- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Zink is a board-certified emergency medicine physician with expertise in the wilderness and global medicine.
- Screening & Prevention
- Sexual Health & Relationships
- Birth Control
- Preparing for Surgery Checklist
- Healthy Teens
- Getting Pregnant
- During Pregnancy
- Labor and Delivery
- After Pregnancy
- Pregnancy Book
- Mental Health
- Prenatal Testing
- Menstrual Health
- Heart Health
- Special Procedures
- Diseases and Conditions
- Browse All Topics
- View All Frequently Asked Questions

Read common questions on the coronavirus and ACOG’s evidence-based answers.
If Your Baby Is Breech
URL has been copied to the clipboard
Frequently Asked Questions Expand All
In the last weeks of pregnancy, a fetus usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation . A breech presentation occurs when the fetus’s buttocks, feet, or both are in place to come out first during birth. This happens in 3–4% of full-term births.
It is not always known why a fetus is breech. Some factors that may contribute to a fetus being in a breech presentation include the following:
You have been pregnant before.
There is more than one fetus in the uterus (twins or more).
There is too much or too little amniotic fluid .
The uterus is not normal in shape or has abnormal growths such as fibroids .
The placenta covers all or part of the opening of the uterus ( placenta previa )
The fetus is preterm .
Occasionally fetuses with certain birth defects will not turn into the head-down position before birth. However, most fetuses in a breech presentation are otherwise normal.
Your health care professional may be able to tell which way your fetus is facing by placing his or her hands at certain points on your abdomen. By feeling where the fetus's head, back, and buttocks are, it may be possible to find out what part of the fetus is presenting first. An ultrasound exam or pelvic exam may be used to confirm it.
External cephalic version (ECV) is an attempt to turn the fetus so that he or she is head down. ECV can improve your chance of having a vaginal birth. If the fetus is breech and your pregnancy is greater than 36 weeks your health care professional may suggest ECV.
ECV will not be tried if:
You are carrying more than one fetus
There are concerns about the health of the fetus
You have certain abnormalities of the reproductive system
The placenta is in the wrong place
The placenta has come away from the wall of the uterus ( placental abruption )
ECV can be considered if you have had a previous cesarean delivery .
The health care professional performs ECV by placing his or her hands on your abdomen. Firm pressure is applied to the abdomen so that the fetus rolls into a head-down position. Two people may be needed to perform ECV. Ultrasound also may be used to help guide the turning.
The fetus's heart rate is checked with fetal monitoring before and after ECV. If any problems arise with you or the fetus, ECV will be stopped right away. ECV usually is done near a delivery room. If a problem occurs, a cesarean delivery can be performed quickly, if necessary.
Complications may include the following:
Prelabor rupture of membranes
Changes in the fetus's heart rate
Placental abruption
Preterm labor
More than one half of attempts at ECV succeed. However, some fetuses who are successfully turned with ECV move back into a breech presentation. If this happens, ECV may be tried again. ECV tends to be harder to do as the time for birth gets closer. As the fetus grows bigger, there is less room for him or her to move.
Most fetuses that are breech are born by planned cesarean delivery. A planned vaginal birth of a single breech fetus may be considered in some situations. Both vaginal birth and cesarean birth carry certain risks when a fetus is breech. However, the risk of complications is higher with a planned vaginal delivery than with a planned cesarean delivery.
In a breech presentation, the body comes out first, leaving the baby’s head to be delivered last. The baby’s body may not stretch the cervix enough to allow room for the baby’s head to come out easily. There is a risk that the baby’s head or shoulders may become wedged against the bones of the mother’s pelvis. Another problem that can happen during a vaginal breech birth is a prolapsed umbilical cord . It can slip into the vagina before the baby is delivered. If there is pressure put on the cord or it becomes pinched, it can decrease the flow of blood and oxygen through the cord to the baby.
Although a planned cesarean birth is the most common way that breech fetuses are born, there may be reasons to try to avoid a cesarean birth.
A cesarean delivery is major surgery. Complications may include infection, bleeding, or injury to internal organs.
The type of anesthesia used sometimes causes problems.
Having a cesarean delivery also can lead to serious problems in future pregnancies, such as rupture of the uterus and complications with the placenta.
With each cesarean delivery, these risks increase.
If you are thinking about having a vaginal birth and your fetus is breech, your health care professional will review the risks and benefits of vaginal birth and cesarean birth in detail. You usually need to meet certain guidelines specific to your hospital. The experience of your health care professional in delivering breech babies vaginally also is an important factor.
Amniotic Fluid : Fluid in the sac that holds the fetus.
Anesthesia : Relief of pain by loss of sensation.
Breech Presentation : A position in which the feet or buttocks of the fetus would appear first during birth.
Cervix : The lower, narrow end of the uterus at the top of the vagina.
Cesarean Delivery : Delivery of a fetus from the uterus through an incision made in the woman’s abdomen.
External Cephalic Version (ECV) : A technique, performed late in pregnancy, in which the doctor attempts to manually move a breech baby into the head-down position.
Fetus : The stage of human development beyond 8 completed weeks after fertilization.
Fibroids : Growths that form in the muscle of the uterus. Fibroids usually are noncancerous.
Oxygen : An element that we breathe in to sustain life.
Pelvic Exam : A physical examination of a woman’s pelvic organs.
Placenta : Tissue that provides nourishment to and takes waste away from the fetus.
Placenta Previa : A condition in which the placenta covers the opening of the uterus.
Placental Abruption : A condition in which the placenta has begun to separate from the uterus before the fetus is born.
Prelabor Rupture of Membranes : Rupture of the amniotic membranes that happens before labor begins. Also called premature rupture of membranes (PROM).
Preterm : Less than 37 weeks of pregnancy.
Ultrasound Exam : A test in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Umbilical Cord : A cord-like structure containing blood vessels. It connects the fetus to the placenta.
Uterus : A muscular organ in the female pelvis. During pregnancy, this organ holds and nourishes the fetus.
Vagina : A tube-like structure surrounded by muscles. The vagina leads from the uterus to the outside of the body.
Vertex Presentation : A presentation of the fetus where the head is positioned down.
Article continues below
Advertisement
If you have further questions, contact your ob-gyn.
Don't have an ob-gyn? Learn how to find a doctor near you .
Published: January 2019
Last reviewed: August 2022
Copyright 2024 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information . This information is designed as an educational aid for the public. It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer .
Clinicians: Subscribe to Digital Pamphlets
Explore ACOG's library of patient education pamphlets.
A Guide to Pregnancy from Ob-Gyns
For trusted, in-depth advice from ob-gyns, turn to Your Pregnancy and Childbirth: Month to Month.
ACOG Explains
A quick and easy way to learn more about your health.
What to Read Next
Cesarean Birth
Fetal Heart Rate Monitoring During Labor
What is back labor?
What is delayed cord clamping?
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Labor & Delivery
What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles
When viewing this topic in a different language, you may notice some differences in the way the content is structured, but it still reflects the latest evidence-based guidance.
Breech presentation
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Breech presentation in pregnancy occurs when a baby presents with the buttocks or feet rather than the head first (cephalic presentation) and is associated with increased morbidity and mortality for both the mother and the baby. [1] Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997. [2] Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002. There is good current evidence regarding effective management of breech presentation in late pregnancy using external cephalic version and/or planned cesarean section.
History and exam
Key diagnostic factors.
- buttocks or feet as the presenting part
- fetal head under costal margin
- fetal heartbeat above the maternal umbilicus
Other diagnostic factors
- subcostal tenderness
- pelvic or bladder pain
Risk factors
- premature fetus
- small for gestational age fetus
- nulliparity
- fetal congenital anomalies
- previous breech delivery
- uterine abnormalities
- abnormal amniotic fluid volume
- placental abnormalities
- female fetus
Diagnostic tests
1st tests to order.
- transabdominal/transvaginal ultrasound
Treatment algorithm
<37 weeks' gestation and in labor, ≥37 weeks' gestation not in labor, ≥37 weeks' gestation in labor: no imminent delivery, ≥37 weeks' gestation in labor: imminent delivery, contributors, natasha nassar, phd.
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Disclosures
NN has received salary support from Australian National Health and a Medical Research Council Career Development Fellowship; she is an author of a number of references cited in this topic.
Christine L. Roberts, MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
CLR declares that she has no competing interests.
Jonathan Morris, MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
JM declares that he has no competing interests.
Peer reviewers
John w. bachman, md.
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
JWB declares that he has no competing interests.
Rhona Hughes, MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
RH declares that she has no competing interests.
Brian Peat, MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
BP declares that he has no competing interests.
Lelia Duley, MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
LD declares that she has no competing interests.
Justus Hofmeyr, MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
JH is an author of a number of references cited in this topic.
Differentials
- Transverse lie
- Caesarean birth
- Mode of term singleton breech delivery
Use of this content is subject to our disclaimer
Log in or subscribe to access all of BMJ Best Practice
Log in to access all of bmj best practice, help us improve bmj best practice.
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Pregnancy Symptoms 5
- Can I get pregnant if… ? 3
- Paternity Tests 2
- The Bumpy Truth Blog 7
- Multiple Births 10
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Cord Blood 4
- Pregnancy Supplements & Medications 14
- Pregnancy Products & Tests 8
- Changes In Your Body 5
- Health & Nutrition 2
- Labor and Birth 65
- Planning and Preparing 24
- Breastfeeding 29
- Week by Week Newsletter 40
- Is it Safe While Pregnant 55
- The First Year 41
- Genetic Disorders & Birth Defects 17
- Pregnancy Health and Wellness 149
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Uncategorized 4
- Women's Health 34
- Prenatal Testing 16
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
- Pregnancy Questions Center
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Breech Presentation
- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE , Medicine , Surgery , Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Table of Contents
Suggest an improvement
- Hidden Post Title
- Hidden Post URL
- Hidden Post ID
- Type of issue * N/A Fix spelling/grammar issue Add or fix a link Add or fix an image Add more detail Improve the quality of the writing Fix a factual error
- Please provide as much detail as possible * You don't need to tell us which article this feedback relates to, as we automatically capture that information for you.
- Your Email (optional) This allows us to get in touch for more details if required.
- Which organ is responsible for pumping blood around the body? * Enter a five letter word in lowercase
- Name This field is for validation purposes and should be left unchanged.
Introduction
Breech presentation is a type of malpresentation and occurs when the fetal head lies over the uterine fundus and fetal buttocks or feet present over the maternal pelvis (instead of cephalic/head presentation).
The incidence in the United Kingdom of breech presentation is 3-4% of all fetuses. 1
Breech presentation is most commonly idiopathic .
Types of breech presentation
The three types of breech presentation are:
- Complete (flexed) breech : one or both knees are flexed (Figure 1)
- Footling (incomplete) breech : one or both feet present below the fetal buttocks, with hips and knees extended (Figure 2)
- Frank (extended) breech : both hips flexed and both knees extended. Babies born in frank breech are more likely to have developmental dysplasia of the hip (Figure 3)

Risk factors
Risk factors for breech presentation can be divided into maternal , fetal and placental risk factors:
- Maternal : multiparity, fibroids, previous breech presentation, Mullerian duct abnormalities
- Fetal : preterm, macrosomia, fetal abnormalities (anencephaly, hydrocephalus, cystic hygroma), multiple pregnancy
- Placental : placenta praevia , polyhydramnios, oligohydramnios , amniotic bands
Clinical features
Before 36 weeks , breech presentation is not significant, as the fetus is likely to revert to a cephalic presentation. The mother will often be asymptomatic with the diagnosis being incidental.
The incidence of breech presentation is approximately 20% at 28 weeks gestation, 16% at 32 weeks gestation and 3-4% at term . Therefore, breech presentation is more common in preterm labour . Most fetuses with breech presentation in the early third trimester will turn spontaneously and be cephalic at term.
However, spontaneous version rates for nulliparous women with breech presentation at 36 weeks of gestation are less than 10% .
Clinical examination
Typical clinical findings of a breech presentation include:
- Longitudinal lie
- Head palpated at the fundus
- Irregular mass over pelvis (feet, legs and buttocks)
- Fetal heart auscultated higher on the maternal abdomen
- Palpation of feet or sacrum at the cervical os during vaginal examination
For more information, see the Geeky Medics guide to obstetric abdominal examination .
Positions in breech presentation
There are multiple fetal positions in breech presentation which are described according to the relation of the fetal sacrum to the maternal pelvis .
These are: direct sacroanterior, left sacroanterior, right sacroanterior, direct sacroposterior, right sacroposterior, left sacroposterior, left sacrotransverse and right sacrotranverse. 5
Investigations
An ultrasound scan is diagnostic for breech presentation. Growth, amniotic fluid volume and anatomy should be assessed to check for abnormalities.
There are three management options for breech presentation at term, with consideration of maternal choice: external cephalic version , vaginal delivery and Caesarean section .
External cephalic version
External cephalic version (ECV) involves manual rotation of the fetus into a cephalic presentation by applying pressure to the maternal abdomen under ultrasound guidance. Entonox and subcutaneous terbutaline are used to relax the uterus.
ECV has a 40% success rate in primiparous women and 60% in multiparous women . It should be offered to nulliparous women at 36 weeks and multiparous women at 37 weeks gestation.
If ECV is unsuccessful, then delivery options include elective caesarean section or vaginal delivery.
Contraindications for undertaking external cephalic version include:
- Antepartum haemorrhage
- Ruptured membranes
- Previous caesarean section
- Major uterine abnormality
- Multiple pregnancy
- Abnormal cardiotocography (CTG)
Vaginal delivery
Vaginal delivery is an option but carries risks including head entrapment, birth asphyxia, intracranial haemorrhage, perinatal mortality, cord prolapse and fetal and/or maternal trauma.
The preference is to deliver the baby without traction and with an anterior sacrum during delivery to decrease the risk of fetal head entrapment .
The mother may be offered an epidural , as vaginal breech delivery can be very painful. 6
Contraindications for vaginal delivery in a breech presentation include:
- Footling breech: the baby’s head and trunk are more likely to be trapped if the feet pass through the dilated cervix too soon
- Macrosomia: usually defined as larger than 3800g
- Growth restricted baby: usually defined as smaller than 2000g
- Other complications of vaginal birth: for example, placenta praevia and fetal compromise
- Lack of clinical staff trained in vaginal breech delivery
Caesarean section
A caesarian section booked as an elective procedure at term is the most common management for breech presentation.
Caesarean section is preferred for preterm babies (due to an increased head to abdominal circumference ratio in preterm babies) and is used if the external cephalic version is unsuccessful or as a maternal preference. This option has fewer risks than a vaginal delivery.
Complications
Fetal complications of breech presentation include:
- Developmental dysplasia of the hip (DDH)
- Cord prolapse
- Fetal head entrapment
- Birth asphyxia
- Intracranial haemorrhage
- Perinatal mortality
Complications of external cephalic version include:
- Transient fetal heart abnormalities (common)
- Fetomaternal haemorrhage
- Placental abruption (rare)
- There are three types of breech presentation: complete, incomplete and frank breech
- The most common clinical findings include: longitudinal lie, smooth fetal head-shape at the fundus, irregular masses over the pelvis and abnormal placement being required for fetal hear auscultation
- The diagnostic investigation is an ultrasound scan
- Breech presentation can be managed in three ways: external cephalic version , vaginal delivery or elective caesarean section
- Complications are more common in vaginal delivery , such as cord prolapse, fetal head entrapment, intracranial haemorrhage and birth asphyxia
Miss Saba Al Juboori
Consultant in Obstetrics and Gynaecology
Miss Neeraja Kuruba
Dr chris jefferies.
- Oxford Handbook of Obstetrics and Gynaecology. Breech Presentation: Overview. Published in 2011.
- Jemimah Thomas. Image: Complete breech.
- Bonnie Urquhart Gruenberg. Footling breech. Licence: [ CC BY-SA ]
- Bonnie Urquhart Gruenberg. Frank breech . Licence: [ CC BY-SA ]
- A Comprehensive Textbook of Obstetrics and Gynaecology. Chapter 50: Malpresentation and Malposition: Breech Presentation. Published in 2011.
- Diana Hamilton Fairley. Lecture Notes: Obstetrics and Gynaecology, Malpresentation, Breech Presentation. Published in 2009.

Other pages
- Product Bundles 🎉
- Join the Team 🙌
- Institutional Licence 📚
- OSCE Station Creator Tool 🩺
- Create and Share Flashcards 🗂️
- OSCE Group Chat 💬
- Newsletter 📰
- Advertise With Us
Join the community

Breech Presentation
- Author: Richard Fischer, MD; Chief Editor: Ronald M Ramus, MD more...
- Sections Breech Presentation
- Vaginal Breech Delivery
- Cesarean Delivery
- Comparative Studies
- External Cephalic Version
- Conclusions
- Media Gallery
Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of births at term. [ 1 ]
Predisposing factors for breech presentation include prematurity , uterine malformations or fibroids, polyhydramnios , placenta previa , fetal abnormalities (eg, CNS malformations, neck masses, aneuploidy), and multiple gestations . Fetal abnormalities are observed in 17% of preterm breech deliveries and in 9% of term breech deliveries.
Perinatal mortality is increased 2- to 4-fold with breech presentation, regardless of the mode of delivery. Deaths are most often associated with malformations, prematurity, and intrauterine fetal demise .

Types of breeches
The types of breeches are as follows:
Frank breech (50-70%) - Hips flexed, knees extended (pike position)
Complete breech (5-10%) - Hips flexed, knees flexed (cannonball position)
Footling or incomplete (10-30%) - One or both hips extended, foot presenting
Historical considerations
Vaginal breech deliveries were previously the norm until 1959 when it was proposed that all breech presentations should be delivered abdominally to reduce perinatal morbidity and mortality. [ 2 ]
Vaginal breech delivery
Three types of vaginal breech deliveries are described, as follows:
Spontaneous breech delivery: No traction or manipulation of the infant is used. This occurs predominantly in very preterm, often previable, deliveries.
Assisted breech delivery: This is the most common type of vaginal breech delivery. The infant is allowed to spontaneously deliver up to the umbilicus, and then maneuvers are initiated to assist in the delivery of the remainder of the body, arms, and head.
Total breech extraction: The fetal feet are grasped, and the entire fetus is extracted. Total breech extraction should be used only for a noncephalic second twin; it should not be used for a singleton fetus because the cervix may not be adequately dilated to allow passage of the fetal head. Total breech extraction for the singleton breech is associated with a birth injury rate of 25% and a mortality rate of approximately 10%. Total breech extractions are sometimes performed by less experienced accoucheurs when a foot unexpectedly prolapses through the vagina. As long as the fetal heart rate is stable in this situation, it is permissible to manage expectantly to allow the cervix to completely dilate around the breech (see the image below).

Technique and tips for assisted vaginal breech delivery
The fetal membranes should be left intact as long as possible to act as a dilating wedge and to prevent overt cord prolapse .
Oxytocin induction and augmentation are controversial. In many previous studies, oxytocin was used for induction and augmentation, especially for hypotonic uterine dysfunction. However, others are concerned that nonphysiologic forceful contractions could result in an incompletely dilated cervix and an entrapped head.
An anesthesiologist and a pediatrician should be immediately available for all vaginal breech deliveries. A pediatrician is needed because of the higher prevalence of neonatal depression and the increased risk for unrecognized fetal anomalies. An anesthesiologist may be needed if intrapartum complications develop and the patient requires general anesthesia .
Some clinicians perform an episiotomy when the breech delivery is imminent, even in multiparas, as it may help prevent soft tissue dystocia for the aftercoming head (see the images below).

The Pinard maneuver may be needed with a frank breech to facilitate delivery of the legs but only after the fetal umbilicus has been reached. Pressure is exerted in the popliteal space of the knee. Flexion of the knee follows, and the lower leg is swept medially and out of the vagina.
No traction should be exerted on the infant until the fetal umbilicus is past the perineum, after which time maternal expulsive efforts should be used along with gentle downward and outward traction of the infant until the scapula and axilla are visible (see the image below).

Use a dry towel to wrap around the hips (not the abdomen) to help with gentle traction of the infant (see the image below).

An assistant should exert transfundal pressure from above to keep the fetal head flexed.
Once the scapula is visible, rotate the infant 90° and gently sweep the anterior arm out of the vagina by pressing on the inner aspect of the arm or elbow (see the image below).

Rotate the infant 180° in the reverse direction, and sweep the other arm out of the vagina. Once the arms are delivered, rotate the infant back 90° so that the back is anterior (see the image below).

The fetal head should be maintained in a flexed position during delivery to allow passage of the smallest diameter of the head. The flexed position can be accomplished by using the Mauriceau Smellie Veit maneuver, in which the operator's index and middle fingers lift up on the fetal maxillary prominences, while the assistant applies suprapubic pressure (see the image below).

