
SARINA SCHRAGER, MD, MS, JULIANNE FALLERONI, DO, MPH, AND JENNIFER EDGOOSE, MD, MPH
A more recent article on endometriosis is available.
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2013;87(2):107-113
Patient information : A handout on this topic is available at https://familydoctor.org/online/famdocen/home/women/reproductive/gynecologic/476.html .
Author disclosure: No relevant financial affiliations to disclose.
Endometriosis, which affects up to 10 percent of reproductive-aged women, is the presence of endometrial tissue outside of the uterine cavity. It is more common in women with pelvic pain or infertility ([corrected] 70 to 90 percent and 21 to 40 percent, respectively). Some women with endometriosis are asymptomatic, whereas others present with symptoms such as debilitating pelvic pain, dysmenorrhea, dyspareunia, and decreased fertility. Diagnosis of endometriosis in primary care is predominantly clinical. Initial treatment includes common agents used for primary dysmenorrhea, such as nonsteroidal anti-inflammatory drugs, combination estrogen/progestin contraceptives, or progestin-only contraceptives. There is some evidence that these agents are helpful and have few adverse effects. Referral to a gynecologist is necessary if symptoms persist or the patient is unable to become pregnant. Laparoscopy is commonly used to confirm the diagnosis before additional treatments are pursued. Further treatments include gonadotropin-releasing hormone analogues, danazol, or surgical removal of ectopic endometrial tissue. These interventions may control symptoms more effectively than initial treatments, but they can have significant adverse effects and limits on duration of therapy.
Endometriosis is defined as the presence of endometrial glandular and/or stromal cells outside of the uterine cavity. There are generally three distinct clinical presentations: endometrial implantation superficially on the peritoneum; endometrial lined ovarian cysts (chocolate cysts) or endometriomas; and endometriotic nodules (a complex, solid mass of endometrial, adipose, and fibromuscular tissue found between the rectum and vagina). 1 However, further laparoscopic studies of the peritoneum also have shown nonclassic lesions, such as clear vesicles, red vesicles, or microscopic disease. 2 Typically, ectopic endometrial tissue is found within the pelvis ( Table 1 ) . 3 Although reported in virtually all organ systems, extrapelvic deposition is exceedingly rare.
Endometriosis is generally considered a benign disease. However, several large cohort studies suggest that endometriosis is an independent risk factor for clear-cell carcinoma and endometrioid ovarian carcinoma. 4
| Transvaginal ultrasonography is the preferred imaging modality for women with suspected endometriosis. | C | |
| Ovulation suppression therapies, such as oral contraceptives and gonadotropin-releasing hormone analogues, are effective for treating endometriosis pain. | A | , , |
| Surgical treatment of endometriosis improves pregnancy rates. | A | , |
| Ovulation suppression therapies do not improve pregnancy rates in patients with endometriosis. | A |
| Ovaries | 55 |
| Anterior cul-de-sac | 35 |
| Posterior broad ligaments | 35 |
| Posterior cul-de-sac | 34 |
| Uterosacral ligaments | 28 |
The earliest and most widely accepted theory of endometriosis etiology is that refluxed menstrual tissue enters the pelvic peritoneal cavity and embeds into other intra-abdominal areas. 5 , 6 This theory is supported by the fact that the most commonly affected sites are closest to the fallopian tubes. 6 In addition, endometriosis often occurs in women with outflow obstruction, such as cervical stenosis, a transverse vaginal septum, and an imperforate hymen. 7
Although women with endometriosis have higher volumes of refluxed menstrual blood and endometrial tissue, 8 most women have some component of retrograde menstruation. The plasminogen activator inhibitor gene has been shown to increase the likelihood of endometrial implantation after retrograde menstruation. 6
The coelomic metaplasia theory of endometriosis proposes that the coelomic epithelium of the peritoneal cavity retains multipotential cells that can develop into endometriotic tissue. This explains rare cases of endometriosis in prepubertal girls, women with Müllerian agenesis, and men. 6 Another theory is that endometrial tissue can be transported to distant sites via lymphatic and vascular channels, which explains rare cases of extra-abdominal endometriosis. 6 Finally, newer research suggests an immunologic component to the development of endometriosis. Concentrations of macrophages, leptin, tumor necrosis factor-α, and interleukin-6 often are higher in the abdominal fluid of women with endometriosis. 6 , 9 , 10

Epidemiology
