson, MJ Tierney, PJ Sadighi. Kapalabhati pranayama: breathe of fire or cause of pneumothorax? A case report. Chest. 2004;125:1951–52. doi: 10.1378/chest.125.5.1951. [ DOI ] [ PubMed ] [ Google Scholar ]
- [21]. RK Yadav, S Das. Effect of yogic practice on pulmonary functions in young females. Indian J Physiol Pharmacol. 2001;45(4):493–96. [ PubMed ] [ Google Scholar ]
- [22]. Amte, et al. Clinical effects of pranayama on performance of rifle shooters. Int J Med Res Health Sci. 2014;3(3):580–86. [ Google Scholar ]
- [23]. V Shankarappa, et al. The short term effect of pranayama on the lung parameters. Journal of Clinical and Diagnostic Research. 2012;6(1):27–30. [ Google Scholar ]
- [24]. BKS Iyengar. London: Geovge Allen and Unwin Ltd; 1968. Light on Yoga; pp. 243–45. [ Google Scholar ]
- [25]. LN Joshi, VD Joshi. Effect of forced breathing on the ventilatory functions of the lung. J Postgrad Med. 1998;44(3):67–69. [ PubMed ] [ Google Scholar ]
- [26]. MR Bhargava, MG Gogate. A study of BHT and its variations following pranayamic exercises. The Clinician. 1982:43–46. [ Google Scholar ]
- [27]. R Jerath, J Edry, V Barnes, V Jerath. Physiology of long pranayamic breathing: Neural respiratory elements may provide a mechanism that can explain how slow deep breathing shifts the autonomic nervous system. Medical hypo. 2008;67(3):566–71. doi: 10.1016/j.mehy.2006.02.042. [ DOI ] [ PubMed ] [ Google Scholar ]
- [28]. Sharma Dr. K Krishna, et al. Effect of yoga therapy on lung functions in respiratory disorder subjects. European Scientific Journal. 2014;10(6) ISSN: 1857 - 7881 (Print) e - ISSN 1857- 7431. [ Google Scholar ]
- [29]. Rajsri, et al. A study on pulmonary function tests in weavers. Int J Med Res Health Sci. 2013;2(4):857–60. [ Google Scholar ]
- [30]. Shravya, et al. Immediate effect of suryanadi pranayama on pulmonary function (ventilatory volumes and capacities) in healthy volunteers. Int J Med Res Helath Sci. 2013;2(4):724–29. [ Google Scholar ]
- View on publisher site
- PDF (81.6 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
Chronic obstructive pulmonary disease (COPD) is a progressive lung condition affecting millions worldwide, primarily linked to smoking. It is marked by a persistent reduction in airflow that gradually worsens, making it increasingly difficult to breathe. Common symptoms of COPD include chronic coughing, wheezing, shortness of breath, and chest ...
See all options. Chronic obstructive pulmonary disease (COPD) is suspected in patients with a history of smoking, occupational and environmental risk factors, or a personal or family history of chronic lung disease. Presents with shortness of breath, wheeze, cough, and sputum production. Diagnostic tests include ...
Dr. Matthew J. Emmett (Medicine): An 81-year-old man was admitted to this hospital with fever, cough, and shortness of breath during the pandemic of coronavirus disease 2019 (Covid-19), the ...
COPD: a case study Authors Debbie Price is lead practice nurse, Llandrindod Wells Medical Practice; Nikki Williams is associate professor of respiratory and sleep physiology, Swansea University. Abstract This article uses a case study to discuss the symptoms, causes and management of chronic obstructive pulmonary disease, describing the patient's
ATS Clinical Cases. The ATS Clinical Cases are a series of cases devoted to interactive clinical case presentations on all aspects of pulmonary, critical care and sleep medicine. They are designed to provide education to practitioners, faculty, fellows, residents, and medical students in the areas of pulmonary, critical care and sleep medicine.