Alternatively, Piper forceps can be used to maintain the head in a flexed position (see the image below).

In many early studies, routine use of Piper forceps was recommended to protect the head and to minimize traction on the fetal neck. Piper forceps are specialized forceps that are placed from below the infant and, unlike conventional forceps, are not tailored to the position of the fetal head (ie, it is a pelvic, not cephalic, application). The forceps are applied while the assistant supports the fetal body in a horizontal plane.
During delivery of the head, avoid extreme elevation of the body, which may result in hyperextension of the cervical spine and potential neurologic injury (see the images below).

Lower Apgar scores, especially at 1 minute, are more common with vaginal breech deliveries. Many advocate obtaining an umbilical cord artery and venous pH for all vaginal breech deliveries to document that neonatal depression is not due to perinatal acidosis.
Fetal head entrapment may result from an incompletely dilated cervix and a head that lacks time to mold to the maternal pelvis. This occurs in 0-8.5% of vaginal breech deliveries. [ 3 ] This percentage is higher with preterm fetuses (< 32 wk), when the head is larger than the body. Dührssen incisions (ie, 1-3 cervical incisions made to facilitate delivery of the head) may be necessary to relieve cervical entrapment. However, extension of the incision can occur into the lower segment of the uterus, and the operator must be equipped to deal with this complication. The Zavanelli maneuver has been described, which involves replacement of the fetus into the abdominal cavity followed by cesarean delivery. While success has been reported with this maneuver, fetal injury and even fetal death have occurred.
Nuchal arms, in which one or both arms are wrapped around the back of the neck, are present in 0-5% of vaginal breech deliveries and in 9% of breech extractions. [ 3 ] Nuchal arms may result in neonatal trauma (including brachial plexus injuries) in 25% of cases. Risks may be reduced by avoiding rapid extraction of the infant during delivery of the body. To relieve nuchal arms when it is encountered, rotate the infant so that the fetal face turns toward the maternal symphysis pubis (in the direction of the impacted arm); this reduces the tension holding the arm around the back of the fetal head, allowing for delivery of the arm.
Cervical spine injury is predominantly observed when the fetus has a hyperextended head prior to delivery. Ballas and Toaff (1976) reported 20 cases of hyperextended necks, defined as an angle of extension greater than 90° ("star-gazing"), discovered on antepartum radiographs. [ 4 ] Of the 11 fetuses delivered vaginally, 8 (73%) sustained complete cervical spinal cord lesions, defined as either transection or nonfunction.
Cord prolapse may occur in 7.4% of all breech labors. This incidence varies with the type of breech: 0-2% with frank breech, 5-10% with complete breech, and 10-25% with footling breech. [ 3 ] Cord prolapse occurs twice as often in multiparas (6%) than in primigravidas (3%). Cord prolapse may not always result in severe fetal heart rate decelerations because of the lack of presenting parts to compress the umbilical cord (ie, that which predisposes also protects).
Prior to the 2001 recommendations by the American College of Obstetricians and Gynecologists (ACOG), approximately 50% of breech presentations were considered candidates for vaginal delivery. Of these candidates, 60-82% were successfully delivered vaginally.
Candidates can be classified based on gestational age. For pregnancies prior to 26 weeks' gestation, prematurity, not mode of delivery, is the greatest risk factor. Unfortunately, no randomized clinical trials to help guide clinical management have been reported. Vaginal delivery can be considered, but a detailed discussion of the risks from prematurity and the lack of data regarding the ideal mode of delivery should take place with the parent(s). For example, intraventricular hemorrhage, which can occur in an infant of extremely low birth weight, should not be misinterpreted as proof of a traumatic vaginal breech delivery.
For pregnancies between 26 and 32 weeks, retrospective studies suggest an improved outcome with cesarean delivery, although these reports are subject to selection bias. In contrast, between 32 and 36 weeks' gestation, vaginal breech delivery may be considered after a discussion of risks and benefits with the parent(s).
After 37 weeks' gestation, parents should be informed of the results of a multicenter randomized clinical trial that demonstrated significantly increased perinatal mortality and short-term neonatal morbidity associated with vaginal breech delivery (see Comparative Studies). For those attempting vaginal delivery, if estimated fetal weight (EFW) is more than 4000 g, some recommend cesarean delivery because of concern for entrapment of the unmolded head in the maternal pelvis, although data to support this practice are limited.
A frank breech presentation is preferred when vaginal delivery is attempted. Complete breeches and footling breeches are still candidates, as long as the presenting part is well applied to the cervix and both obstetrical and anesthesia services are readily available in the event of a cord prolapse.
The fetus should show no neck hyperextension on antepartum ultrasound imaging (see the image below). Flexed or military position is acceptable.
Regarding prior cesarean delivery, a retrospective study by Ophir et al of 71 women with one prior low transverse cesarean delivery who subsequently delivered a breech fetus found that 24 women had an elective repeat cesarean and 47 women had a trial of labor. [ 5 ] In the 47 women with a trial of labor, 37 (78.7%) resulted in a vaginal delivery. Two infants in the trial of labor group had nuchal arms (1 with a transient brachial plexus injury) and 1 woman required a hysterectomy for hemorrhage due to a uterine dehiscence discovered after vaginal delivery. Vaginal breech delivery after one prior cesarean delivery is not contraindicated, though larger studies are needed.
Primigravida versus multiparous
It had been commonly believed that primigravidas with a breech presentation should have a cesarean delivery, although no data (prospective or retrospective) support this view. The only documented risk related to parity is cord prolapse, which is 2-fold higher in parous women than in primigravid women.
Radiographic and CT pelvimetry
Historically, radiograph pelvimetry was believed to be useful to quantitatively assess the inlet and mid pelvis. Recommended pelvimetry criteria included a transverse inlet diameter larger than 11.5 cm, anteroposterior inlet diameter larger than 10.5 cm, transverse midpelvic diameter (between the ischial spines) larger than 10 cm, and anteroposterior midpelvic diameter larger than 11.5 cm. However, radiographic pelvimetry is rarely, if ever, used in the United States.
CT pelvimetry , which is associated with less fetal radiation exposure than conventional radiographic pelvimetry, was more recently advocated by some investigators. It, too, is rarely used today.
Ultimately, if the obstetrical operator is not experienced or comfortable with vaginal breech deliveries, cesarean delivery may be the best choice. Unfortunately, with the dwindling number of experienced obstetricians who still perform vaginal breech deliveries and who can teach future generations of obstetricians, this technique may soon be lost due to attrition.
In 1970, approximately 14% of breeches were delivered by cesarean delivery. By 1986, that rate had increased to 86%. In 2003, based on data from the National Center for Health Statistics, the rate of cesarean delivery for all breech presentations was 87.2%. Most of the remaining breeches delivered vaginally were likely second twins, fetal demises, and precipitous deliveries. However, the rise in cesarean deliveries for breeches has not necessarily equated with an improvement in perinatal outcome. Green et al compared the outcome for term breeches prior to 1975 (595 infants, 22% cesarean delivery rate for breeches) with those from 1978-1979 (164 infants, 94% cesarean delivery rate for breeches). [ 6 ] Despite the increase in rates of cesarean delivery, the differences in rates of asphyxia, birth injury, and perinatal deaths were not significant.
Maneuvers for cesarean delivery are similar to those for vaginal breech delivery, including the Pinard maneuver, wrapping the hips with a towel for traction, head flexion during traction, rotation and sweeping out of the fetal arms, and the Mauriceau Smellie Veit maneuver.
An entrapped head can still occur during cesarean delivery as the uterus contracts after delivery of the body, even with a lower uterine segment that misleadingly appears adequate prior to uterine incision. Entrapped heads occur more commonly with preterm breeches, especially with a low transverse uterine incision. As a result, some practitioners opt to perform low vertical uterine incisions for preterm breeches prior to 32 weeks' gestation to avoid head entrapment and the kind of difficult delivery that cesarean delivery was meant to avoid. Low vertical incisions usually require extension into the corpus, resulting in cesarean delivery for all future deliveries.
If a low transverse incision is performed, the physician should move quickly once the breech is extracted in order to deliver the head before the uterus begins to contract. If any difficulty is encountered with delivery of the fetal head, the transverse incision can be extended vertically upward (T incision). Alternatively, the transverse incision can be extended laterally and upward, taking great care to avoid trauma to the uterine arteries. A third option is the use of a short-acting uterine relaxant (eg, nitroglycerin) in an attempt to facilitate delivery.
Only 3 randomized studies have evaluated the mode of delivery of the term breech. All other studies were nonrandomized or retrospective, which may be subject to selection bias.
In 1980, Collea et al randomized 208 women in labor with term frank breech presentations to either elective cesarean delivery or attempted vaginal delivery after radiographic pelvimetry. [ 7 ] Oxytocin was allowed for dysfunctional labor. Of the 60 women with adequate pelves, 49 delivered vaginally. Two neonates had transient brachial plexus injuries. Women randomized to elective cesarean delivery had higher postpartum morbidity rates (49.3% vs 6.7%).
In 1983, Gimovsky et al randomized 105 women in labor with term nonfrank breech presentations to a trial of labor versus elective cesarean delivery. [ 8 ] In this group of women, 47 had complete breech presentations, 16 had incomplete breech presentations (hips flexed, 1 knee extended/1 knee flexed), 32 had double-footling presentations, and 10 had single-footling presentations. Oxytocin was allowed for dysfunctional labor. Of the labor group, 44% had successful vaginal delivery. Most cesarean deliveries were performed for inadequate pelvic dimensions on radiographic pelvimetry. The rate of neonatal morbidity did not differ between neonates delivered vaginally and those delivered by cesarean delivery, although a higher maternal morbidity rate was noted in the cesarean delivery group.
In 2000, Hannah and colleagues completed a large, multicenter, randomized clinical trial involving 2088 term singleton fetuses in frank or complete breech presentations at 121 institutions in 26 countries. [ 9 ] In this study, popularly known as the Term Breech Trial, subjects were randomized into a planned cesarean delivery group or a planned vaginal birth group. Exclusion criteria were estimated fetal weight (EFW) more than 4000 g, hyperextension of the fetal head, lethal fetal anomaly or anomaly that might result in difficulty with delivery, or contraindication to labor or vaginal delivery (eg, placenta previa ).
Subjects randomized to cesarean delivery were scheduled to deliver after 38 weeks' gestation unless conversion to cephalic presentation had occurred. Subjects randomized to vaginal delivery were treated expectantly until labor ensued. Electronic fetal monitoring was either continuous or intermittent. Inductions were allowed for standard obstetrical indications, such as postterm gestations. Augmentation with oxytocin was allowed in the absence of apparent fetopelvic disproportion, and epidural analgesia was permitted.
Adequate labor was defined as a cervical dilation rate of 0.5 cm/h in the active phase of labor and the descent of the breech fetus to the pelvic floor within 2 hours of achieving full dilation. Vaginal delivery was spontaneous or assisted and was attended by an experienced obstetrician. Cesarean deliveries were performed for inadequate progress of labor, nonreassuring fetal heart rate, or conversion to footling breech. Results were analyzed by intent-to-treat (ie, subjects were analyzed by randomization group, not by ultimate mode of delivery).
Of 1041 subjects in the planned cesarean delivery group, 941 (90.4%) had cesarean deliveries. Of 1042 subjects in the planned vaginal delivery group, 591 (56.7%) had vaginal deliveries. Indications for cesarean delivery included: fetopelvic disproportion or failure to progress in labor (226), nonreassuring fetal heart rate tracing (129), footling breech (69), request for cesarean delivery (61), obstetrical or medical indications (45), or cord prolapse (12).
The composite measurement of either perinatal mortality or serious neonatal morbidity by 6 weeks of life was significantly lower in the planned cesarean group than in the planned vaginal group (5% vs 1.6%, P < .0001). Six of 16 neonatal deaths were associated with difficult vaginal deliveries, and 4 deaths were associated with fetal heart rate abnormalities. The reduction in risk in the cesarean group was even greater in participating countries with overall low perinatal mortality rates as reported by the World Health Organization. The difference in perinatal outcome held after controlling for the experience level of the obstetrician. No significant difference was noted in maternal mortality or serious maternal morbidity between the 2 groups within the first 6 weeks of delivery (3.9% vs 3.2%, P = .35).
A separate analysis showed no difference in breastfeeding, sexual relations, or depression at 3 months postpartum, though the reported rate of urinary incontinence was higher in the planned vaginal group (7.3% vs 4.5%).
Based on the multicenter trial, the ACOG published a Committee Opinion in 2001 that stated "planned vaginal delivery of a singleton term breech may no longer be appropriate." This did not apply to those gravidas presenting in advanced labor with a term breech and imminent delivery or to a nonvertex second twin.
A follow-up study by Whyte et al was conducted in 2004 on 923 children who were part of the initial multicenter study. [ 10 ] The authors found no differences between the planned cesarean delivery and planned vaginal breech delivery groups with regards to infant death rates or neurodevelopmental delay by age 2 years. Similarly, among 917 participating mothers from the original trial, no substantive differences were apparent in maternal outcome between the 2 groups. [ 11 ] No longer-term maternal effects, such as the impact of a uterine scar on future pregnancies, have yet been reported.
A meta-analysis of the 3 above mentioned randomized trials was published in 2015. The findings included a reduction in perinatal/neonatal death, reduced composite short-term outcome of perinatal/neonatal death or serious neonatal morbidity with planned cesarean delivery versus planned vaginal delivery. [ 12 ] However, at 2 years of age, there was no significant difference in death or neurodevelopmental delay between the two groups. Maternal outcomes assessed at 2 years after delivery were not significantly different.
With regard to preterm breech deliveries, only one prospective randomized study has been performed, which included only 38 subjects (28-36 wk) with preterm labor and breech presentation. [ 13 ] Of these subjects, 20 were randomized to attempted vaginal delivery and 18 were randomized to immediate cesarean delivery. Of the attempted vaginal delivery group, 25% underwent cesarean delivery for nonreassuring fetal heart rate tracings. Five neonatal deaths occurred in the vaginal delivery group, and 1 neonatal death occurred in the cesarean delivery group. Two neonates died from fetal anomalies, 3 from respiratory distress, and 1 from sepsis.
Nonanomalous infants who died were not acidotic at delivery and did not have birth trauma. Differences in Apgar scores were not significant, although the vaginal delivery group had lower scores. The small number of enrolled subjects precluded any definitive conclusions regarding the safety of vaginal breech delivery for a preterm breech.
Retrospective analyses showed a higher mortality rate in vaginal breech neonates weighing 750-1500 g (26-32 wk), but less certain benefit was shown with cesarean delivery if the fetal weight was more than 1500 g (approximately 32 wk). Therefore, this subgroup of very preterm infants (26-32 wk) may benefit from cesarean delivery, although this recommendation is based on potentially biased retrospective data.
A large cohort study was published in 2015 from the Netherlands Perinatal Registry, which included 8356 women with a preterm (26-36 6/7 weeks) breech from 2000 to 2011, over three quarters of whom intended to deliver vaginally. In this overall cohort, there was no significant difference in perinatal mortality between the planned vaginal delivery and planned cesarean delivery groups (adjusted odds ratio 0.97, 95% confidence interval 0.60 – 1.57). However, the subgroup delivering at 28 to 32 weeks had a lower perinatal mortality with planned cesarean section (aOR 0.27, 95% CI 0.10 – 0.77). After adding a composite of perinatal morbidity, planned cesarean delivery was associated with a better outcome than a planned vaginal delivery (aOR 0.77, 95% CI 0.63 – 0.93. [ 14 ]
A Danish study found that nulliparous women with a singleton breech presentation who had a planned vaginal delivery were at significantly higher risk for postoperative complications, such as infection, compared with women who had a planned cesarean delivery. This increased risk was due to the likelihood of conversion to an emergency cesarean section, which occurred in over 69% of the planned vaginal deliveries in the study. [ 15 ]
The Maternal-Fetal Medicine Units Network of the US National Institute of Child Health and Human Development considered a multicenter randomized clinical trial of attempted vaginal delivery versus elective cesarean delivery for 24- to 28-week breech fetuses. [ 16 ] However, it was not initiated because of anticipated difficulty with recruitment, inadequate numbers to show statistically significant differences, and medicolegal concerns. Therefore, this study is not likely to be performed.
External cephalic version (ECV) is the transabdominal manual rotation of the fetus into a cephalic presentation.
Initially popular in the 1960s and 1970s, ECV virtually disappeared after reports of fetal deaths following the procedure. Reintroduced to the United States in the 1980s, it became increasingly popular in the 1990s.
Improved outcome may be related to the use of nonstress tests both before and after ECV, improved selection of low-risk fetuses, and Rh immune globulin to prevent isoimmunization.
Prepare for the possibility of cesarean delivery. Obtain a type and screen as well as an anesthesia consult. The patient should have nothing by mouth for at least 8 hours prior to the procedure. Recent ultrasonography should have been performed for fetal position, to check growth and amniotic fluid volume, to rule out a placenta previa, and to rule out anomalies associated with breech. Another sonogram should be performed on the day of the procedure to confirm that the fetus is still breech.
A nonstress test (biophysical profile as backup) should be performed prior to ECV to confirm fetal well-being.
Perform ECV in or near a delivery suite in the unlikely event of fetal compromise during or following the procedure, which may require emergent delivery.
ECV can be performed with 1 or 2 operators. Some prefer to have an assistant to help turn the fetus, elevate the breech out of the pelvis, or to monitor the position of the baby with ultrasonography. Others prefer a single operator approach, as there may be better coordination between the forces that are raising the breech and moving the head.
ECV is accomplished by judicious manipulation of the fetal head toward the pelvis while the breech is brought up toward the fundus. Attempt a forward roll first and then a backward roll if the initial attempts are unsuccessful. No consensus has been reached regarding how many ECV attempts are appropriate at one time. Excessive force should not be used at any time, as this may increase the risk of fetal trauma.
Following an ECV attempt, whether successful or not, repeat the nonstress test (biophysical profile if needed) prior to discharge. Also, administer Rh immune globulin to women who are Rh negative. Some physicians traditionally induce labor following successful ECV. However, as virtually all of these recently converted fetuses are unengaged, many practitioners will discharge the patient and wait for spontaneous labor to ensue, thereby avoiding the risk of a failed induction of labor. Additionally, as most ECV’s are attempted prior to 39 weeks, as long as there are no obstetrical or medical indications for induction, discharging the patient to await spontaneous labor would seem most prudent.
In those with an unsuccessful ECV, the practitioner has the option of sending the patient home or proceeding with a cesarean delivery. Expectant management allows for the possibility of spontaneous version. Alternatively, cesarean delivery may be performed at the time of the failed ECV, especially if regional anesthesia is used and the patient is already in the delivery room (see Regional anesthesia). This would minimize the risk of a second regional analgesia.
In those with an unsuccessful ECV, the practitioner may send the patient home, if less than 39 weeks, with plans for either a vaginal breech delivery or scheduled cesarean after 39 weeks. Expectant management allows for the possibility of a spontaneous version. Alternatively, if ECV is attempted after 39 weeks, cesarean delivery may be performed at the time of the failed ECV, especially if regional anesthesia is used and the patient is already in the delivery room (see Regional anesthesia). This would minimize the risk of a second regional analgesia.
Success rate
Success rates vary widely but range from 35% to 86% (average success rate in the 2004 National Vital Statistics was 58%). Improved success rates occur with multiparity, earlier gestational age, frank (versus complete or footling) breech presentation, transverse lie, and in African American patients.
Opinions differ regarding the influence of maternal weight, placental position, and amniotic fluid volume. Some practitioners find that thinner patients, posterior placentas, and adequate fluid volumes facilitate successful ECV. However, both patients and physicians need to be prepared for an unsuccessful ECV; version failure is not necessarily a reflection of the skill of the practitioner.
Zhang et al reviewed 25 studies of ECV in the United States, Europe, Africa, and Israel. [ 17 ] The average success rate in the United States was 65%. Of successful ECVs, 2.5% reverted back to breech presentation (other estimates range from 3% to 5%), while 2% of unsuccessful ECVs had spontaneous version to cephalic presentation prior to labor (other estimates range from 12% to 26%). Spontaneous version rates depend on the gestational age when the breech is discovered, with earlier breeches more likely to undergo spontaneous version.
A prospective study conducted in Germany by Zielbauer et al demonstrated an overall success rate of 22.4% for ECV among 353 patients with a singleton fetus in breech presentation. ECV was performed at 38 weeks of gestation. Factors found to increase the likelihood of success were a later week of gestation, abundant amniotic fluid, fundal and anterior placental location, and an oblique lie. [ 18 ]
A systematic review in 2015 looked at the effectiveness of ECV with eight randomized trials of ECV at term. Compared to women with no attempt at ECV, ECV reduced non-cephalic presentation at birth by 60% and reduced cesarean sections by 40% in the same group. [ 19 ] Although the rate of cesarean section is lower when ECV is performed than if not, the overall rate of cesarean section remains nearly twice as high after successful ECV due to both dystocia and non-reassuring fetal heart rate patterns. [ 20 ] Nulliparity was the only factor shown in follow-up to increase the risk of instrumental delivery following successful ECV. [ 21 ]
While most studies of ECV have been performed in university hospitals, Cook showed that ECV has also been effective in the private practice setting. [ 22 ] Of 65 patients with term breeches, 60 were offered ECV. ECV was successful in 32 (53%) of the 60 patients, with vaginal delivery in 23 (72%) of the 32 patients. Of the remaining breech fetuses believed to be candidates for vaginal delivery, 8 (80%) had successful vaginal delivery. The overall vaginal delivery rate was 48% (31 of 65 patients), with no significant morbidity.
Cost analysis
In 1995, Gifford et al performed a cost analysis of 4 options for breech presentations at term: (1) ECV attempt on all breeches, with attempted vaginal breech delivery for selected persistent breeches; (2) ECV on all breeches, with cesarean delivery for persistent breeches; (3) trial of labor for selected breeches, with scheduled cesarean delivery for all others; and (4) scheduled cesarean delivery for all breeches prior to labor. [ 23 ]
ECV attempt on all breeches with attempted vaginal breech delivery on selected persistent breeches was associated with the lowest cesarean delivery rate and was the most cost-effective approach. The second most cost-effective approach was ECV attempt on all breeches, with cesarean delivery for persistent breeches.
Uncommon risks of ECV include fractured fetal bones, precipitation of labor or premature rupture of membranes , abruptio placentae , fetomaternal hemorrhage (0-5%), and cord entanglement (< 1.5%). A more common risk of ECV is transient slowing of the fetal heart rate (in as many as 40% of cases). This risk is believed to be a vagal response to head compression with ECV. It usually resolves within a few minutes after cessation of the ECV attempt and is not usually associated with adverse sequelae for the fetus.
Trials have not been large enough to determine whether the overall risk of perinatal mortality is increased with ECV. The Cochrane review from 2015 reported perinatal death in 2 of 644 in ECV and 6 of 661 in the group that did not attempt ECV. [ 19 ]
A 2016 Practice Bulletin by ACOG recommended that all women who are near term with breech presentations should be offered an ECV attempt if there are no contraindications (see Contraindications below). [ 24 ] ACOG guidelines issued in 2020 recommend that ECV should be performed starting at 37+0 weeks, in order to reduce the likelihood of reversion and to increase the rate of spontaneous version. [ 25 ]
ACOG recommends that ECV be offered as an alternative to a planned cesarean section for a patient who has a term singleton breech fetus, wishes to have a planned vaginal delivery of a vertex-presenting fetus, and has no contraindications. ACOG also advises that ECV be attempted only in settings where cesarean delivery services are available. [ 26 ]
ECV is usually not performed on preterm breeches because they are more likely to undergo spontaneous version to cephalic presentation and are more likely to revert to breech after successful ECV (approximately 50%). Earlier studies of preterm ECV did not show a difference in the rates of breech presentations at term or overall rates of cesarean delivery. Additionally, if complications of ECV were to arise that warranted emergent delivery, it would result in a preterm neonate with its inherent risks. The Early External Cephalic Version (ECV) 2 trial was an international, multicentered, randomized clinical trial that compared ECV performed at 34-35 weeks’ gestation compared with 37 weeks’ gestation or more. [ 27 ] Early ECV increased the chance of cephalic presentation at birth; however, no difference in cesarean delivery rates was noted, along with a nonstatistical increase in preterm births.
A systematic review looked at 5 studies of ECV completed prior to 37 weeks and concluded that compared with no ECV attempt, ECV commenced before term reduces the non-cephalic presentation at birth, however early ECV may increase the risk of late preterm birth. [ 28 ]
Given the increasing awareness of the risks of late preterm birth and early term deliveries, the higher success of earlier ECV should be weighed against the risks of iatrogenic prematurity should a complication arise necessitating delivery.
Contraindications
Absolute contraindications for ECV include multiple gestations with a breech presenting fetus, contraindications to vaginal delivery (eg, herpes simplex virus infection, placenta previa), and nonreassuring fetal heart rate tracing.
Relative contraindications include polyhydramnios or oligohydramnios , fetal growth restriction , uterine malformation , and major fetal anomaly.
Controversial candidates
Women with prior uterine incisions may be candidates for ECV, but data are scant. In 1991, Flamm et al attempted ECV on 56 women with one or more prior low transverse cesarean deliveries. [ 29 ] The success rate of ECV was 82%, with successful vaginal births in 65% of patients with successful ECVs. No uterine ruptures occurred during attempted ECV or subsequent labor, and no significant fetal complications occurred.
In 2010 ACOG acknowledged that although there is limited data in both the above study and one more recently, [ 30 ] no serious adverse events occurred in these series. A larger prospective cohort study that was published in 2014 reported similar success rates of ECV among women with and without prior cesarean section, although lower vaginal birth rates. There were, however, no cases of uterine rupture or other adverse outcomes. [ 31 ]
Another controversial area is performing ECV on a woman in active labor. In 1985, Ferguson and Dyson reported on 15 women in labor with term breeches and intact membranes. [ 32 ] Four patients were dilated greater than 5 cm (2 women were dilated 8 cm). Tocolysis was administered, and intrapartum ECV was attempted. ECV was successful in 11 of 15 patients, with successful vaginal births in 10 patients. No adverse effects were noted. Further studies are needed to evaluate the safety and efficacy of intrapartum ECV.
Data regarding the benefit of intravenous or subcutaneous beta-mimetics in improving ECV rates are conflicting.
In 1996, Marquette et al performed a prospective, randomized, double-blinded study on 283 subjects with breech presentations between 36 and 41 weeks' gestation. [ 33 ] Subjects received either intravenous ritodrine or placebo. The success rate of ECV was 52% in the ritodrine group versus 42% in the placebo group ( P = .35). When only nulliparous subjects were analyzed, significant differences were observed in the success of ECV (43% vs 25%, P < .03). ECV success rates were significantly higher in parous versus nulliparous subjects (61% vs 34%, P < .0001), with no additional improvement with ritodrine.
A systematic review published in 2015 of six randomized controlled trials of ECV that compared the use of parenteral beta-mimetic tocolysis during ECV concluded that tocolysis was effective in increasing the rate of cephalic presentation in labor and reducing the cesarean delivery rate by almost 25% in both nulliparous and multiparous women. [ 34 ] Data on adverse effects and other tocolytics was insufficient. A review published in 2011 on Nifedipine did not show an improvement in ECV success. [ 35 ]
Regional anesthesia
Regional analgesia, either epidural or spinal, may be used to facilitate external cephalic version (ECV) success. When analgesia levels similar to that for cesarean delivery are given, it allows relaxation of the anterior abdominal wall, making palpation and manipulation of the fetal head easier. Epidural or spinal analgesia also eliminates maternal pain that may cause bearing down and tensing of the abdominal muscles. If ECV is successful, the epidural can be removed and the patient sent home to await spontaneous labor. If ECV is unsuccessful, a patient can proceed to cesarean delivery under her current anesthesia, if the gestational age is more than 39 weeks.
The main disadvantage is the inherent risk of regional analgesia, which is considered small. Additionally, lack of maternal pain could potentially result in excessive force being applied to the fetus without the knowledge of the operator.
In 1994, Carlan et al retrospectively analyzed 61 women who were at more than 36 weeks' gestation and had ECV with or without epidural. [ 36 ] The success rate of ECV was 59% in the epidural group and 24% in the nonepidural group ( P < .05). In 7 of 8 women with unsuccessful ECV without epidural, a repeat ECV attempt after epidural was successful. No adverse effects on maternal or perinatal morbidity or mortality occurred.
In 1997, Schorr et al randomized 69 subjects who were at least 37 weeks' gestation to either epidural or control groups prior to attempted ECV. [ 37 ] Those in whom ECV failed underwent cesarean delivery. The success rate of ECV was 69% in the epidural group and 32% in the control group (RR, 2.12; 95% CI, 1.24-3.62). The cesarean delivery rate was 79% in the control group and 34% in the epidural group ( P = .001). No complications of epidural anesthesia and no adverse fetal effects occurred.
In 1999, Dugoff et al randomized 102 subjects who were at more than 36 weeks' gestation with breech presentations to either spinal anesthesia or a control group. [ 38 ] All subjects received 0.25 mg terbutaline subcutaneously. The success rate of ECV was 44% in the spinal group and 42% in the nonspinal group, which was not statistically significant.
In contrast, a 2007 randomized clinical trial of spinal analgesia versus no analgesia in 74 women showed a significant improvement in ECV success (66.7% vs 32.4%, p = .004), with a significantly lower pain score by the patient. [ 39 ]
The 2015 systematic review asserted that regional analgesia in combination with a tocolytic was more effective than the tocolytic alone for increasing ECV success; however there was no difference in cephalic presentation in labor. Data from the same review was insufficient to assess regional analgesia without tocolysis [ 34 ]
Acoustic stimulation
Johnson and Elliott performed a randomized, blinded trial on 23 subjects to compare acoustic stimulation prior to ECV with a control group when the fetal spine was in the midline (directly back up or back down). [ 40 ] Of those who received acoustic stimulation, 12 of 12 fetuses shifted to a spine-lateral position after acoustic stimulation, and 11 (91%) underwent successful ECV. In the control group, 0 of 11 shifts and 1 (9%) successful ECV ( P < .0001) occurred. Additional studies are needed.
Amnioinfusion
Although an earlier study reported on the utility of amnioinfusion to successfully turn 6 fetuses who initially failed ECV, [ 41 ] a subsequent study was published of 7 women with failed ECV who underwent amniocentesis and amnioinfusion of up to 1 liter of crystalloid. [ 42 ] Repeat attempts of ECV were unsuccessful in all 7 cases. Amnioinfusion to facilitate ECV cannot be recommended at this time.
Vaginal delivery rates after successful version
The rate of cesarean delivery ranges from 0-31% after successful external cephalic version (ECV). Controversy has existed on whether there is a higher rate of cesarean delivery for labor dystocia following ECV. In 1994, a retrospective study by Egge et al of 76 successful ECVs matched with cephalic controls by delivery date, parity, and gestational age failed to note any significant difference in the cesarean delivery rate (8% in ECV group, 6% in control group). [ 43 ]
However, in 1997, Lau et al compared 154 successful ECVs to 308 spontaneously occurring cephalic controls (matched for age, parity, and type of labor onset) with regard to the cesarean delivery rate. [ 44 ] Cesarean delivery rates were higher after ECV (16.9% vs 7.5%, P < .005) because of higher rates of cephalopelvic disproportion and nonreassuring fetal heart rate tracings. This may be related to an increased frequency of compound presentations after ECV. Immediate induction of labor after successful ECV may also contribute to an increase in the cesarean delivery rate due to failed induction in women with unripe cervices and unengaged fetal heads.
Further, in another cohort study from 2015, factors were described which decreased the vaginal delivery rate after successful ECV including labor induction, less than 2 weeks between ECV and delivery, high body mass index, and previous cesarean. [ 45 ] The overall caesarean delivery rate in this cohort was 15%.
Vaginal breech delivery requires an experienced obstetrician and careful counseling of the parents. Although studies on the delivery of the preterm breech are limited, the multicenter Term Breech Trial found an increased rate of perinatal mortality and serious immediate perinatal morbidity, though no differences were seen in infant outcome at 2 years of age.
Parents must be informed about potential risks and benefits to the mother and neonate for both vaginal breech delivery and cesarean delivery. Discussion of risks should not be limited only to the current pregnancy. The risks of a cesarean on subsequent pregnancies, including uterine rupture and placental attachment abnormalities ( placenta previa , abruption , accreta), as well as maternal and perinatal sequelae from these complications, should be reviewed as well.
It remains concerning that the dearth of experienced physicians to teach younger practitioners will lead to the abandonment of vaginal breeches altogether. For those wishing to learn the art of vaginal breech deliveries, simulation training with pelvic models has been advocated to familiarize trainees with the procedure in a nonthreatening environment. [ 46 ] Once comfortable with the appropriate maneuvers, vaginal delivery of the second, noncephalic twin, may be attempted under close supervision by an experienced physician. The cervix will already be fully dilated, and, assuming the second twin is not significantly larger, the successful vaginal delivery rate has been quoted to be as high as 96%.
External cephalic version (ECV) is a safe alternative to vaginal breech delivery or cesarean delivery, reducing the cesarean delivery rate for breech by 50%. ACOG recommends offering ECV to all women with a breech fetus near term. [ 24 ] Adjuncts such as tocolysis, regional anesthesia, and acoustic stimulation when appropriate may improve ECV success rates.
Hickok DE, Gordon DC, Milberg JA, Williams MA, Daling JR. The frequency of breech presentation by gestational age at birth: a large population-based study. Am J Obstet Gynecol . 1992 Mar. 166(3):851-2. [QxMD MEDLINE Link] .
Wright RC. Reduction of perinatal mortality and morbidity in breech delivery through routine use of cesarean section. Obstet Gynecol . 1959. 14:758-63.
Cheng M, Hannah M. Breech delivery at term: a critical review of the literature. Obstet Gynecol . 1993 Oct. 82(4 Pt 1):605-18. [QxMD MEDLINE Link] .
Ballas S, Toaff R. Hyperextension of the fetal head in breech presentation: radiological evaluation and significance. Br J Obstet Gynaecol . 1976 Mar. 83(3):201-4. [QxMD MEDLINE Link] .
Ophir E, Oettinger M, Yagoda A, Markovits Y, Rojansky N, Shapiro H. Breech presentation after cesarean section: always a section?. Am J Obstet Gynecol . 1989 Jul. 161(1):25-8. [QxMD MEDLINE Link] .
Green JE, McLean F, Smith LP, Usher R. Has an increased cesarean section rate for term breech delivery reduced in incidence of birth asphyxia, trauma, and death?. Am J Obstet Gynecol . 1982 Mar 15. 142(6 Pt 1):643-8. [QxMD MEDLINE Link] .
Collea JV, Chein C, Quilligan EJ. The randomized management of term frank breech presentation: a study of 208 cases. Am J Obstet Gynecol . 1980 May 15. 137(2):235-44. [QxMD MEDLINE Link] .
Gimovsky ML, Wallace RL, Schifrin BS, Paul RH. Randomized management of the nonfrank breech presentation at term: a preliminary report. Am J Obstet Gynecol . 1983 May 1. 146(1):34-40. [QxMD MEDLINE Link] .
Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet . 2000 Oct 21. 356(9239):1375-83. [QxMD MEDLINE Link] .
Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol . 2004 Sep. 191(3):864-71. [QxMD MEDLINE Link] .
Hannah ME, Whyte H, Hannah WJ, Hewson S, Amankwah K, Cheng M. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol . 2004 Sep. 191(3):917-27. [QxMD MEDLINE Link] .
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev . 2015 Jul 21. 7:CD000166. [QxMD MEDLINE Link] .
Zlatnik FJ. The Iowa premature breech trial. Am J Perinatol . 1993 Jan. 10(1):60-3. [QxMD MEDLINE Link] .
Bergenhenegouwen L, Vlemmix F, Ensing S, Schaaf J, van der Post J, Abu-Hanna A, et al. Preterm Breech Presentation: A Comparison of Intended Vaginal and Intended Cesarean Delivery. Obstet Gynecol . 2015 Dec. 126 (6):1223-30. [QxMD MEDLINE Link] .
Caning MM, Rasmussen SC, Krebs L. Maternal outcomes of planned mode of delivery for term breech in nulliparous women. PLoS One . 2024. 19 (4):e0297971. [QxMD MEDLINE Link] . [Full Text] .
Eller DP, VanDorsten JP. Route of delivery for the breech presentation: a conundrum. Am J Obstet Gynecol . 1995 Aug. 173(2):393-6; discussion 396-8. [QxMD MEDLINE Link] .
Zhang J, Bowes WA Jr, Fortney JA. Efficacy of external cephalic version: a review. Obstet Gynecol . 1993 Aug. 82(2):306-12. [QxMD MEDLINE Link] .
Zielbauer AS, Louwen F, Jennewein L. External cephalic version at 38 weeks' gestation at a specialized German single center. PLoS One . 2021. 16 (8):e0252702. [QxMD MEDLINE Link] . [Full Text] .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev . 2015 Apr 1. 4:CD000083. [QxMD MEDLINE Link] .
de Hundt M, Velzel J, de Groot CJ, Mol BW, Kok M. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol . 2014 Jun. 123 (6):1327-34. [QxMD MEDLINE Link] .
de Hundt M, Vlemmix F, Bais JM, de Groot CJ, Mol BW, Kok M. Risk factors for cesarean section and instrumental vaginal delivery after successful external cephalic version. J Matern Fetal Neonatal Med . 2016 Jun. 29 (12):2005-7. [QxMD MEDLINE Link] .
Cook HA. Experience with external cephalic version and selective vaginal breech delivery in private practice. Am J Obstet Gynecol . 1993 Jun. 168(6 Pt 1):1886-9; discussion 1889-90. [QxMD MEDLINE Link] .
Gifford DS, Keeler E, Kahn KL. Reductions in cost and cesarean rate by routine use of external cephalic version: a decision analysis. Obstet Gynecol . 1995 Jun. 85(6):930-6. [QxMD MEDLINE Link] .
Practice Bulletin No. 161 Summary: External Cephalic Version. Obstet Gynecol . 2016 Feb. 127 (2):412-3. [QxMD MEDLINE Link] .
[Guideline] External Cephalic Version: ACOG Practice Bulletin, Number 221. Obstet Gynecol . 2020 May. 135 (5):e203-e212. [QxMD MEDLINE Link] .
[Guideline] ACOG Committee Opinion No. 745: Mode of Term Singleton Breech Delivery. Obstet Gynecol . 2018 Aug; reaffirmed 2023. 132 (2):e60-e63. [QxMD MEDLINE Link] . [Full Text] .
Hutton E, Hannah M, Ross S, Delisle MF, Carson G, Windrim R, et al. The Early External Cephalic Version (ECV) 2 Trial: an international multicentre randomised controlled trial of timing of ECV for breech pregnancies. BJOG . 2011 Apr. 118(5):564-577. [QxMD MEDLINE Link] .
Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev . 2015 Jul 29. 7:CD000084. [QxMD MEDLINE Link] .
Flamm BL, Fried MW, Lonky NM, Giles WS. External cephalic version after previous cesarean section. Am J Obstet Gynecol . 1991 Aug. 165(2):370-2. [QxMD MEDLINE Link] .
de Meeus JB, Ellia F, Magnin G. External cephalic version after previous cesarean section: a series of 38 cases. Eur J Obstet Gynecol Reprod Biol . 1998 Oct. 81 (1):65-8. [QxMD MEDLINE Link] .
Burgos J, Cobos P, Rodríguez L, Osuna C, Centeno MM, Martínez-Astorquiza T, et al. Is external cephalic version at term contraindicated in previous caesarean section? A prospective comparative cohort study. BJOG . 2014 Jan. 121 (2):230-5; discussion 235. [QxMD MEDLINE Link] .
Ferguson JE 2nd, Dyson DC. Intrapartum external cephalic version. Am J Obstet Gynecol . 1985 Jun 1. 152(3):297-8. [QxMD MEDLINE Link] .
Marquette GP, Boucher M, Theriault D, Rinfret D. Does the use of a tocolytic agent affect the success rate of external cephalic version?. Am J Obstet Gynecol . 1996 Oct. 175(4 Pt 1):859-61. [QxMD MEDLINE Link] .
Cluver C, Gyte GM, Sinclair M, Dowswell T, Hofmeyr GJ. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev . 2015 Feb 9. 2:CD000184. [QxMD MEDLINE Link] .
Wilcox CB, Nassar N, Roberts CL. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG . 2011 Mar. 118 (4):423-8. [QxMD MEDLINE Link] .
Carlan SJ, Dent JM, Huckaby T, Whittington EC, Shaefer D. The effect of epidural anesthesia on safety and success of external cephalic version at term. Anesth Analg . 1994 Sep. 79(3):525-8. [QxMD MEDLINE Link] .
Schorr SJ, Speights SE, Ross EL, et al. A randomized trial of epidural anesthesia to improve external cephalic version success. Am J Obstet Gynecol . 1997 Nov. 177(5):1133-7. [QxMD MEDLINE Link] .
Dugoff L, Stamm CA, Jones OW 3rd, Mohling SI, Hawkins JL. The effect of spinal anesthesia on the success rate of external cephalic version: a randomized trial. Obstet Gynecol . 1999 Mar. 93(3):345-9. [QxMD MEDLINE Link] .
Weiniger CF, Ginosar Y, Elchalal U, Sharon E, Nokrian M, Ezra Y. External cephalic version for breech presentation with or without spinal analgesia in nulliparous women at term: a randomized controlled trial. Obstet Gynecol . 2007 Dec. 110(6):1343-50. [QxMD MEDLINE Link] .
Johnson RL, Elliott JP. Fetal acoustic stimulation, an adjunct to external cephalic version: a blinded, randomized crossover study. Am J Obstet Gynecol . 1995 Nov. 173(5):1369-72. [QxMD MEDLINE Link] .
Benifla JL, Goffinet F, Darai E, Madelenat P. Antepartum transabdominal amnioinfusion to facilitate external cephalic version after initial failure. Obstet Gynecol . 1994 Dec. 84(6):1041-2. [QxMD MEDLINE Link] .
Adama van Scheltema PN, Feitsma AH, Middeldorp JM, Vandenbussche FP, Oepkes D. Amnioinfusion to facilitate external cephalic version after initial failure. Obstet Gynecol . 2006 Sep. 108(3 Pt 1):591-2. [QxMD MEDLINE Link] .
Egge T, Schauberger C, Schaper A. Dysfunctional labor after external cephalic version. Obstet Gynecol . 1994 May. 83(5 Pt 1):771-3. [QxMD MEDLINE Link] .
Lau TK, Lo KW, Rogers M. Pregnancy outcome after successful external cephalic version for breech presentation at term. Am J Obstet Gynecol . 1997 Jan. 176(1 Pt 1):218-23. [QxMD MEDLINE Link] .
Burgos J, Iglesias M, Pijoan JI, Rodriguez L, Fernández-Llebrez L, Martínez-Astorquiza T. Probability of cesarean delivery after successful external cephalic version. Int J Gynaecol Obstet . 2015 Nov. 131 (2):192-5. [QxMD MEDLINE Link] .
Deering S, Brown J, Hodor J, Satin AJ. Simulation training and resident performance of singleton vaginal breech delivery. Obstet Gynecol . 2006 Jan. 107(1):86-9. [QxMD MEDLINE Link] .
- Footling breech presentation. Once the feet have delivered, one may be tempted to pull on the feet. However, a singleton gestation should not be pulled by the feet because this action may precipitate head entrapment in an incompletely dilated cervix or may precipitate nuchal arms. As long as the fetal heart rate is stable and no physical evidence of a prolapsed cord is evident, management may be expectant while awaiting full cervical dilation.
- Assisted vaginal breech delivery. Thick meconium passage is common as the breech is squeezed through the birth canal. This is usually not associated with meconium aspiration because the meconium passes out of the vagina and does not mix with the amniotic fluid.
- Assisted vaginal breech delivery. The Ritgen maneuver is applied to take pressure off the perineum during vaginal delivery. Episiotomies are often performed for assisted vaginal breech deliveries, even in multiparous women, to prevent soft tissue dystocia.
- Assisted vaginal breech delivery. No downward or outward traction is applied to the fetus until the umbilicus has been reached.
- Assisted vaginal breech delivery. With a towel wrapped around the fetal hips, gentle downward and outward traction is applied in conjunction with maternal expulsive efforts until the scapula is reached. An assistant should be applying gentle fundal pressure to keep the fetal head flexed.
- Assisted vaginal breech delivery. After the scapula is reached, the fetus should be rotated 90° in order to deliver the anterior arm.
- Assisted vaginal breech delivery. The anterior arm is followed to the elbow, and the arm is swept out of the vagina.
- Assisted vaginal breech delivery. The fetus is rotated 180°, and the contralateral arm is delivered in a similar manner as the first. The infant is then rotated 90° to the backup position in preparation for delivery of the head.
- Assisted vaginal breech delivery. The fetal head is maintained in a flexed position by using the Mauriceau maneuver, which is performed by placing the index and middle fingers over the maxillary prominence on either side of the nose. The fetal body is supported in a neutral position, with care to not overextend the neck.
- Piper forceps application. Piper forceps are specialized forceps used only for the after-coming head of a breech presentation. They are used to keep the fetal head flexed during extraction of the head. An assistant is needed to hold the infant while the operator gets on one knee to apply the forceps from below.
- Assisted vaginal breech delivery. Low 1-minute Apgar scores are not uncommon after a vaginal breech delivery. A pediatrician should be present for the delivery in the event that neonatal resuscitation is needed.
- Assisted vaginal breech delivery. The neonate after birth.
- Ultrasound demonstrating a fetus in breech presentation with a hyperextended head (ie, "star gazing").