Here is a case study for students and medical practitioners aimed at providing a clinical simulation exam scenario in patients with COPD. A COPD case study. The 56-year-old patient presents with a difficulty in breathing. The patient complained of feeling short of breath in the morning upon waking up.
In the case of COPD, this information is especially relevant given its importance in epidemiology, clinical manifestation and health management. 10 Furthermore, the study of the medical student population represents an especially relevant niche since they have recently studied the disease and are close to receiving a license to practice ...
Today, we're talking about the diagnosis and management of COPD. COPD is the most common chronic lung disease in the world. Global prevalence is about 10%, and its prevalence is only expected to ...
Chronic obstructive pulmonary disease (COPD) is associated with a high clinical and economic burden and is the fourth leading cause of death in the United States. The management of patients with COPD aims to minimize and control symptoms, prevent exacerbations, and improve quality of life. We provide an illustrated case study of a female patient with typical progression of COPD and describe ...
Case study 1: A 63-year-old man with moderate/severe COPD and a chest infection. ... COPD, chronic obstructive pulmonary disease; mMRC, modified Medical Research Council Dyspnoea Scale. ...
Abstract. Introduction: This case was developed to be administered during an internal medicine-geriatrics clerkship with third-year medical students in a small-group setting of approximately 5-20 students to provide instructions on the diagnosis and treatment of chronic obstructive pulmonary disease. It is based on learning objectives from the ...
Alpha 1 Antitrypsin Deficiency with Normal Levels Presenting as a Diagnostic Challenge. Suma Menon, Sindhuja Marupudi, Muhammad Imtiaz Ahmad, Fatima Khan, and Ahmar Malik. Holey Moly! A Case of the Vanishing Lung. Janvi Paralkar, Navitha Ramesh, and Albert Miller.
Meet Susan M! Share your impressions in our latest COPD case study. Summary of in-patient admission: Susan M. is being discharged today following a 6-day ICU and step-down admission for acute exacerbation of COPD with bacterial pneumonia requiring intubation and mechanical ventilation for a period of 32 hours. Subsequent to her extubation and transfer to the step down unit she was treated with ...
The objective of the present study is to determine the current level of understanding of COPD among said population. Methods: A cross-sectional observational study was done using digital surveys given to medical students in their final year at the Universidad de Sevilla. Those surveyed were asked about demographic data, smoking habits as well ...
We're interested in your thoughts on another COPD case study: Jim B., a 68-year-old man here for his Phase II Pulmonary Rehabilitation intake interview. A bit more about Jim: Medical history: COPD, FEV1 six weeks ago was 38% of normal predicted, recent CXR shows flattened diaphragm with increased AP diameter, appendectomy age 34, broken nose and broken right arm as a child.
This Independent Study is brought to you for free and open access by the Department of Nursing at UND Scholarly Commons. It has been accepted for inclusion in Nursing Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact. [email protected]. COPD Case Study.
This page titled 2: Case Study #1- Chronic Obstructive Pulmonary Disease (COPD) is shared under a CC BY-SA 4.0 license and was authored, remixed, and/or curated by Glynda Rees, Rob Kruger, and Janet Morrison via source content that was edited to the style and standards of the LibreTexts platform.
According to recent studies, the prevalence of COPD in older adults is increasing, along with the complexity of care due to comorbidities, drug interactions, and side effects. A thorough evaluation of a patient case provides insight into the everyday challenges of COPD management. [Journal of Gerontological Nursing, 44(7), 10-14.].
This case study provides a critical analysis of the management of a patient with long-term conditions in a community matron service. Particular attention is given to the effect of chronic obstructive pulmonary disease (COPD). The effect of COPD on health and wellbeing, quality of life and hospital admissions is examined, and outcomes are ...
Aim: The present study is planned to find the effect of pranayama on pulmonary functions in medical students. Materials and Methods: This study is conducted on 50 students doing lst year M.B.B.S. Consent form has been taken from them. They have been given yoga training 30 min daily for 2 mnth under the guidance of a trained yoga instructor.