Contributor Information and Disclosures
Richard Fischer, MD Professor, Division Head, Department of Obstetrics and Gynecology, Division of Maternal-Fetal Medicine, Cooper University Hospital Richard Fischer, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Institute of Ultrasound in Medicine , Association of Professors of Gynecology and Obstetrics , Society for Maternal-Fetal Medicine Disclosure: Stock ownership for: Pfizer Pharmaceuticals (< 5% of portfolio); Johnson & Johnson (< 5% of portfolio).
Alisa B Modena, MD, FACOG Assistant Professor, Cooper Medical School of Rowan University; Attending Physician, Division of Maternal-Fetal Medicine, Cooper University Hospital Alisa B Modena, MD, FACOG is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Institute of Ultrasound in Medicine , Philadelphia Perinatal Society, Society for Maternal-Fetal Medicine Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference Disclosure: Received salary from Medscape for employment. for: Medscape.
Richard S Legro, MD Professor, Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology, Pennsylvania State University College of Medicine; Consulting Staff, Milton S Hershey Medical Center Richard S Legro, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , Society of Reproductive Surgeons , American Society for Reproductive Medicine , Endocrine Society , Phi Beta Kappa Disclosure: Received honoraria from Korea National Institute of Health and National Institute of Health (Bethesda, MD) for speaking and teaching; Received honoraria from Greater Toronto Area Reproductive Medicine Society (Toronto, ON, CA) for speaking and teaching; Received honoraria from American College of Obstetrics and Gynecologists (Washington, DC) for speaking and teaching; Received honoraria from National Institute of Child Health and Human Development Pediatric and Adolescent Gynecology Research Thi.
Ronald M Ramus, MD Professor of Obstetrics and Gynecology, Director, Division of Maternal-Fetal Medicine, Virginia Commonwealth University School of Medicine Ronald M Ramus, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Institute of Ultrasound in Medicine , Medical Society of Virginia , Society for Maternal-Fetal Medicine Disclosure: Nothing to disclose.
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- HIV in Pregnancy
- Pulmonary Disease and Pregnancy
- Kidney Disease and Pregnancy
- Vaccinations/Immunizations During Pregnancy
- Common Pregnancy Complaints and Questions
- Shock and Pregnancy
- Pregnancy Diagnosis
- Is immunotherapy for cancer safe in pregnancy?
- Labetalol, Nifedipine: Outcome on Pregnancy Hypertension
- The Pregnancy Challenges of Women With Chronic Conditions

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 2020/viewarticle/immunotherapy-cancer-safe-pregnancy-2024a100083dnews news Is immunotherapy for cancer safe in pregnancy?

- 2002261369-overviewDiseases & Conditions Diseases & Conditions Postterm Pregnancy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Glob Health

Maternal and fetal risks of planned vaginal breech delivery vs planned caesarean section for term breech birth: A systematic review and meta-analysis
Francisco j fernández-carrasco.
1 Department of Gynaecology and Obstetrics, Punta de Europa Hospital, Cádiz, Spain
2 Nursing and Physiotherapy Department, Faculty of Nursing, University of Cádiz, Algeciras, Spain
Delia Cristóbal-Cañadas
3 Neonatal and Paediatric Intensive Care Unit, Torrecárdenas University Hospital, Almeria, Spain
Juan Gómez-Salgado
4 Department of Gynaecology and Obstetrics, Ceuta University Hospital, Midwifery Teaching Unit of Ceuta, University of Granada, Ceuta, Spain
5 Safety and Health Postgraduate Programme, Espíritu Santo University, Guyaquil, Ecuador
Juana M Vázquez-Lara
6 Department of Gynaecology and Obbstetrics, Ceuta University Hospital, Midwifery Teaching Unit of Ceuta, University of Granada, Ceuta, Spain
Luciano Rodríguez-Díaz
Tesifón parrón-carreño.
7 School of Health Sciences, University of Almeria, Almeria, Spain
8 Territorial Delegation of Equality, Health and Social Policies, Health Delegation of Almeria, Almeria, Spain
Associated Data
Breech presentation delivery approach is a controversial issue in obstetrics. How to cope with breech delivery (vaginal or C-section) has been discussed to find the safest in terms of morbidity. The aim of this study was to assess the risks of foetal and maternal mortality and perinatal morbidity associated with vaginal delivery against elective caesarean in breech presentations, as reported in observational studies.
Studies assessing perinatal morbidity and mortality associated with breech presentations births. Cochrane, Medline, Scopus, Embase, Web of Science, and Cuiden databases were consulted. This protocol was registered in PROSPERO CRD42020197598. Selection criteria were: years between 2010 and 2020, in English language, and full-term gestation (37-42 weeks). The methodological quality of the eligible articles was assessed according to the Newcastle-Ottawa scale. Meta-analyses were performed to study each parameter related to neonatal mortality and maternal morbidity.
The meta-analysis included 94 285 births with breech presentation. The relative risk of perinatal mortality was 5.48 (95% confidence interval (CI) = 2.61-11.51) times higher in the vaginal delivery group, 4.12 (95% CI = 2.46-6.89) for birth trauma and 3.33 (95% CI = 1.95-5.67) for Apgar results. Maternal morbidity showed a relative risk 0.30 (95% CI = 0.13-0.67) times higher in the planned caesarean group.
Conclusions
An increment in the risk of perinatal mortality, birth trauma, and Apgar lower than 7 was identified in planned vaginal delivery. However, the risk of severe maternal morbidity because of complications of a planned caesarean was slightly higher.
One of the most controversial topics in obstetrics in recent years has been the discussion about how to deal with breech delivery, whether vaginal or caesarean. Although caesarean is considered a safe way of treating breech delivery, it contributes to high rates of postpartum maternal morbidity in developed countries and it is known to cause significant complications such as anaemia, urinary tract infections, superficial or complete dehiscence of the operative wound, endometritis, inflammatory complications [ 1 ], muscle pain, headache, lack of sexual satisfaction after delivery, digestive problems, fever and infection, abnormal bleeding, and stress urinary incontinence [ 2 ].
However, in 2000, the authors of the Term Breech Trial Collaborative Group (TBT) [ 3 ] published a randomised multicentre collaborative study about how to deal with term breech delivery. They concluded that elective caesareans offered better results than vaginal deliveries in full-term foetuses with breech presentation, while maternal complications were similar between the two groups. So, according to this evidence, the practice of elective caesarean was fostered in such presentations [ 3 ]. Following this trend, the TBT recommendation was adopted by important organisations in many countries, opting for a scheduled caesarean before the end of gestation and this way preventing spontaneous breech vaginal delivery, and the attributed risks, from being triggered [ 4 ].
Subsequently, in 2006 the PREMODA multicentre study was published [ 5 ]. Based on this study, The American College of Obstetricians and Gynecologists changed their protocols that same year and concluded that vaginal delivery in breech presentation and single-term gestation was a reasonable option in properly selected pregnant women and experienced health workers [ 6 ].
Therefore, the TBT study [ 3 ] was called into question and some national associations [ 7 ] included the option of having a vaginal breech delivery in their childbirth care protocol for full-term breech presentation, allowing the free evolution of the delivery process, provided that there is specifically trained staff in the affected centre. This procedure is currently accepted [ 6 ].
Analysing the original TBT data [ 3 ], serious concerns were raised regarding the design of the study, methods, and conclusions. In a considerable number of cases, there was a lack of adherence to the inclusion criteria and there was great interinstitutional variation regarding the standards of care. Also, inadequate methods of foetal antepartum and intrapartum evaluation were used, and a large proportion of women were recruited during active delivery, in many cases, without assistance from a doctor with adequate experience [ 8 ].
Primary caesarean in the first pregnancy has been associated with neonatal and maternal adverse outcomes in subsequent delivery [ 9 ]. In this way, abandoning vaginal delivery with breech presentation and opting indiscriminately for a caesarean would mean denying women access to health care options [ 10 ].
The Cochrane review conducted by Hofmeyr et al., which focused on planned caesarean section for term breech delivery, concluded that it reduced perinatal and neonatal death as well as serious neonatal morbidity, at the expense of somewhat increased maternal morbidity compared with planned vaginal delivery. Authors suggested to consider mother's preference for vaginal birth and risks such as future pregnancy complications, and the option of external cephalic version [ 11 ].
The meta-analysis conducted by Berhan et al. [ 12 ] (1993-2014) aimed at assessing the risk of morbidity and perinatal mortality in breech, full-term and single-foetus deliveries. Results showed a higher relative risk in vaginal delivery for perinatal mortality, trauma at birth, and Apgar at the fifth minute of life.
The present meta-analysis sought to update scientific evidence with the latest studies published in the last 10 years (2010-2020), so the results would be a complementary update. The objective of this meta-analysis was to compare the risks of vaginal delivery with elective caesarean in breech presentations, in terms of neonatal mortality, perinatal trauma, Apgar, neonatal intensive care unit (ICU) admittance, and maternal morbidity, according to evidence published during the last 10 years.
Study design
A systematic review of observational studies and meta-analysis was conducted. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed [ 13 , 14 ].
A systematic bibliographic search was carried out using the Cochrane, Medline, Scopus, Embase, Web of Science, and Cuiden databases. Extensive searches were performed on the reference lists of selected articles. Our search terms included: “breech”, “breech presentation”, “breech birth”, “breech delivery”. During the process, search terms were alternately combined using Boolean logic. The search was based on a clinically answerable question in PICO format, Population (pregnant women with single, full-term foetus, and breech presentation); Intervention (vaginal delivery risks); Comparison (caesarean delivery risks) and Outcomes (risk of neonatal mortality, perinatal trauma, Apgar test with low score, neonatal ICU admittance, and maternal morbidity). Following this structure, the different search strategies were designed. The detailed search strategies employed in each database are summarised in Table S1 in the Online Supplementary Document .
This revision protocol was registered in PROSPERO.
Inclusion and selection criteria
For this study, the default inclusion criteria were:
- Observational studies of cohorts were included; reviews, brief reports, guidelines, and comments were excluded.
- Studies that assessed perinatal mortality and morbidity in relation to the type of delivery with breech presentation.
- Studies published in any language, between January 2010 and September 2020.
- Studies in which the samples were characterised by full-term gestations (between 37 and 42 weeks of gestation), with a single foetus, and breech presentation.
The authors decided to establish observational studies as an inclusion criterion as a review restricted to randomised controlled trials would have given an incomplete summary of the effects of a treatment, due to potential harms. Therefore, ClinicalTrials.gov was not consulted. The studies published before 2010 were excluded because recent scientific publications have turned other previously published ones into outdated evidence, and the aimed was to gather the latest reliable results. In addition, studies where foetuses had lethal congenital abnormalities and caesareans made by other obstetric indications such as multiple pregnancy or intrauterine foetal deaths were also excluded.
The selection of studies was carried out in three stages. First, after reviewing the titles, all relevant literature was retrieved from the respective databases. Second, summaries of all recovered articles were reviewed and then grouped as “eligible for inclusion” or “Not eligible for inclusion”. Third, articles that were grouped as “eligible for inclusion” were revised in detail for the final decision.
The entire process of selection, the quality assessment and also data extraction were carried out by two investigators independently. Each study was individually evaluated by one of the researchers and results were shared. In case of discrepancies, both researchers discussed their arguments and agreement was reached by consensus; occasionally, a third researcher’s assessment was required.
Methodological quality of the included studies
The methodological quality of the eligible articles was assessed according to the Newcastle-Ottawa scale. This scale was designed for assessing the quality of non-randomised studies included in a systematic review and/or meta-analyses. It contains eight items organised in three dimensions: the selection of the study groups (four items); the comparability of the groups (one item); and the ascertainment of the outcome (three items). Studies were evaluated following a star system such that each item can be awarded a maximum of one star, excepting the item related to comparability, which allows the assignment of two stars. The total score ranges between zero and nine stars [ 15 , 16 ].
Data extraction
To structure the collected data, all results compatible with perinatal mortality and morbidity in relation to the type of delivery with breech presentation in full-term gestations (between 37 and 42 weeks of gestation) with a single foetus were searched internationally. The results of the different items were compared on the basis of the primary outcomes, which were neonatal mortality, perinatal trauma, Apgar, neonatal ICU admittance, and maternal morbidity.
Data were extracted using a standard Excel (Microsoft, Redmond, WA, USA) spreadsheet. The extracted data included: the name of the first author, year of publication, period of study, country where the study was conducted in, conclusion of the study, sample size, type of delivery, intrapartum and neonatal mortality, perinatal trauma, Apgar score at the first and fifth minute of life, neonatal ICU admissions, and severe maternal morbidity.
In this review, neonatal mortality was considered as deaths before 7 days of age after birth. The WHO establishes early neonatal mortality up to the seventh day of life. Complications at birth as a result of childbirth are manifested in the first 7 days [ 17 ]. In fact, all the observational studies included in the present meta-analysis took this same period of time as a reference. Perinatal trauma included collarbone fracture, humerus or femur, intracerebral bleeding, cephalic haematoma, facial paralysis, brachial plexus injury, and other trauma.
For this study, severe maternal morbidity was considered as unexpected labour and delivery outcomes that result in significant short-term or long-term consequences for the woman's health. Serious complications of the intervention, whether caesarean or delivery, severe postpartum haemorrhages, neurological problems, sepsis, lung, kidney, or cardiac problems were included [ 18 ].
Statistical analysis
A meta-analysis was performed to evaluate each of the indicators that could measure morbidity and mortality in planned vaginal delivery and scheduled caesarean for breech presentations for both the newborn and the mother.
The Mantel-Haenszel method was used to obtain typical RR estimates and 95% confidence intervals (CI). Heterogeneity was determined using the Cochran’s Q χ 2 test and the I 2 values for the following variables:
(1) Early and incipient neonatal death, (2) birth trauma, (3) Apgar test score at 5 minutes, (4) neonatal admission to ICU, (5) severe maternal morbidity.
Heterogeneity between studies was assessed by calculating values for I 2 and P values. Due to the high I 2 , an important statistic for assessing heterogeneity, the random effects method was used. The I 2 value was interpreted as without heterogeneity (0%), low heterogeneity (<40%), moderate heterogeneity (<60%), substantial heterogeneity (<75%) and considerable heterogeneity (≥75%) [ 19 ]. The stability of the overall RR in the withdrawal of any of the studies was performed by sensitivity analysis (treating one study at a time). All meta-analyses were performed using the Epidat Software 3.0 (Xunta de Galicia, Santiago de Compostela, Spain).
Description of the included studies
The initial electronic search yielded a total of 19 055 references, and after removing duplicate records, 6802 references were reviewed. Of these, after reading the title and abstract, 6644 references were deleted for not meeting the inclusion criteria, so 158 were selected for full text review. Following the research protocol, 142 were excluded because they were not related to the current revision, because some made comparisons between breech and vertex presentation, and others assessed long-term maternal and neonatal complications. Finally, 16 articles were selected for meta-analysis [ 10 , 20 - 34 ]. The selection process is shown in Figure 1 .

PRISMA flowchart.
Of the 16 studies, 10 had been conducted in Europe, 2 in Asia, 2 in Oceania, and 2 in Africa. Of these, 4 were in favour of elective caesarean to minimise neonatal morbidity but recognised that this increased long-term maternal morbidity by conditioning the type of birth for a future pregnancy [ 10 , 21 , 27 , 34 ]. Two of the reviewed studies found that caesarean reduced the risk of neonatal mortality [ 10 , 21 ]. However, 12 of the studies involved in the meta-analysis concluded that vaginal delivery could be an acceptable option in breech presentation provided that strict criteria for the selection of cases were established [ 20 , 22 - 26 , 28 - 33 ]. Sample sizes for the studies included ranged from 111 to 58 320 ( Table 1 ).
Characteristics of the studies included in the meta-analysis
| Author, year | Country | Study period | Type of study | Number of breech deliveries | Attempted deliveries | Planned caesareans | Quality assessment | Conclusions |
|---|---|---|---|---|---|---|---|---|
| Vlemmix F et al, 2014 [ ] | Netherlands | 1999-2007 | Cohort | 58 320 | 27 817 | 30 503 | High quality | The more caesareans, the less mortality and neonatal morbidity, but mothers will end up with scarred uterus for future pregnancies. |
| Babovic I et al, 2010 [ ] | Serbia | 2007-2008 | Cohort | 401 | 267 | 134 | High quality | No deaths or nervous system injuries in any of the groups |
| Tharin HJE et al, 2011 [ ] | Denmark | Jan1997-2008 | Cohort | 21 803 | 7039 | 14 764 | High quality | Caesarean decreases child mortality, Apgar values at 5 min are higher, and less ICU admittances are required. Strict selection does not reduce the risks of vaginal delivery. |
| Singh A et al, 2012 [ ] | India | 2007-2009 | Cohort | 111 | 60 | 51 | High quality | With strict selection of women, vaginal delivery would be a feasible option. |
| Toivonen E et al, 2012 [ ] | Finlandia | 2004-2009 | Cohort | 751 | 254 | 497 | High quality | Vaginal delivery would be an acceptable option by accurately selecting cases. |
| Vistad I et al, 2013 [ ] | Norway | 2001-2011 | Cohort | 568 | 289 | 279 | High quality | Vaginal delivery would be an acceptable option through strict selection and control. |
| Foster BA et al 2014 [ ] | Australia | Oct 1999- Dec 2010 | Cohort | 766 | 243 | 523 | High quality | Fewer complications in vaginal delivery than in studies in other countries. Therefore, an acceptable option. |
| Babovic I et al, 2016 [ ] | Serbia | 2013 | Cohort | 146 | 72 | 74 | High quality | Caesarean delivery is best in nulliparous women over 35 y of age or women whose estimated foetal weight is greater than 3500 g. For all other cases, vaginal delivery would be an acceptable option. |
| Bin YS et al, 2016 [ ] | Australia | 2009-2012 | Cohort | 5197 | 352 | 4845 | High quality | Vaginal delivery causes more neonatal and maternal morbidity. Therefore, caesarean is recommended for all breech births. |
| Högberg U et al, 2016 [ ] | Tanzania | 1999-2010 | Cohort | 1655 | 908 | 747 | High quality | Low-income country. Vaginal delivery is associated with perinatal risk. But caesarean doesn't work better. Therefore, they opt for vaginal delivery. |
| Abdessalami S et al, 2017 [ ] | Netherlands | 2007-2015 | Cohort | 309 | 119 | 190 | High quality | Vaginal delivery is an option in selected women with low risk but is strongly influenced by the counselling technique, which is not always based on scientific evidence. |
| Fonseca A et al, 2017 [ ] | Portugal | Jan 2012 – Oct 2014 | Cohort | 1327 | 65 | 1262 | High quality | Both delivery pathways are acceptable, with no more risks in vaginal deliveries than in caesareans. |
| Debero-Mere T et al, 2017 [ ] | Ethiopia | 2013-2016 | Cohort | 384 | 317 | 67 | High quality | Low-income country. Vaginal delivery implies a higher risk in women over the age of 35, with large foetuses and poor cervical conditions. If cases are accurately selected, vaginal delivery seems a safe option. |
| Louwen F et al, 2017 [ ] | Germany | Jan 204- Jun 2011 | Cohort | 747 | 433 | 314 | High quality | Vaginal delivery with the woman upright is more successful than in the dorsal position. Therefore, vaginal delivery is an acceptable option. |
| Grupta V et al, 2019 [ ] | India | 2016-2017 | Cohort | 180 | 127 | 53 | High quality | Vaginal delivery is an option when carefully selecting cases. |
| Vinkenvleugel DAM et al 2020 [ ] | Netherlands | 2011-2017 | Cohort | 1620 | 425 | 1195 | High quality | Elective caesarean would be safer for newborns, but worse for the mother as it conditions the birth pathway for future pregnancy. Therefore, vaginal delivery will be attempted as long as it can be cared for by an experienced person and the conditions are strictly selected. |
Regarding methodological quality assessment, the included studies were scored from 5 to 9 stars according to de Newcastle-Ottawa scale ( Table 2 ). The publication bias was analysed, and results were summarised in Figure S1 and Figure S2 in the Online Supplementary Document .
Methodological quality assessment and quality of evidence*
| Author, year | Selection | Comparability | Outcome | GRADE (quality of evidence) |
|---|---|---|---|---|
| Abdessalami S et al, 2017 [ ] | * * * * | * * | * * * | 2++ |
| Babovic I et al, 2010 [ ] | * * * * | * * | * * * | 2++ |
| Babovic I et al, 2016 [ ] | * * * * | * * | * * * | 2++ |
| Bin YS et al, 2016 [ ] | * * * * | * * | * * * | 2++ |
| Debero-Mere T et al, 2017 [ ] | * * * | * * | * * | 2++ |
| Fonseca A et al, 2017 [ ] | * * * * | * * | * * * | 2++ |
| Foster Ab et al 2014 [ ] | * * * * | * * | * * * | 2++ |
| Grupta V et al, 2019 [ ] | * * * * | * * | * * * | 2++ |
| Högberg U et al, 2016 [ ] | * * * * | * * | * * * | 2++ |
| Louwen F et al, 2017 [ ] | * * * * | * * | * * * | 2++ |
| Singh A et al, 2012 [ ] | * * * | * * | * * * | 2+ |
| Tharin HJE et al, 2011 [ ] | * * | * | * * | 2 |
| Toivonen E et al, 2012 [ ] | * * * * | - | * * * | 2 |
| Vinkenvleugel DAM et al 2020 [ ] | * * * * | * * | * * * | 2++ |
| Vistad I et al, 2013 [ ] | * * * * | * * | * * * | 2++ |
| Vlemmix F et al, 2014 [ ] | * * * | * | * * * | 2+ |
*Selection: maximum score ****, Comparability: maximum score **, Outcome: maximum score ***. GRADE: 1 = high, 2 = moderate, 3 = low, 4 = very low.
Findings of the meta-analysis
Perinatal mortality analysis consisted of 16 studies and included 94 285 single foetus, full-term, breech presentation deliveries (38 787 planned vaginal deliveries and 55 498 scheduled caesareans). As shown in Figure 2 , perinatal mortality (intrapartum and early neonatal death) in the planned vaginal delivery group was 235 (0.6%), and in the elective caesarean group it was 76 (0.14%) (10,20-34). The grouped meta-analysis has shown that the risk of perinatal mortality was 5.48 (95% CI = 2.61 to 11.51) times higher in the vaginal delivery group than in the planned caesarean group. The overall heterogeneity of the tests showed substantial variability between studies (I 2 = 72%). Sensitivity analysis showed that the overall RR was 3.10; 95% CI = 1.8 - 5.2 (the detailed sensitivity analysis of each variable are summarised in Table S2 in the Online Supplementary Document ).

Meta-analysis of perinatal deaths in full-term singleton breech presentation (planned vaginal delivery vs planned caesarean section) (n = 94 285).
Perinatal trauma analysis included 70 143 single foetus, full-term, breech presentation deliveries (30 523 planned vaginal deliveries and 39 620 planned caesareans). As shown in Figure 3 , perinatal trauma in the planned vaginal delivery group was 285 (0.41%), and in the elective caesarean group it was 124 (0.18%) [ 10 , 20 , 22 - 25 , 27 , 29 , 30 , 32 - 34 ]. The grouped meta-analysis showed a 4.12 (95% CI = 2.46 to 6.89) times increased risk of birth trauma in the planned vaginal delivery group. The overall heterogeneity of the tests showed substantial variability between studies (I 2 = 70%). The sensitivity analysis showed that the overall RR was 3.6 95% CI = 2.17-6.09.

Meta-analysis of perinatal trauma in term singleton breech presentation (planned vaginal delivery vs planned caesarean section) (n = 70 143).
Regarding the Apgar score at minute 5, 13 studies were assessed including 92 135 deliveries with breech, single foetus, and term presentations (37 502 planned vaginal deliveries and 54 633 planned caesareans). 846 (0.92%) neonates of the planned vaginal delivery group had an Apgar below 7 points at the 5th minute of life. Also, in the planned caesarean group, there were 218 (0.24%) neonates whose test score was less than 7 points at 5 minutes of life [ 10 , 20 , 21 , 23 - 27 , 29 , 30 , 32 , 33 ] ( Figure 4 ). The grouped meta-analysis showed a nearly 3.33 (95% CI = 1.95-5.67) times higher risk of the Apgar test having a score of less than 7 points in the planned vaginal delivery group. The overall heterogeneity of the tests showed considerable variability between studies (I 2 = 86%). However, the sensitivity analysis showed that the overall RR was 3.8 95% CI = 2.07-7.25.

Meta-analysis of 5-minute Apgar <7 score in term singleton breech presentation (planned vaginal delivery vs planned caesarean section) (n = 92 135).
Admittance to neonatal ICU assessment included 9 studies, 32 438 single foetus, full-term, breech presentation deliveries (9053 planned vaginal deliveries and 23 385 elective caesareans) were included. In the planned vaginal delivery group, there were 435 (1.86%) admittances at the ICU of newborns, while in the planned caesarean group, the figure was 869 (3.72%) [ 20 , 21 , 23 - 25 , 27 , 29 , 30 ] ( Figure 5 ). The grouped meta-analysis showed a 1.90 (95% CI = 1.34-2.70) times increased risk of admittance to ICU in the planned vaginal delivery group. The overall heterogeneity of the tests showed substantial variability between studies (I 2 = 64%). However, the sensitivity analysis showed that the overall RR was 1.9 (95% CI = 1.36-2.76).

Meta-analysis of intensive care unit (ICU) admissions in term, singleton breech presentation (planned vaginal delivery vs planned caesarean section) (n = 32 438).
Regarding maternal morbidity, the analysis included 4 studies. 4007 single foetus, full-term, breech presentation deliveries were included (863 planned vaginal deliveries and 3144 planned caesareans) [ 23 , 27 , 30 , 34 ] ( Figure 6 ). Maternal morbidity was found in 6 cases (0.69%) for the planned vaginal delivery group, and in 83 cases (2.64%) for the planned caesarean group. The grouped meta-analysis showed a 0.30 (95% CI = 0.13-0.67) times reduced risk of severe maternal morbidity in the planned vaginal delivery group than in the planned caesarean group. The overall heterogeneity of the tests showed very low variability between studies (I 2 = 0%).

Meta-analysis of severe maternal morbidity in term singleton breech presentation (planned vaginal delivery vs planned caesarean section) (n = 4007).
Main findings
The meta-analysis has shown a decreased relative risk perinatal mortality and morbidity in a planned caesarean as compared with a vaginal delivery when breech presentation.
Interpretation
Regardless of whether childbirth is done vaginally or through caesarean delivery, morbidity and mortality rates have been represented higher at breech births than at cephalic births [ 35 ]. Since the publication of TBT [ 3 ], several studies have shown increased morbidity and perinatal mortality with breech presentations in planned vaginal delivery vs planned caesarean [ 9 , 21 , 36 , 37 ]. These results were consistent with TBT [ 3 ] and PREMODA results [ 5 ].
Although the potential biases associated with the observational design of the studies included in this meta-analysis must be recognised, with the consequent caution in comparing results with similar previous studies, our results were in line with previous meta-analyses. According to Berhan et al. [ 12 ], the relative risk of perinatal mortality, trauma at birth, and Apgar at the fifth minute of life were higher in the planned vaginal delivery than in planned caesarean for term singleton breech (3.4 vs 6.3; 3.1 vs 4.2; and 4.7 vs 2.99, respectively). Our study, despite having included only observational studies, agreed with these outcomes.
For the severe maternal morbidity indicator, the present meta-analysis showed a relative risk of 0.30 in favour of vaginal delivery. This means that vaginal delivery is a protective factor against severe maternal morbidity. Although the risk is low, maternal morbidity and mortality increase as a result of complications of a planned caesarean for breech presentations [ 21 , 36 ]. Several studies claimed that planned caesarean may increase the risks for the mother as a result of scarred uterus [ 9 , 21 , 34 ], so the relative safety of planned caesarean should be weighed [ 9 , 38 ].
In the absence of a contraindication for vaginal delivery, a woman with a breech presentation foetus must be truthfully informed, considering the scientific evidence so far, of the risks and benefits of vaginal breech delivery and elective caesarean, so that the woman can decide and consent to the desired type of delivery [ 29 , 39 ]. The woman's decision must be respected and, to do so, the staff attending births must be trained and updated in the assistance of breech vaginal deliveries [ 39 , 40 ]. Otherwise, the woman will be denied a medical treatment option to which she could have turned to [ 40 ].
Regardless of the way of planning the type of delivery, vaginal delivery in breech presentation will always exist, as a delivery may always become urgent and present with these characteristics. Therefore, it is essential that staff attending births do not lose this ability and master it in order to provide quality health care to women [ 39 ].
Strengths and limitations
The risks for neonatal mortality and maternal morbidity implies an ethical dilemma: assuming either the risk of neonatal mortality or the risk of severe maternal morbidity. The risk of neonatal mortality was higher; therefore, we would only consider exposing the mother and foetus to vaginal delivery in the case of good obstetric conditions and given that the health care professional is well trained and experienced in these procedures. Otherwise, we recommend delivery by caesarean section. Our study bases the practice of individualisation on decision-making when choosing the type of delivery in unique gestations with full-term foetuses and breech presentation. Each pregnancy should assess the risks individually, considering the woman's preferences and the context, and seeking a balance between neonatal mortality and maternal morbidity.
Some limitations have been found in conducting this research, starting with the great variability regarding the size of the samples. Studies with very small samples have had little weight when calculating RR in the grouped meta-analysis, while studies with a very large sample size had much more weight. For this reason, we have had to accept a relatively high (moderate) percentage of heterogeneity (I 2 ) in some meta-analyses as, if eliminated, the sample would be drastically reduced.
Vaginal, breech, full-term delivery with a single foetus had a higher risk of morbidity and perinatal mortality than caesarean delivery under the same conditions. Still, the results of this meta-analysis suggested that the risk of vaginal breech delivery is lower than in the results of other previously published studies [ 29 - 31 , 33 , 34 ].
Additionally, the potential bias accompanying observational studies should be acknowledged, given the Newcastle-Ottawa tool identified some items with lack of quality. Therefore, caution is suggested when comparing and generalising the results.
CONCLUSIONS
Term breech birth risks have been analysed according to two possibilities: Vaginal delivery and caesarean delivery risks. Caesarean had high rates of postpartum maternal morbidity. Also, there is no evidence of reduced child perinatal morbidity or mortality. Otherwise, there is no contraindication for vaginal delivery in breech presentation in selected pregnant women and in the presence of experienced health workers.
Our results could help in decision-making related to breech delivery, individualising the decision for each case by knowing the risks associated with each option. From an ethical perspective, the issue addressed in the review is highly sensitive, considering the risk of maternal morbidity and the risk of neonatal mortality. For this reason, further research is suggested that consolidates the available evidence for decision-making between the studied delivery methods.
Additional material
Funding : None.
Authors contributions : Conceptualization, FJFC, DCC, JMVL, TPC and LRD; Data curation, FJFC and DCC; Formal analysis, FJFC, DCC, JGS, JMVL, TPC and LRD; Investigation, FJFC, DCC, JGS, JMVL and TPC; Methodology, FJFC, JGS, JMVL, TPC and LRD; Project administration, TPC and LRD; Resources, DCC, JGS, JMVL and LRD; Software, FJFC, DCC, JGS and LRD; Supervision, JMVL, TPC and LRD; Validation, DCC, JGS, JMVL and TPC; Visualization, TPC; Writing – original draft, FJFC, DCC and JMVL; Writing – review & editing, JGS, JMVL, TPC and LRD.
Disclosure of interest: The authors completed the ICMJE Disclosure of Interest Form (available upon request from the corresponding author) and declare no conflicts of interest.
Breech baby at the end of pregnancy
Published: July 2017
Please note that this information will be reviewed every 3 years after publication.
This patient information page provides advice if your baby is breech towards the end of pregnancy and the options available to you.
It may also be helpful if you are a partner, relative or friend of someone who is in this situation.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information is for you if your baby remains in the breech position after 36 weeks of pregnancy. Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies.
This information includes:
- What breech is and why your baby may be breech
- The different types of breech
- The options if your baby is breech towards the end of your pregnancy
- What turning a breech baby in the uterus involves (external cephalic version or ECV)
- How safe ECV is for you and your baby
- Options for birth if your baby remains breech
- Other information and support available
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms .
- Breech is very common in early pregnancy, and by 36–37 weeks of pregnancy most babies will turn into the head-first position. If your baby remains breech, it does not usually mean that you or your baby have any problems.
- Turning your baby into the head-first position so that you can have a vaginal delivery is a safe option.
- The alternative to turning your baby into the head-first position is to have a planned caesarean section or a planned vaginal breech birth.
Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies. Breech is very common in early pregnancy, and by 36-37 weeks of pregnancy, most babies turn naturally into the head-first position.
Towards the end of pregnancy, only 3-4 in every 100 (3-4%) babies are in the breech position.
A breech baby may be lying in one of the following positions:
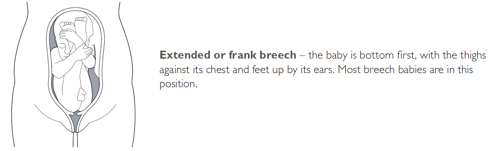
It may just be a matter of chance that your baby has not turned into the head-first position. However, there are certain factors that make it more difficult for your baby to turn during pregnancy and therefore more likely to stay in the breech position. These include:
- if this is your first pregnancy
- if your placenta is in a low-lying position (also known as placenta praevia); see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
- if you have too much or too little fluid ( amniotic fluid ) around your baby
- if you are having more than one baby.
Very rarely, breech may be a sign of a problem with the baby. If this is the case, such problems may be picked up during the scan you are offered at around 20 weeks of pregnancy.
If your baby is breech at 36 weeks of pregnancy, your healthcare professional will discuss the following options with you:
- trying to turn your baby in the uterus into the head-first position by external cephalic version (ECV)
- planned caesarean section
- planned vaginal breech birth.
What does ECV involve?
ECV involves applying gentle but firm pressure on your abdomen to help your baby turn in the uterus to lie head-first.
Relaxing the muscle of your uterus with medication has been shown to improve the chances of turning your baby. This medication is given by injection before the ECV and is safe for both you and your baby. It may make you feel flushed and you may become aware of your heart beating faster than usual but this will only be for a short time.
Before the ECV you will have an ultrasound scan to confirm your baby is breech, and your pulse and blood pressure will be checked. After the ECV, the ultrasound scan will be repeated to see whether your baby has turned. Your baby’s heart rate will also be monitored before and after the procedure. You will be advised to contact the hospital if you have any bleeding, abdominal pain, contractions or reduced fetal movements after ECV.
ECV is usually performed after 36 or 37 weeks of pregnancy. However, it can be performed right up until the early stages of labour. You do not need to make any preparations for your ECV.
ECV can be uncomfortable and occasionally painful but your healthcare professional will stop if you are experiencing pain and the procedure will only last for a few minutes. If your healthcare professional is unsuccessful at their first attempt in turning your baby then, with your consent, they may try again on another day.
If your blood type is rhesus D negative, you will be advised to have an anti-D injection after the ECV and to have a blood test. See the NICE patient information Routine antenatal anti-D prophylaxis for women who are rhesus D negative , which is available at: www.nice.org.uk/guidance/ta156/informationforpublic .
Why turn my baby head-first?
If your ECV is successful and your baby is turned into the head-first position you are more likely to have a vaginal birth. Successful ECV lowers your chances of requiring a caesarean section and its associated risks.
Is ECV safe for me and my baby?
ECV is generally safe with a very low complication rate. Overall, there does not appear to be an increased risk to your baby from having ECV. After ECV has been performed, you will normally be able to go home on the same day.
When you do go into labour, your chances of needing an emergency caesarean section, forceps or vacuum (suction cup) birth is slightly higher than if your baby had always been in a head-down position.
Immediately after ECV, there is a 1 in 200 chance of you needing an emergency caesarean section because of bleeding from the placenta and/or changes in your baby’s heartbeat.
ECV should be carried out by a doctor or a midwife trained in ECV. It should be carried out in a hospital where you can have an emergency caesarean section if needed.
ECV can be carried out on most women, even if they have had one caesarean section before.
ECV should not be carried out if:
- you need a caesarean section for other reasons, such as placenta praevia; see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
- you have had recent vaginal bleeding
- your baby’s heart rate tracing (also known as CTG) is abnormal
- your waters have broken
- you are pregnant with more than one baby; see the RCOG patient information Multiple pregnancy: having more than one baby .
Is ECV always successful?
ECV is successful for about 50% of women. It is more likely to work if you have had a vaginal birth before. Your healthcare team should give you information about the chances of your baby turning based on their assessment of your pregnancy.
If your baby does not turn then your healthcare professional will discuss your options for birth (see below). It is possible to have another attempt at ECV on a different day.
If ECV is successful, there is still a small chance that your baby will turn back to the breech position. However, this happens to less than 5 in 100 (5%) women who have had a successful ECV.
There is no scientific evidence that lying down or sitting in a particular position can help your baby to turn. There is some evidence that the use of moxibustion (burning a Chinese herb called mugwort) at 33–35 weeks of pregnancy may help your baby to turn into the head-first position, possibly by encouraging your baby’s movements. This should be performed under the direction of a registered healthcare practitioner.
Depending on your situation, your choices are:
There are benefits and risks associated with both caesarean section and vaginal breech birth, and these should be discussed with you so that you can choose what is best for you and your baby.
Caesarean section
If your baby remains breech towards the end of pregnancy, you should be given the option of a caesarean section. Research has shown that planned caesarean section is safer for your baby than a vaginal breech birth. Caesarean section carries slightly more risk for you than a vaginal birth.
Caesarean section can increase your chances of problems in future pregnancies. These may include placental problems, difficulty with repeat caesarean section surgery and a small increase in stillbirth in subsequent pregnancies. See the RCOG patient information Choosing to have a caesarean section .
If you choose to have a caesarean section but then go into labour before your planned operation, your healthcare professional will examine you to assess whether it is safe to go ahead. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
Vaginal breech birth
After discussion with your healthcare professional about you and your baby’s suitability for a breech delivery, you may choose to have a vaginal breech birth. If you choose this option, you will need to be cared for by a team trained in helping women to have breech babies vaginally. You should plan a hospital birth where you can have an emergency caesarean section if needed, as 4 in 10 (40%) women planning a vaginal breech birth do need a caesarean section. Induction of labour is not usually recommended.
While a successful vaginal birth carries the least risks for you, it carries a small increased risk of your baby dying around the time of delivery. A vaginal breech birth may also cause serious short-term complications for your baby. However, these complications do not seem to have any long-term effects on your baby. Your individual risks should be discussed with you by your healthcare team.
Before choosing a vaginal breech birth, it is advised that you and your baby are assessed by your healthcare professional. They may advise against a vaginal birth if:
- your baby is a footling breech (one or both of the baby’s feet are below its bottom)
- your baby is larger or smaller than average (your healthcare team will discuss this with you)
- your baby is in a certain position, for example, if its neck is very tilted back (hyper extended)
- you have a low-lying placenta (placenta praevia); see the RCOG patient information Placenta Praevia, placenta accreta and vasa praevia
- you have pre-eclampsia or any other pregnancy problems; see the RCOG patient information Pre-eclampsia .
With a breech baby you have the same choices for pain relief as with a baby who is in the head-first position. If you choose to have an epidural, there is an increased chance of a caesarean section. However, whatever you choose, a calm atmosphere with continuous support should be provided.
If you have a vaginal breech birth, your baby’s heart rate will usually be monitored continuously as this has been shown to improve your baby’s chance of a good outcome.
In some circumstances, for example, if there are concerns about your baby’s heart rate or if your labour is not progressing, you may need an emergency caesarean section during labour. A paediatrician (a doctor who specialises in the care of babies, children and teenagers) will attend the birth to check your baby is doing well.
If you go into labour before 37 weeks of pregnancy, the balance of the benefits and risks of having a caesarean section or vaginal birth changes and will be discussed with you.
If you are having twins and the first baby is breech, your healthcare professional will usually recommend a planned caesarean section.
If, however, the first baby is head-first, the position of the second baby is less important. This is because, after the birth of the first baby, the second baby has lots more room to move. It may turn naturally into a head-first position or a doctor may be able to help the baby to turn. See the RCOG patient information Multiple pregnancy: having more than one baby .
If you would like further information on breech babies and breech birth, you should speak with your healthcare professional.
Further information
- NHS information on breech babies
- NCT information on breech babies
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions , if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
- https://aqua.nhs.uk/resources/shared-decision-making-case-studies/
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Clinical Guidelines No. 20a External Cephalic Version and Reducing Incidence of Term Breech Presentation and No. 20b Management of Breech Presentation . The guidelines contain a full list of the sources of evidence we have used.
This information was reviewed before publication by women attending clinics in Nottingham, Essex, Inverness, Manchester, London, Sussex, Bristol, Basildon and Oxford, by the RCOG Women’s Network and by the RCOG Women’s Voices Involvement Panel.
Please give us feedback by completing our feedback survey:
- Members of the public – patient information feedback
- Healthcare professionals – patient information feedback
External Cephalic Version and Reducing the Incidence of Term Breech Presentation Green-top Guideline
Management of Breech Presentation Green-top Guideline
What happens if your baby is breech?
Babies often twist and turn during pregnancy, but most will have moved into the head-down (also known as head-first) position by the time labour begins. However, that does not always happen, and a baby may be:
- bottom first or feet first (breech position)
- lying sideways (transverse position)
Bottom first or feet first (breech baby)
If your baby is lying bottom or feet first, they are in the breech position. If they're still breech at around 36 weeks' gestation, the obstetrician and midwife will discuss your options for a safe delivery.
Turning a breech baby
If your baby is in a breech position at 36 weeks, you'll usually be offered an external cephalic version (ECV). This is when a healthcare professional, such as an obstetrician, tries to turn the baby into a head-down position by applying pressure on your abdomen. It's a safe procedure, although it can be a bit uncomfortable.
Giving birth to a breech baby
If an ECV does not work, you'll need to discuss your options for a vaginal birth or caesarean section with your midwife and obstetrician.
If you plan a caesarean and then go into labour before the operation, your obstetrician will assess whether it's safe to proceed with the caesarean delivery. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
The Royal College of Obstetricians and Gynaecologists (RCOG) website has more information on what to expect if your baby is still breech at the end of pregnancy .
The RCOG advises against a vaginal breech delivery if:
- your baby's feet are below its bottom – known as a "footling breech"
- your baby is larger or smaller than average – your healthcare team will discuss this with you
- your baby is in a certain position – for example, their neck is very tilted back, which can make delivery of the head more difficult
- you have a low-lying placenta (placenta praevia)
- you have pre-eclampsia
Lying sideways (transverse baby)
If your baby is lying sideways across the womb, they are in the transverse position. Although many babies lie sideways early on in pregnancy, most turn themselves into the head-down position by the final trimester.
Giving birth to a transverse baby
Depending on how many weeks pregnant you are when your baby is in a transverse position, you may be admitted to hospital. This is because of the very small risk of the umbilical cord coming out of your womb before your baby is born (cord prolapse). If this happens, it's a medical emergency and the baby must be delivered very quickly.
Sometimes, it's possible to manually turn the baby to a head-down position, and you may be offered this.
But, if your baby is still in the transverse position when you approach your due date or by the time labour begins, you'll most likely be advised to have a caesarean section.
Video: My baby is breech. What help will I get?
In this video, a midwife describes what a breech position is and what can be done if your baby is breech.
Page last reviewed: 1 November 2023 Next review due: 1 November 2026
Breech presentation
Highlights & basics.
- Diagnostic Approach
- Risk Factors
History & Exam
- Differential Diagnosis
- Tx Approach
- Emerging Tx
- Complications
PATIENT RESOURCES
- Patient Instructions
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Quick Reference
Key Factors
Other Factors
Diagnostics Tests
Treatment Options
Epidemiology
Pathophysiology.

Key Articles
Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. Mar 2017 [internet publication]. [Full Text]
Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
Referenced Articles
1. Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997.
2. Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002.
3. Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol. 1976 May 15;125(2):269-70. [Abstract]
4. Nassar N, Roberts CL, Cameron CA, et al. Diagnostic accuracy of clinical examination for detection of non-cephalic presentation in late pregnancy: cross sectional analytic study. BMJ. 2006 Sep 16;333(7568):578-80. [Abstract] [Full Text]
5. Roberts CL, Peat B, Algert CS, et al. Term breech birth in New South Wales, 1990-1997. Aust N Z J Obstet Gynaecol. 2000 Feb;40(1):23-9. [Abstract]
6. Roberts CL, Algert CS, Peat B, et al. Small fetal size: a risk factor for breech birth at term. Int J Gynaecol Obstet. 1999 Oct;67(1):1-8. [Abstract]
7. Brar HS, Platt LD, DeVore GR, et al. Fetal umbilical velocimetry for the surveillance of pregnancies complicated by placenta previa. J Reprod Med. 1988 Sep;33(9):741-4. [Abstract]
8. Kian L. The role of the placental site in the aetiology of breech presentation. J Obstet Gynaecol Br Commonw. 1963 Oct;70:795-7. [Abstract]
9. Rayl J, Gibson PJ, Hickok DE. A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol. 1996 Jan;174(1 Pt 1):28-32. [Abstract]
10. Westgren M, Edvall H, Nordstrom L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985 Jan;92(1):19-22. [Abstract]
11. Brenner WE, Bruce RD, Hendricks CH. The characteristics and perils of breech presentation. Am J Obstet Gynecol. 1974 Mar 1;118(5):700-12. [Abstract]
12. Hall JE, Kohl S. Breech presentation. Am J Obstet Gynecol. 1956 Nov;72(5):977-90. [Abstract]
13. Morgan HS, Kane SH. An analysis of 16,327 breech births. JAMA. 1964 Jan 25;187:262-4. [Abstract]
14. Luterkort M, Persson P, Weldner B. Maternal and fetal factors in breech presentation. Obstet Gynecol. 1984 Jul;64(1):55-9. [Abstract]
15. Braun FH, Jones KL, Smith DW. Breech presentation as an indicator of fetal abnormality. J Pediatr. 1975 Mar;86(3):419-21. [Abstract]
16. Albrechtsen S, Rasmussen S, Dalaker K, et al. Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence. Obstet Gynecol. 1998 Sep;92(3):345-50. [Abstract]
17. Zlopasa G, Skrablin S, Kalafatić D, et al. Uterine anomalies and pregnancy outcome following resectoscope metroplasty. Int J Gynaecol Obstet. 2007 Aug;98(2):129-33. [Abstract]
18. Acién P. Breech presentation in Spain, 1992: a collaborative study. Eur J Obstet Gynecol Reprod Biol. 1995 Sep;62(1):19-24. [Abstract]
19. Michalas SP. Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases. Int J Gynaecol Obstet. 1991 Jul;35(3):215-9. [Abstract]
20. Fianu S, Vaclavinkova V. The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand. 1978;57(4):371-2. [Abstract]
21. Haruyama Y. Placental implantation as the cause of breech presentation [in Japanese]. Nihon Sanka Fujinka Gakkai Zasshi. 1987 Jan;39(1):92-8. [Abstract]
22. Filipov E, Borisov I, Kolarov G. Placental location and its influence on the position of the fetus in the uterus [in Bulgarian]. Akush Ginekol (Sofiia). 2000;40(4):11-2. [Abstract]
23. Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001 May 5;322(7294):1089-93. [Abstract] [Full Text]
24. Beischer NA, Mackay EV, Colditz P, eds. Obstetrics and the newborn: an illustrated textbook. 3rd ed. London: W.B. Saunders; 1997.
25. Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
26. Royal College of Obstetricians and Gynaecologists. Antepartum haemorrhage: green-top guideline no. 63. November 2011 [internet publication]. [Full Text]
27. American College of Obstetricians and Gynecologists. Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-56. [Abstract]
28. Enkin M, Keirse MJNC, Neilson J, et al. Guide to effective care in pregnancy and childbirth. 3rd ed. Oxford: Oxford University Press; 2000.
29. Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000083. [Abstract] [Full Text]
30. Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
31. Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. Mar 2017 [internet publication]. [Full Text]
32. Rosman AN, Guijt A, Vlemmix F, et al. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [Abstract]
33. American College of Obstetricians and Gynecologists. Practice bulletin no. 221: external cephalic version. May 2020 [internet publication]. [Full Text]
34. Bogner G, Xu F, Simbrunner C, et al. Single-institute experience, management, success rate, and outcome after external cephalic version at term. Int J Gynaecol Obstet. 2012 Feb;116(2):134-7. [Abstract]
35. Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983 May;90(5):392-9. [Abstract]
36. Beuckens A, Rijnders M, Verburgt-Doeleman GH, et al. An observational study of the success and complications of 2546 external cephalic versions in low-risk pregnant women performed by trained midwives. BJOG. 2016 Feb;123(3):415-23. [Abstract]
37. Nassar N, Roberts CL, Barratt A, et al. Systematic review of adverse outcomes of external cephalic version and persisting breech presentation at term. Paediatr Perinat Epidemiol. 2006 Mar;20(2):163-71. [Abstract]
38. Sela HY, Fiegenberg T, Ben-Meir A, et al. Safety and efficacy of external cephalic version for women with a previous cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2009 Feb;142(2):111-4. [Abstract]
39. Pichon M, Guittier MJ, Irion O, et al. External cephalic version in case of persisting breech presentation at term: motivations and women's experience of the intervention [in French]. Gynecol Obstet Fertil. 2013 Jul-Aug;41(7-8):427-32. [Abstract]
40. Nassar N, Roberts CL, Raynes-Greenow CH, et al. Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG. 2007 Mar;114(3):325-33. [Abstract] [Full Text]
41. Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
42. US Food & Drug Administration. FDA Drug Safety Communication: new warnings against use of terbutaline to treat preterm labor. Feb 2011 [internet publication]. [Full Text]
43. European Medicines Agency. Restrictions on use of short-acting beta-agonists in obstetric indications - CMDh endorses PRAC recommendations. October 2013 [internet publication]. [Full Text]
44. Magro-Malosso ER, Saccone G, Di Tommaso M, et al. Neuraxial analgesia to increase the success rate of external cephalic version: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2016 Sep;215(3):276-86. [Abstract]
45. de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
46. American College of Obstetricians and Gynecologists. Committee opinion no. 745: mode of term singleton breech delivery. Aug 2018 (reaffirmed 2023) [internet publication]. [Full Text]
47. Berhan Y, Haileamlak A. The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG. 2016 Jan;123(1):49-57. [Abstract] [Full Text]
48. Lydon-Rochelle M, Holt VL, Martin DP, et al. Association between method of delivery and maternal rehospitalisation. JAMA. 2000 May 10;283(18):2411-6. [Abstract]
49. Yokoe DS, Christiansen CL, Johnson R, et al. Epidemiology of and surveillance for postpartum infections. Emerg Infect Dis. 2001 Sep-Oct;7(5):837-41. [Abstract]
50. van Ham MA, van Dongen PW, Mulder J. Maternal consequences of caesarean section. A retrospective study of intra-operative and postoperative maternal complications of caesarean section during a 10-year period. Eur J Obstet Gynecol Reprod Biol. 1997 Jul;74(1):1-6. [Abstract]
51. Murphy DJ, Liebling RE, Verity L, et al. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001 Oct 13;358(9289):1203-7. [Abstract]
52. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001 Jul;15(3):232-40. [Abstract]
53. Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. Br J Obstet Gynaecol. 1996 Feb;103(2):154-61. [Abstract]
54. Persson J, Wolner-Hanssen P, Rydhstroem H. Obstetric risk factors for stress urinary incontinence: a population-based study. Obstet Gynecol. 2000 Sep;96(3):440-5. [Abstract]
55. MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000 Dec;107(12):1460-70. [Abstract]
56. Thompson JF, Roberts CL, Currie M, et al. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002 Jun;29(2):83-94. [Abstract]
57. Australian Institute of Health and Welfare. Australia's mothers and babies 2015 - in brief. October 2017 [internet publication]. [Full Text]
58. Mutryn CS. Psychosocial impact of cesarean section on the family: a literature review. Soc Sci Med. 1993 Nov;37(10):1271-81. [Abstract]
59. DiMatteo MR, Morton SC, Lepper HS, et al. Cesarean childbirth and psychosocial outcomes: a meta-analysis. Health Psychol. 1996 Jul;15(4):303-14. [Abstract]
60. Greene R, Gardeit F, Turner MJ. Long-term implications of cesarean section. Am J Obstet Gynecol. 1997 Jan;176(1 Pt 1):254-5. [Abstract]
61. Coughlan C, Kearney R, Turner MJ. What are the implications for the next delivery in primigravidae who have an elective caesarean section for breech presentation? BJOG. 2002 Jun;109(6):624-6. [Abstract]
62. Hemminki E, Merilainen J. Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol. 1996 May;174(5):1569-74. [Abstract]
63. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002 Jun;99(6):976-80. [Abstract]
64. Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995 Feb;102(2):101-6. [Abstract]
65. Annibale DJ, Hulsey TC, Wagner CL, et al. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995 Aug;149(8):862-7. [Abstract]
66. Hook B, Kiwi R, Amini SB, et al. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics. 1997 Sep;100(3 Pt 1):348-53. [Abstract]
67. Stock SJ, Thomson AJ, Papworth S, et al. Antenatal corticosteroids to reduce neonatal morbidity and mortality: Green-top Guideline No. 74. BJOG. 2022 Jul;129(8):e35-60. [Abstract] [Full Text]
68. American College of Obstetricians and Gynaecologists. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. Aug 2017 (reaffirmed 2024) [internet publication]. [Full Text]
69. Nassar N, Roberts CL, Cameron CA, et al. Outcomes of external cephalic version and breech presentation at term: an audit of deliveries at a Sydney tertiary obstetric hospital, 1997-2004. Acta Obstet Gynecol Scand. 2006;85(10):1231-8. [Abstract]
70. Nwosu EC, Walkinshaw S, Chia P, et al. Undiagnosed breech. Br J Obstet Gynaecol. 1993 Jun;100(6):531-5. [Abstract]
71. Flamm BL, Ruffini RM. Undetected breech presentation: impact on external version and cesarean rates. Am J Perinatol. 1998 May;15(5):287-9. [Abstract]
72. Cockburn J, Foong C, Cockburn P. Undiagnosed breech. Br J Obstet Gynaecol. 1994 Jul;101(7):648-9. [Abstract]
73. Leung WC, Pun TC, Wong WM. Undiagnosed breech revisited. Br J Obstet Gynaecol. 1999 Jul;106(7):638-41. [Abstract]
74. Wilcox C, Nassar N, Roberts C. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG. 2011 Mar;118(4):423-8. [Abstract]
75. Qureshi H, Massey E, Kirwan D, et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med. 2014 Feb;24(1):8-20. [Abstract] [Full Text]
76. Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015 Jul 29;(7):CD000084. [Abstract] [Full Text]
77. Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012 May 16;(5):CD003928. [Abstract] [Full Text]
78. Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000051. [Abstract] [Full Text]
79. National Institute for Health and Care Excellence. Caesarean birth. Jan 2024 [internet publication]. [Full Text]
80. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):917-27. [Abstract]
81. Eide MG, Oyen N, Skjaerven R, et al. Breech delivery and Intelligence: a population-based study of 8,738 breech infants. Obstet Gynecol. 2005 Jan;105(1):4-11. [Abstract]
82. Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):864-71. [Abstract]
83. Brown S, Lumley J. Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998 Feb;105(2):156-61. [Abstract]
Sign in to access our clinical decision support tools
- Introduction
- Conclusions
- Article Information
UC-pH indicates umbilical cord pH.
eTable 1 . ICD-10 Codes
eTable 2. Comparison of Primary and Secondary Outcomes Between Umbilical Cord pH Groups, 0 to 7 Days After Birth
eTable 3. Comparison of Primary and Secondary Outcomes Between UC-pH Groups, Unadjusted Results
eTable 4. Comparison of Primary and Secondary Outcomes Between Umbilical Cord pH Groups in Cohort With 2 Umbilical Cord pH Measurements
eTable 5. Baseline Descriptive Characteristics According to Umbilical Cord pH Levels, Including Missing Umbilical Cord pH Measurements
eTable 6. Comparison of Primary and Secondary Outcomes Among Infants With Missing Umbilical Cord pH Measurements and Reference Group
eTable 7. Comparison of Primary and Secondary Outcomes Between Umbilical Cord pH Groups With Imputation for Missing Values of Umbilical Cord pH
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Andersson CB , Klingenberg C , Thellesen L , Johnsen SP , Kesmodel US , Petersen JP. Umbilical Cord pH Levels and Neonatal Morbidity and Mortality. JAMA Netw Open. 2024;7(8):e2427604. doi:10.1001/jamanetworkopen.2024.27604
Manage citations:
© 2024
- Permissions
Umbilical Cord pH Levels and Neonatal Morbidity and Mortality
- 1 Danish Center for Health Services Research, Department of Clinical Medicine, Aalborg University, Aalborg, Denmark
- 2 Department of Obstetrics and Gynaecology, Aalborg University Hospital, Thisted, Denmark
- 3 Department of Paediatrics, University Hospital of North Norway, Tromsø
- 4 Research Group for Child and Adolescent Health, Department of Clinical Medicine, The Arctic University of Norway, Tromsø
- 5 Department of Obstetrics and Gynaecology, Herlev Hospital, University of Copenhagen, Herlev, Denmark
- 6 Department of Obstetrics and Gynaecology, Aalborg University Hospital, Aalborg, Denmark
- 7 Department of Clinical Medicine, Aalborg University, Aalborg, Denmark
- 8 Department of Paediatrics, Aarhus University Hospital, Aarhus, Denmark
Question What is the umbilical cord (UC) pH threshold for increased morbidity and mortality among full-term infants in a national unselected population?
Findings In this national cohort study of 340 431 liveborn, singleton, full-term infants without malformations, lower UC-pH levels were associated with the risk of adverse neonatal outcomes, even at levels not previously associated with increased morbidity and mortality. This association was observed for serious and less severe outcomes, including the need for respiratory support during the transition to extrauterine life and hypoglycemia.
Meaning These findings suggest that the UC-pH threshold for more intensive observation and treatment, in case of acidosis, may be reconsidered.
Importance Umbilical cord pH (UC-pH) level is an important objective indicator of intrapartum fetal hypoxia and is used to predict neonatal morbidity and mortality. A UC-pH value of less than 7.00 is often defined as a threshold for severe acidosis, but existing evidence is divergent and largely based on UC-pH measurements from selected populations; consequently, the results are challenging to interpret.
Objective To investigate the association between UC-pH levels and the risk of adverse neonatal outcomes in a national setting with universal UC-pH measurement.
Design, Setting, and Participants This national, population-based cohort study included all liveborn, singleton, full-term infants without malformations born in Denmark from January 1, 2012, to December 31, 2018. Data were analyzed from January 1, 2023, to March 1, 2024.
Exposure Umbilical cord pH level categorized as less than 7.00, 7.00 to 7.09, 7.10 to 7.19 and 7.20 to 7.50 (reference group).
Main Outcomes and Measures The primary outcome was a composite of severe adverse neonatal outcomes: neonatal death, therapeutic hypothermia, mechanical ventilation, treatment with inhaled nitric oxide, or seizures. Secondary outcomes were individual components of the primary outcome, Apgar score, respiratory outcomes, and hypoglycemia. Data are presented as adjusted risk ratios (ARRs) with 95% CIs.
Results Among the 340 431 infants included, mean (SD) gestational age was 39.9 (1.6) weeks; mean (SD) birth weight was 3561 (480) g; and 51.3% were male. Umbilical cord pH of less than 7.20 was observed more often among infants with a gestational age of 40 or 41 weeks (31.6%-33.6% compared with 18.2%-20.2% at a gestational age of 39 weeks) and among male infants (53.9%-55.4% vs 44.6%-46.1% among female infants). Compared with the pH reference group (576 of 253 540 [0.2%]), the risk for the primary outcome was increased for the groups with UC-pH levels of less than 7.00 (171 of 1743 [9.8%]), 7.00 to 7.09 (101 of 11 904 [0.8%]), and 7.10 to 7.19 (259 of 73 244 [0.4%]). Comparable patterns were observed for the individual outcomes, except for neonatal death, which was only increased in the group with UC-pH levels of less than 7.10. The risk of treatment with continuous positive airway pressure was increased when UC-pH levels were less than 7.20, and the risk of hypoglycemia was 21.5% if UC-pH levels were less than 7.10.
Conclusions and Relevance In this cohort study of 340 431 newborn infants, results support and extend previous studies indicating a higher risk of adverse outcomes even at UC-pH levels above 7.00. The threshold for more intensive observation and treatment may be reconsidered.
Umbilical cord blood pH (UC-pH) measurement is used to identify infants exposed to intrapartum hypoxia and acidosis. Severe metabolic acidosis is associated with an increased risk of developing hypoxic-ischemic encephalopathy (HIE), potentially leading to lifelong disabilities or death. 1 , 2 Additionally, severe intrapartum hypoxia can result in multiorgan injury, affecting the heart, lungs, and kidneys. 3 Immediate recognition of severe acidosis after birth is essential for closer observation and timely intervention, and in case of HIE, to provide therapeutic hypothermia aimed at preventing the second phase of brain injury that occurs 6 to 15 hours after birth. 4 - 6
There is no global consensus on a specific UC-pH threshold value associated with increased morbidity and mortality risk. A UC-pH level of less than 7.00 is often defined as severe acidosis, and this threshold is also widely used as one of the criteria for therapeutic hypothermia. 4 - 6 Some authors argue that a higher UC-pH threshold improves detection of infants with moderate to severe HIE who may benefit from therapeutic hypothermia, and many centers today already screen for HIE and offer therapeutic hypothermia to infants with UC-pH values above 7.00 if other criteria are fulfilled, but evidence of benefit is limited. 7 - 10 For respiratory adverse outcomes, previous studies 11 , 12 have shown that need for respiratory support to assist transition to extrauterine life is increased at values above 7.00. In 2022, Bligard et al 11 investigated adverse neonatal outcomes among 2081 infants born from planned cesarean section with regional anesthesia and found an almost 3-fold increased risk of respiratory distress among infants with UC-pH levels of less than 7.20 compared with infants with UC-pH levels of 7.20 or greater.
Most previous studies are based on populations in settings with a policy of selective measurement of UC-pH levels, reserved for high-risk deliveries or deliveries in which the fetus shows sign of hypoxia during birth. Since 2009, the policy in Denmark has been universal measuring of UC-pH levels, and in 2014 the proportion of infants with at least 1 UC-pH measurement was 95.6%. The implementation of universal UC-pH measurement has increased the proportion of samples in both vigorous and nonvigorous infants and in acute obstetric situations. 13 In this population-based cohort study, we investigated the association between UC-pH values and the risk of adverse neonatal outcomes in a setting with universal UC-pH measurement.
Permission to access data used for the study was granted by the Danish Data Protection Agency. In Denmark, ethical permissions and informed consent are not required for register-based studies. The study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
In this population-based cohort study, data were obtained from the Danish Civil Registration System, which holds information on residence and vital status, and the Danish National Patient Register. The Danish National Patient Register contains data on all pregnant women, deliveries, and newborn infants in Denmark, including obstetric characteristics, complications, UC-pH levels, diagnoses ( International Statistical Classification of Diseases, Tenth Revision ) and medical procedural codes. 14 , 15 The unique 10-digit civil registration number, assigned to all inhabitants of Denmark at birth or entry into the country, allows unambiguous individual-level identification and data linkage across nationwide registers, including linkage between mother and infant.
In Denmark, measurement of UC-pH levels is recommended from blood samples collected within the first minute after birth in case the cord is not clamped, and within 30 minutes after birth if from a clamped segment of the cord. It is recommended that the blood gas levels be analyzed within 30 minutes from birth. 16 Late cord clamping was recommended in Denmark from 2017 and was not common practice during the study period.
This study was based on a secondary data analysis of all liveborn, singleton, full-term infants (gestational age ≥37 weeks) born in Denmark from January 1, 2012, through December 31, 2018. Infants with congenital malformations of the heart, lungs, or nervous system were excluded. Furthermore, we excluded infants with UC-pH levels of less than 6.50 and greater than 7.50, as these pH values were considered registration errors ( Figure ). 17
We included all infants with at least 1 UC-pH measurement. Infants were categorized into groups according to UC-pH levels of less than 7.00, 7.00 to 7.09, 7.10 to 7.19, and 7.20 to 7.50 (reference group). The reference group was chosen since this interval contains the top of the normal reference curve. 10 , 17
We obtained data on gestational age, sex assigned at birth, birth weight, maternal smoking in pregnancy, types 1 and 2 diabetes, gestational diabetes, hypertension, preeclampsia, other medical diseases (respiratory diseases, hypothyroidism, hyperthyroidism, polycystic ovary syndrome, gastrointestinal diseases, and neurological disease), placental insufficiency (pathological signs on the cardiotocography, intrauterine growth restriction [<−2 SD], low amniotic fluid volume, or abnormal ultrasonographic Doppler indices of fetal vessels), intrapartum fever, serious birth events (shoulder dystocia, uterine rupture, placental abruption, cord prolapse, or vasa praevia), breech presentation, instrumental delivery, and emergency cesarean section ( Table 1 ). We did not report data on race and ethnicity since we did not find it relevant in this context. Gestational age was set in 99.2% of pregnancies during an ultrasonographic examination early or late in the second trimester. 18 Diagnoses and procedures included in this study are presented in eTable 1 in Supplement 1 ).
The outcomes of interest were neonatal morbidity and mortality, occurring within the first 28 days after birth. The primary outcome was defined as a composite of severe adverse neonatal outcomes encompassing neonatal death, therapeutic hypothermia, mechanical ventilation, treatment with inhaled nitric oxide, or seizures. Secondary outcomes were individual components of the primary outcome and specific clinical outcomes, including 5-minute Apgar scores below 4 and 7, treatment with continuous positive airway pressure, meconium aspiration syndrome, and hypoglycemia.
Data were analyzed from January 1, 2023, to March 1, 2024. Results in the main analysis were adjusted for factors known from the literature to affect the association between hypoxia and adverse neonatal outcomes: infant sex assigned at birth; gestational age (37, 38, 39, 40, 41, and ≥42 weeks), year of birth, intrapartum fever, intrauterine growth restriction, and types 1 and 2 diabetes. 19 - 23 Our results are based on 1 UC-pH value from each included infant, and if 2 values were registered, we used the lowest value.
All outcomes, including the composite outcome, were dichotomous and coded as 0 or 1. We used modified Poisson regression models (Poisson regression with robust error variance) to estimate the difference in adverse outcomes between the groups with UC-pH levels below 7.20 and the reference group with UC-pH levels of 7.20 to 7.50. 24 - 27 The results are reported as risks and adjusted risk ratios (ARR) with 95% CIs. Stata, version 15 (StataCorp LLC) was used for statistical analyses.
We performed 4 sensitivity analyses: one with more restricted composite outcomes, one with a restricted surveillance period of 7 days, one without adjustments, and one only including infants with UC-pH values sampled from both the umbilical artery and vein. Moreover, we analyzed the group with missing UC-pH measurement according to characteristics and outcomes and report on results after multivariate imputation by chained equations for missing UC-pH measurement. 28
Among 362 389 live singleton infants with no malformations in Denmark from 2012 to 2018, at least 1 UC-pH measurement was registered in 340 431 infants (93.9%) ( Figure ). A total of 5.9% of infants were missing UC-pH measurements, which was higher among infants with the primary outcome (109 of 1216 [9.0%]) and with neonatal death (27 of 141 [19.1%]). The mean (SD) gestational age was 39.9 (1.6) weeks, mean (SD) birth weight was 3561 (480) g, 51.3% were male, and 48.7% were female. Comparison groups included 1743 infants (0.5%) with UC-pH levels of less than 7.00, 11 904 (3.5%) with levels of 7.00 to 7.09, and 73 244 (21.5%) with levels of 7.10 to 7.19. Umbilical cord pH levels of less than 7.20 were observed more often among infants with a gestational age of 40 weeks (568 of 1743 [32.6%] for <7.00; 3763 of 11 904 [31.6%] for 7.00-7.09; 24 028 of 73 244 [32.8%] for 7.10-7.19) and among infants with a gestational age 41 weeks (555 of 1743 [31.8%] for <7.00; 4000 of 11 904 [33.6%] for 7.00-7.09; 22 041 of 73 244 [30.1%] for 7.10-7.19) compared with a gestational age of 39 weeks (318 of 1743 [18.2%] for <7.00; 2229 of 11 904 [18.7%] for 7.00-7.09; 14 819 of 73 244 [20.2%] for 7.10-7.19]) and among male infants (966 [55.4%] for <7.00; 6522 of 11 904 [54.8%] for 7.00-7.09; 39 468 of 73 244 [53.9%] for 7.10-7.19) compared with female infants (777 of 1797 [43.2%] for <7.00; 5382 of 11 904 [45.2%] for 7.00-7.09; 33 776 of 73 244 [46.1%] for 7.10-7.19).
Among infants with UC-pH levels of less than 7.00, there was a higher proportion of pregnancies complicated by placental insufficiency, gestational diabetes, hypertensive disorders, and other maternal medical diseases. Moreover, deliveries were more often complicated by serious birth events ( Table 1 ).
In the group with UC-pH levels of less than 7.00, the risk of the primary composite outcome was markedly increased compared with the risk in the reference group (171 of 1743 [9.8%] vs 576 of 253 540 [0.2%]), as was the risk of neonatal death (34 of 1743 [2.0%] vs 55 of 253 540 [0.02%]). Comparable differences were seen for all individual outcomes.
In the group with UC-pH levels of 7.00 to 7.09, the risk of the primary outcome was 101 of 11 904 (0.8%). The risk of most adverse outcomes was markedly lower compared with those with UC-pH levels of less than 7.00, but still significantly higher than in the reference group. The ARR for therapeutic hypothermia was 13.83 (95% CI, 8.43-22.69) in the group with UC-pH levels of 7.00 to 7.09 compared with the reference group. The proportion of infants diagnosed with hypoglycemia was comparable if UC-pH levels were less than 7.00 (274 of 1743 [21.5%]) and 7.00 to 7.09 (2449 of 11 904 [20.6%]).
In the group with UC-pH levels of 7.10 to 7.19, the risk of most adverse neonatal outcomes was lower but still increased (primary outcome, 259 of 73 244 [0.4%]). The ARR for the primary outcome was 1.60 (95% CI, 1.38-1.85) and ARRs were 2.24 (95% CI, 20.1-2.50) for low Apgar scores, 1.97 (95% CI. 1.90-2.05) for continuous positive air pressure, and 1.76 (95% CI, 1.70-1.82) for hypoglycemia when compared with infants with UC-pH levels of 7.20 to 7.50. However, the risk of neonatal death was not increased. Overall, 1976 of 11 904 infants (16.6%) with UC-pH levels of 7.00 to 7.09 and 4286 of 73 244 (5.9%) with UC-pH levels of 7.10 to 7.19 received noninvasive respiratory support to assist transition to extrauterine life (ARRs, 5.55 [95% CI 5.30-5.82] and 1.97 [95% CI 1.90-2.05], respectively) ( Table 2 ).
In the sensitivity analyses, we found that restricting the composite outcome to exclude therapeutic hypothermia resulted in a reduced risk in the group with UC-pH levels of less than 7.00 ( Table 3 ). Results from the analysis with a 7-day study period and the unadjusted results were not markedly different from the main results (eTables 2 and 3 in Supplement 1 ). When only including cases with UC-pH levels measured from both the umbilical cord artery and vein, we found a lower risk of adverse outcomes in the group with UC-pH levels of less than 7.00, but nearly the same risk in the groups with UC-pH levels of 7.00 to 7.09 and 7.10 to 7.19 (eTable 4 in Supplement 1 ).
In the group with missing UC-pH measurements (31 285 of 362 389 [5.9%] of the study population), we found similar characteristics as in the groups with UC-pH levels of greater than 7.10 and similar risk of adverse outcomes as in the group with UC-pH levels of 7.10 to 7.19, except for the risk of neonatal death, which equaled that of the group with UC-pH levels of 7.00 to 7.09 (eTables 5 and 6 in Supplement 1 ). Multiple imputation for missing UC-pH measurement did not change the overall results (eTable 7 in Supplement 1 ).
In this nationwide cohort study, we investigated the risk of neonatal morbidity and mortality in infants with low UC-pH levels and found that neonates with lower UC-pH values had substantially increased risk of adverse neonatal outcomes. This was seen in the group with UC-pH levels of less than 7.00 but also in the group with UC-pH levels of 7.00 to 7.09 and, to a lesser extent, in the group with UC-pH levels of 7.10 to 7.19. Our findings indicate an association between UC-pH levels and the risk of neonatal morbidity and mortality, even at levels not previously clearly related to adverse neonatal outcomes.
Our results correlate well with those of previous studies indicating that the risk of an adverse outcome is increased at UC-pH levels above 7.00. Our results showed that the ARR for therapeutic hypothermia was 13.83 (95% CI, 8.43-22.69) in the group with UC-pH levels of 7.00 to 7.09 despite the pH threshold at 7.00 recommended in the Danish guidelines ( Table 2 ). 29 This supports previous findings suggesting a higher pH threshold for screening for HIE and using therapeutic hypothermia if other criteria are fulfilled. 7 - 10 In line with Bligard et al, 11 who found a tripled risk of respiratory distress if UC-pH value was less than 7.20, we found that the ARR for continuous positive airway pressure to support transition to extrauterine life was 5.55 (95% CI, 5.30-5.82) in the group with UC-pH of 7.00 to 7.09 and 1.97 (95% CI, 1.90-2.05) in the group with UC-pH levels of 7.10 to 7.19.
It is known from previous studies 30 - 32 that there is an association among acidosis, hypoglycemia and adverse neurological outcomes. However, we have not found prior studies indicating similar marked (5-fold) increased risk of hypoglycemia in infants with UC-pH levels of below 7.10.
The correlation between fetal acidosis and adverse neonatal outcome is complex and not well understood. Adverse neonatal outcomes can be caused by intrapartum acidosis alone or by known or unknown antenatal conditions such as maternal medical diseases, late gestational age, placental insufficiency, infections, fetal anemia, acute obstetric situations such as placental abruption, or a combination of acidosis and 1 or more of these factors. 19 - 23 , 33 , 34 This means that in individual cases, differentiating whether neonatal encephalopathy is primarily caused by hypoxia (eg, HIE), inherent or acquired child frailty, birth-related factors, or a combination thereof, can be challenging or even impossible. 34 - 36 The complexity implies difficulty in establishing a model linking umbilical cord acidemia with a risk of neonatal morbidity and mortality without introducing bias. In our main analysis, we adjusted for factors known from the literature to affect the risks of hypoxia and adverse neonatal outcomes.
Most previous studies 9 - 12 restricted the inclusion criteria to infants with UC-pH measured from both the umbilical cord artery and vein. This criterion ensures that the pH level from the umbilical artery, which defines acidosis, is known. However, previous studies 13 have shown that the registration of only 1 UC-pH measurement is higher in cases with increased risk of complications (eg, fetal growth retardation), and excluding these infants may therefore underestimate the risk of complications. In the present study we expanded the inclusion criteria to infants with at least 1 UC-pH measurement. When including infants with 1 UC-pH measurement (or 2 measurements with a pH difference <0.02, suggesting sampling from the same vessel), part of our results were expectedly based on UC-pH measurement from the umbilical vein. Samples obtained from the umbilical vein have a higher pH level, and this might cause selective misclassification in the UC-pH groups. Therefore, the group with UC-pH levels of less than 7.00 is potentially slightly underestimated, and some of the infants in the group with UC-pH levels of 7.00 to 7.09 will expectedly include infants with an arterial pH level below 7.00. To compare our results with those from previous studies, we performed a sensitivity analysis in which only infants with UC-pH levels sampled from both the umbilical artery and vein were included. This analysis showed a lower risk of adverse outcomes in the group with UC-pH levels of less than 7.00, but the risk of adverse outcomes in the groups with UC-pH levels of 7.00 to 7.09 and 7.10 to 7.19 were the same. This corresponds well with a previous study showing that in very acute situations with expected higher risk of adverse outcomes, the proportion with only 1 UC-pH measurement was higher. 13 Despite the risk of misclassification, it is valuable to include infants with only 1 UC-pH measurement to include the most serious cases.
The strength of our study lies in the national population-based material that makes it possible to study the risk of adverse neonatal outcome according to UC-pH levels while avoiding selection bias from a selective approach only measuring UC-pH levels in infants suspected of having or with an increased risk of hypoxia and neonatal complications. The large sample size allowed us to include rare events such as therapeutic hypothermia and neonatal death. The national implementation of universal UC-pH measurement means that the cohort included deliveries and infants from all parts of the country and from both small maternity wards and large university hospitals. This is unique compared with previous studies, 9 , 10 , 12 , 33 which are from single hospitals or administrative regions. The comprehensive registration of characteristics, interventions, and complications during birth enabled us to compare the 4 UC-pH level groups and the group with missing UC-pH measurement according to risk factors for acidosis and complications.
This study also has some limitations. Our study did not contain all elements of the cord blood gas analyses, since only UC-pH measurements are included in the central registers in Denmark. Not having access to P co 2 , base excess, and lactate values means that we were not able to distinguish between metabolic and respiratory acidosis. However, previous studies 7 , 37 , 38 have shown that the arterial UC-pH measurement had a markedly better sensitivity to detect moderate to severe HIE compared with umbilical cord base excess, and UC-pH levels in general are recognized as a good parameter of adverse neonatal outcomes.
The proportion of infants with missing UC-pH values within the composite outcome was 109 of 1216 (9.0%) and within neonatal death was 27 of 141 (19.1%), which is in contrast to 5.9% missing UC-pH values in the overall population. This could have resulted in an underestimation of the risk of adverse outcomes in the groups with low UC-pH levels. However, when testing with multiple imputations for missing values, we found that effect estimates were largely unchanged.
Another limitation is that the validity of the study depends on registrations of diagnoses and procedures by clinicians, which will never be flawless in everyday clinical life. In general, registrations of treatments and interventions are more valid than diagnoses. 39 We found no indications of differences in registration between different UC-pH groups.
The primary composite outcome was, in addition to neonatal death, based on procedures used in the treatment of severe acidemia or respiratory diseases. We acknowledge that including therapeutic hypothermia in the composite primary outcome affects the results, since UC-pH levels of less than 7.00 constitute one of the criteria for this treatment in Danish guidelines. This was also seen from the sensitivity analysis with restricted composite outcome ( Table 3 ).
Our study was conducted in a high-income country where more than 95% of deliveries take place in a hospital and where there is good access to ultrasonographic examinations for due dates and screening for malformations as well as obstetric and neonatal care. This may limit the generalizability of the results if compared with other settings. The risk of adverse neonatal outcomes associated with acidosis is presumably higher in settings with less access to obstetric and neonatal care.
This comprehensive cohort study with universal UC-pH measurement indicates that a UC-pH level below 7.20 is associated with a higher risk of infant mortality and morbidities. Even UC-pH levels of 7.10 to 7.19 were linked to an increased risk of severe neonatal morbidities, and neonatal morbidity increased further when UC-pH levels were below 7.10. Furthermore, the results indicated that UC-pH levels of 7.00 to 7.10 were associated with a 5-fold increased need for respiratory support and risk of hypoglycemia. Although we could not differentiate between the specific adverse effects of hypoxia from birth and other causes of neonatal complications or interventions, recognizing the risks associated with low UC-pH levels remains important. Knowing the risk of neonatal adverse outcomes at different levels of UC-pH may lead to reconsidering the threshold for more intensive observation of infants to identify clinical conditions in which intervention is needed. Future studies are needed, especially concerning the risk of adverse outcomes later in childhood.
Accepted for Publication: June 17, 2024.
Published: August 14, 2024. doi:10.1001/jamanetworkopen.2024.27604
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Andersson CB et al. JAMA Network Open .
Corresponding Author: Charlotte Brix Andersson, MD, Danish Center for Health Services Research, Department of Clinical Medicine, Aalborg University, Selma Lagerløfs Vej 249, 9260 Gistrup, Denmark ( [email protected] ).
Author Contributions: Dr Andersson had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Andersson, Thellesen, Johnsen, Kesmodel, Petersen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Andersson, Klingenberg, Petersen.
Critical review of the manuscript for important intellectual content: Thellesen, Johnsen, Kesmodel, Petersen.
Statistical analysis: Andersson.
Obtained funding: Andersson.
Administrative, technical, or material support: Johnsen.
Supervision: Klingenberg, Thellesen, Johnsen, Kesmodel, Petersen.
Conflict of Interest Disclosures: Prof Klingenberg reported honoraria from Chiesi Farmaceutici SpA as a member of the board for the Nordic Neonatal Meeting outside the submitted work. No other disclosures were reported.
Funding/Support: This study was supported by the Elsass Foundation, Denmark, the Dagmar Marshalls Foundation, and the Carsten Lenstrups Foundation.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: Jan Brink Valentin, MSc, Danish Center for health Services Research, Department of Clinical Medicine, Aalborg University, provided statistical support, for which he was not compensated.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

Breech Births and Autism: Exploring the Potential Link
Upside-down and unexpected, a baby’s bottom-first entry into the world might just be the first clue in unraveling the complex puzzle of autism spectrum disorder. This intriguing possibility has sparked a growing interest among researchers and healthcare professionals alike, as they seek to understand the potential connections between birth complications and neurodevelopmental outcomes. As we delve into the intricate relationship between breech births and autism, we’ll explore the latest research, examine the evidence, and consider the implications for parents and healthcare providers.
Understanding Breech Births
Breech presentation occurs when a baby is positioned to be born buttocks or feet first, rather than the typical head-first position. This unique positioning can present challenges during delivery and has been associated with various complications. There are three main types of breech presentations:
1. Frank breech: The baby’s buttocks are aimed at the birth canal with the legs sticking straight up in front of the body and the feet near the head.
2. Complete breech: The baby’s buttocks are down, with the legs folded at the knees and feet near the buttocks.
3. Footling breech: One or both of the baby’s feet are positioned to come out first.
The prevalence of breech births is relatively low, occurring in approximately 3-4% of all pregnancies at term. However, the potential complications associated with breech deliveries can be significant. These may include:
– Umbilical cord prolapse – Head entrapment – Birth injuries – Increased risk of oxygen deprivation
Given these risks, healthcare providers must carefully consider the management and delivery options for breech babies. These options may include:
1. External cephalic version (ECV): A procedure to manually turn the baby to a head-down position before labor begins.
2. Planned cesarean section: Often recommended for breech presentations to reduce the risk of complications.
3. Vaginal breech delivery: In some cases, with experienced practitioners and carefully selected patients, a vaginal breech delivery may be attempted.
The choice of delivery method depends on various factors, including the type of breech presentation, the mother’s health, and the healthcare provider’s expertise. C-Section and Autism: Exploring the Potential Connection and Debunking Myths is a topic that has gained attention in recent years, highlighting the need to consider all aspects of birth interventions and their potential long-term effects.
Autism Spectrum Disorder: An Overview
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental condition characterized by challenges in social interaction, communication, and restricted or repetitive behaviors and interests. The spectrum nature of autism means that individuals can experience a wide range of symptoms and severities, making each case unique.
The prevalence of autism has been steadily increasing over the past few decades. According to the Centers for Disease Control and Prevention (CDC), approximately 1 in 36 children in the United States is diagnosed with ASD. This rise in diagnosis rates has led to increased research efforts to understand the underlying causes and risk factors associated with autism.
While the exact causes of autism remain unknown, researchers have identified several risk factors that may contribute to its development. These include:
1. Genetic factors: Studies have shown that autism has a strong genetic component, with certain gene variations increasing the likelihood of developing ASD.
2. Environmental factors: Exposure to certain environmental toxins, maternal infections during pregnancy, and advanced parental age have been associated with increased autism risk.
3. Prenatal and perinatal complications: Various birth complications, including premature birth, low birth weight, and oxygen deprivation during delivery, have been linked to higher rates of autism.
4. Neurological differences: Brain imaging studies have revealed structural and functional differences in the brains of individuals with autism compared to neurotypical individuals.
The interplay between genetics and environmental factors is complex, and researchers are still working to unravel the intricate web of influences that contribute to autism development. This complexity underscores the importance of considering multiple factors when examining potential links between birth complications and autism risk.
Examining the Potential Link: Are Breech Babies More Likely to Be Autistic?
The question of whether breech babies are more likely to develop autism has been the subject of several studies in recent years. While some research suggests a potential connection, the evidence remains mixed and inconclusive.
A study published in the journal Pediatrics in 2009 found that children born in breech position had a 67% higher risk of autism compared to those born in the typical head-first position. The researchers hypothesized that the increased risk might be due to a combination of factors, including potential oxygen deprivation during delivery and the possibility that the breech position itself could be a marker for underlying neurological differences.
However, it’s important to note that this study, like many others in this field, had limitations. For example, it didn’t account for all potential confounding factors, such as genetic predisposition or other prenatal complications that might influence both breech presentation and autism risk.
Other studies have produced contradictory findings. A large-scale Swedish study published in 2015 found no significant association between breech presentation and autism risk after adjusting for various factors, including gestational age, birth weight, and maternal characteristics.
These conflicting results highlight the complexity of the relationship between birth complications and neurodevelopmental outcomes. It’s crucial to remember that correlation does not imply causation, and the presence of a statistical association doesn’t necessarily mean that breech births directly cause autism.
Birth Complications and Autism Risk
While the specific link between breech births and autism remains unclear, there is a broader body of research examining the relationship between various birth complications and autism risk. The Complex Relationship Between Birth Complications and Autism: Exploring Potential Links and Current Research provides a comprehensive overview of this topic.
Some birth complications that have been associated with increased autism risk include:
1. Premature birth: The Link Between Premature Birth and Autism: Understanding the Risks and Research explores this connection in detail.
2. Low birth weight: Often associated with prematurity, low birth weight has been linked to higher rates of autism.
3. Maternal infections during pregnancy: Certain infections, particularly those that trigger a strong immune response, may increase autism risk.
4. Oxygen deprivation during delivery: Also known as birth asphyxia, this complication has been associated with various neurodevelopmental issues, including autism.
5. Placental complications: Placental Abruption and Autism: Exploring the Potential Connection discusses one such complication and its potential implications.
When comparing breech birth complications to other birth-related risk factors, it’s important to consider the potential mechanisms linking these complications to autism development. One prevailing theory focuses on the role of oxygen deprivation and its impact on brain development.
During a difficult delivery, such as some breech births, there’s an increased risk of oxygen deprivation to the baby’s brain. This can potentially lead to changes in brain structure and function, which may contribute to the development of autism or other neurodevelopmental conditions.
However, it’s crucial to note that many children who experience birth complications, including breech births, do not develop autism. Conversely, many children with autism have no history of significant birth complications. This underscores the complex, multifactorial nature of autism spectrum disorder and the need for continued research to better understand its origins.
Implications for Parents and Healthcare Providers
Given the current state of research on breech births and autism risk, what are the implications for parents and healthcare providers? While it’s important not to overstate the potential connection, there are several considerations to keep in mind:
1. Prenatal care and monitoring: For pregnancies involving breech presentation, healthcare providers should continue to closely monitor fetal development and position. Regular ultrasounds and check-ups can help identify any potential issues early on.
2. Delivery options: The choice between attempting an external cephalic version, planning a cesarean section, or considering a vaginal breech delivery should be made on a case-by-case basis. Healthcare providers should discuss the potential risks and benefits of each option with parents, taking into account the latest research on long-term outcomes.
3. Early intervention and developmental screening: Given the potential for increased risk, parents of breech babies may want to be particularly vigilant about monitoring their child’s developmental milestones. Preemies and Autism: Understanding the Connection Between Premature Birth and Autism Spectrum Disorder discusses the importance of early screening and intervention for at-risk infants.
4. Balancing risks and benefits: When making decisions about breech deliveries, it’s essential to consider both the immediate risks of the delivery itself and the potential long-term implications. Healthcare providers should stay informed about the latest research and guidelines to provide the best possible advice to parents.
5. Addressing parental concerns: Parents who have had a breech delivery may have concerns about their child’s risk of autism or other developmental issues. Healthcare providers should be prepared to address these concerns compassionately and provide evidence-based information and resources.
It’s worth noting that while breech presentation may be associated with a slightly increased risk of autism, it’s just one of many factors that can influence a child’s development. Can Birth Trauma Cause Autism? Exploring the Potential Link Between Perinatal Complications and ASD provides a broader perspective on the relationship between various birth experiences and autism risk.
As we’ve explored the potential link between breech births and autism, it’s clear that the relationship is complex and not fully understood. While some studies suggest a possible association, others have found no significant connection. This inconsistency in the research underscores the need for further investigation into the potential mechanisms linking birth complications to neurodevelopmental outcomes.
For parents and healthcare providers, the current state of knowledge emphasizes the importance of individualized care and decision-making. Each pregnancy and delivery is unique, and the management of breech presentations should be based on a careful consideration of all relevant factors, including the potential long-term implications for the child’s development.
It’s crucial to remember that breech presentation is just one of many factors that may influence a child’s risk of developing autism. Genetic predisposition, environmental exposures, and other prenatal and perinatal factors all play a role in shaping a child’s neurodevelopmental trajectory. The Complex Relationship Between Prematurity and Autism: Exploring the Latest Research provides additional insights into the multifaceted nature of autism risk factors.
Parents who have concerns about their child’s development, regardless of birth history, should feel empowered to discuss these concerns with their healthcare providers. Early identification and intervention can make a significant difference in outcomes for children with autism spectrum disorder.
As research in this field continues to evolve, it’s likely that we’ll gain a clearer understanding of the relationship between breech births, other birth complications, and autism risk. The Complex Relationship Between Traumatic Birth Experiences and Autism: Exploring the Evidence offers further insights into ongoing research in this area. In the meantime, focusing on providing the best possible care during pregnancy, delivery, and early childhood remains the most effective approach to supporting healthy development for all children.
References:
1. American College of Obstetricians and Gynecologists. (2018). Mode of term singleton breech delivery. ACOG Committee Opinion No. 745. Obstetrics & Gynecology, 132(2), e60-e63.
2. Bilder, D., Pinborough-Zimmerman, J., Miller, J., & McMahon, W. (2009). Prenatal, perinatal, and neonatal factors associated with autism spectrum disorders. Pediatrics, 123(5), 1293-1300.
3. Centers for Disease Control and Prevention. (2023). Data & Statistics on Autism Spectrum Disorder. https://www.cdc.gov/ncbddd/autism/data.html
4. Gardener, H., Spiegelman, D., & Buka, S. L. (2011). Perinatal and neonatal risk factors for autism: a comprehensive meta-analysis. Pediatrics, 128(2), 344-355.
5. Maenner, M. J., Shaw, K. A., Bakian, A. V., et al. (2023). Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2020. MMWR Surveillance Summaries, 72(2), 1-14.
6. Modabbernia, A., Velthorst, E., & Reichenberg, A. (2017). Environmental risk factors for autism: an evidence-based review of systematic reviews and meta-analyses. Molecular Autism, 8(1), 13.
7. Schieve, L. A., Tian, L. H., Baio, J., et al. (2014). Population attributable fractions for three perinatal risk factors for autism spectrum disorders, 2002 and 2008 autism and developmental disabilities monitoring network. Annals of Epidemiology, 24(4), 260-266.
8. Xiang, A. H., Wang, X., Martinez, M. P., et al. (2015). Association of maternal diabetes with autism in offspring. JAMA, 313(14), 1425-1434.
Similar Posts

Prenatal Alcohol Exposure and Autism: Examining the Potential Connection
A single glass of wine during pregnancy could be the butterfly effect that alters a child’s neurodevelopmental trajectory, sparking a controversial debate about the potential link between prenatal alcohol consumption and autism spectrum disorders. This contentious issue has been the subject of intense scrutiny and research in recent years, as scientists and medical professionals strive…

Prenatal Drug Exposure and Autism: Exploring the Potential Link and Risks
As expectant mothers cradle their growing bellies, a silent storm brews within, where the choices of today ripple through generations, potentially shaping the intricate dance of neurons that may lead to autism. The relationship between prenatal drug exposure and autism spectrum disorder (ASD) has become a topic of increasing concern and scientific inquiry in recent…

Environmental Factors and Autism: The Complex Relationship Explained
Whispers of the womb and echoes of the environment intertwine in a dance that may shape the intricate puzzle of autism spectrum disorders. This complex interplay between nature and nurture has long captivated researchers, clinicians, and families alike, as they seek to unravel the mysteries surrounding the development of autism. As our understanding of this…

Metformin in Pregnancy and Autism: Exploring the Link and Potential Effects
Tiny pills swallowed during pregnancy ripple through time, potentially shaping the intricate wiring of young minds long after birth. This thought-provoking concept has sparked intense debate and research in the medical community, particularly concerning the use of metformin during pregnancy and its possible connection to autism spectrum disorder (ASD). As expectant mothers navigate the complex…

Albuterol and Pregnancy: Potential Link to Autism Examined
Breathless anticipation grips expectant mothers as they navigate the delicate balance between managing their asthma and safeguarding their unborn child’s neurological future. For many pregnant women with asthma, the use of albuterol as a rescue medication is a common and often necessary part of their healthcare regimen. However, recent concerns about the potential link between…

Premature Birth and Autism: Exploring the Complex Relationship and Addressing Concerns
Whispers of genetic code and the ticking of a biological clock intertwine in the delicate dance between premature birth and autism, leaving scientists and parents alike grappling for answers. This complex relationship has been the subject of extensive research and debate in recent years, as medical professionals and families seek to understand the potential connections…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

COMMENTS
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
In a breech presentation, the body comes out first, leaving the baby's head to be delivered last. The baby's body may not stretch the cervix enough to allow room for the baby's head to come out easily. There is a risk that the baby's head or shoulders may become wedged against the bones of the mother's pelvis.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
Breech presentation, which occurs in approximately 3 percent of fetuses at term, describes the fetus whose presenting part is the buttocks and/or feet. Although most breech fetuses have normal anatomy, this presentation is associated with an increased risk for congenital malformations and mild deformations, torticollis, and developmental ...
A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks ...
Breech delivery is the single most common abnormal presentation. The incidence is highly dependent on the gestational age. At 20 weeks, about one in four pregnancies are breech presentation. By full term, the incidence is about 4%. Other contributing factors include: Abnormal shape of the pelvis, uterus, or abdominal wall,
Breech presentation is associated with uterine and congenital abnormalities, and has a significant recurrence risk. Term babies presenting by the breech have worse outcomes than cephalic presenting babies, irrespective of the mode of delivery. A large reduction in the incidence of planned vaginal breech birth followed publication of the Term ...
Summary. Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal ...
Breech presentation: clinical practice guideline from the French College of Gynaecologists and Obstetricians [2020] ... compared to a C/S without also discussing the risks of a C/S when a breech presentation is diagnosed prior to labour, has the potential to sway clinician attitudes and therefore birth mode decision-making in women. ...
Management of Breech Presentation. ... Women should be informed that when planning delivery for a breech baby, the risk of perinatal mortality is approximately 0.5/1000 with caesarean section after 39 +0 weeks of gestation; and approximately 2.0/1000 with planned vaginal breech birth. This compares to approximately 1.0/1000 with planned ...
Labour with a preterm breech should be managed as with a term breech. C. Where there is head entrapment, incisions in the cervix (vaginal birth) or vertical uterine D incision extension (caesarean section) may be used, with or without tocolysis. Evidence concerning the management of preterm labour with a breech presentation is lacking.
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Introduction. Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman's and the baby's health. The aim of this review is to determine the most ...
Breech presentation is a type of malpresentation and occurs when the fetal head lies over the uterine fundus and fetal buttocks or feet present over the maternal pelvis (instead of cephalic/head presentation). The incidence in the United Kingdom of breech presentation is 3-4% of all fetuses. 1.
Breech and external cephalic version. Breech presentation is when the fetus is lying longitudinally and its buttocks, foot or feet are presenting instead of its head. Figure 1. Breech presentations. Breech presentation occurs in three to four per cent of term deliveries and is more common in nulliparous women.
Overview. Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of ...
Breech presentation delivery approach is a controversial issue in obstetrics. How to cope with breech delivery (vaginal or C-section) has been discussed to find the safest in terms of morbidity. ... Term breech birth risks have been analysed according to two possibilities: Vaginal delivery and caesarean delivery risks. Caesarean had high rates ...
Management of breech presentation Objectives: To provide health professionals and women with information regarding the benefits and risks of their options when a breech presentation is diagnosed either at term or at planned or spontaneous preterm birth. Target audience: Health professionals providing maternity care.
1 INTRODUCTION. In about 3% of term pregnancies, the fetus is in a breech position with the bottom, feet or knee first. 1-3 If the fetus remains in breech position after an attempted external cephalic version, there are two options available: planned vaginal breech delivery (PVD) or planned cesarean breech delivery (PCD). 4 Both options are associated with risks.
Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies. Breech is very common in early pregnancy, and by 36-37 weeks of pregnancy, most babies turn naturally into the head-first position. Towards the end of pregnancy, only 3-4 in every 100 (3-4%) babies are in the breech ...
Turning a breech baby. If your baby is in a breech position at 36 weeks, you'll usually be offered an external cephalic version (ECV). This is when a healthcare professional, such as an obstetrician, tries to turn the baby into a head-down position by applying pressure on your abdomen. It's a safe procedure, although it can be a bit uncomfortable.
Key Highlights. Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and ...
The risk of treatment with continuous positive airway pressure was increased when UC-pH levels were less than 7.20, and the risk of hypoglycemia was 21.5% if UC-pH levels were less than 7.10. ... (shoulder dystocia, uterine rupture, placental abruption, cord prolapse, or vasa praevia), breech presentation, instrumental delivery, and emergency ...
There are three main types of breech presentations: 1. Frank breech: The baby's buttocks are aimed at the birth canal with the legs sticking straight up in front of the body and the feet near the head. 2. Complete breech: The baby's buttocks are down, with the legs folded at the knees and feet near the buttocks. 3.