Endometriosis is an estrogen-dependent disease predominantly affecting reproductive-aged women, with the highest incidence among women 25 to 29 years of age. 11 The prevalence of endometriosis in the general population is difficult to accurately assess because some women with the disease have limited or no symptoms. Some studies suggest that it affects up to 10 percent of reproductive-aged women. 12 [corrected] Endometriosis is diagnosed in 21 to 40 percent of women with infertility 13 and in 70 to 90 percent of women with chronic pelvic pain. 14
In the United States, endometriosis is the third leading cause of gynecologic hospitalizations. 15 It is estimated that the disease leads to $2,801 in health care costs and $1,023 in lost productivity at work per patient annually. 16 In one nationwide survey, 50 percent of women with endometriosis reported spending entire days in bed over the previous 12 months because of the condition, with an average of 17.8 days spent in bed. 17
Risk Factors
It has been reported that the risk of endometriosis is six times higher in first-degree relatives of women with severe endometriosis. 9 However, a more recent case-control study showed that the familial impact on the incidence of endometriosis is not significant. 18
Early menarche and late menopause, which lead to increased exposure to menstruation, are commonly cited risk factors for endometriosis. 5 , 19 However, epidemiologic studies are equivocal as to whether these are true risk factors or findings associated with the disease itself. 20 Low body mass index 21 , 22 and higher caffeine or alcohol consumption 21 also are associated with an increased risk of endometriosis. Table 2 includes possible risk factors for the disease. 20 – 22 Oral contraceptives and regular exercise (i.e., more than four hours per week) may decrease the risk. 5 , 21
| Early menarche |
| First-degree relative with endometriosis |
| Late menopause |
| Low body mass index |
| Müllerian anomalies |
| Nulliparity |
| Prolonged menstruation (> five days) |
| Shorter lactation intervals |
| Shorter menstrual cycles (< 28 days) |
| White race (compared with black race) |
Clinical Presentation
The clinical presentation of endometriosis is highly variable and ranges from debilitating pelvic pain and infertility to no symptoms. Table 3 lists the symptoms and comorbidities that are associated with higher rates of endometriosis. 23 In a large case-control study in the United Kingdom, 73 percent of women with endometriosis reported dysmenorrhea, abdominal or pelvic pain, or menorrhagia, compared with 20 percent of women without the disease. 23 Many women with endometriosis present with nonspecific symptoms, such as chronic lower back pain or abdominal pain, which may delay diagnosis. Table 4 includes the differential diagnosis of common symptoms of endometriosis. 5 It takes an average of 11.7 years for endometriosis to be diagnosed in a woman with symptoms. 24
| / | |
|---|---|
| Infertility/subfertility | 8.2 (6.9 to 9.9) |
| Dysmenorrhea | 8.1 (7.2 to 9.3) |
| Ovarian cysts | 7.3 (5.7 to 9.4) |
| Dyspareunia and/or postcoital bleeding | 6.8 (5.7 to 8.2) |
| Abdominal or pelvic pain | 5.2 (4.7 to 5.7) |
| Pelvic inflammatory disease | 3.0 (2.5 to 3.6) |
| Irritable bowel syndrome | 1.6 (1.3 to 1.8) |
| Adnexal masses | Benign and malignant ovarian cysts, hydrosalpinges |
| Chronic lower abdominal pain | Irritable bowel syndrome, neuropathic pain, adhesions, pelvic vascular congestion |
| Chronic lower back pain | Musculoskeletal strain |
| Dyschezia (i.e., difficulty with defecation) | Constipation, anal fissures |
| Dysmenorrhea | Adenomyosis, physiologic etiology |
| Dyspareunia | Psychosexual problems, vaginal atrophy, infectious vaginitis or cervicitis, vulvodynia |
| Dysuria | Urinary tract infection, interstitial cystitis |
| Infertility | Anovulation, luteal phase deficiency, cervical or tubal structural or infectious pathology, male factor infertility |
Similarly, objective physical examination findings are limited and nonspecific. Although many women with endometriosis will have normal examination findings, some will exhibit tenderness of the posterior fornix, limited motion of the uterus or ovaries, or an adnexal mass. Some women will have diffuse tenderness on pelvic examination. However, in women undergoing evaluation for infertility, uterosacral nodularity with associated tenderness is pathognomonic for endometriosis. 25
The diagnosis of endometriosis in primary care is initially clinical and based on history and physical examination findings. Histologic confirmation is usually achieved with the detection of extrauterine endometrial cells on laparoscopy. Less invasive diagnostic tests are being pursued. Transvaginal ultrasonography can reliably detect cystic endometriomas (89 percent sensitivity, 91 percent specificity) and is considered the imaging modality of choice, 26 , 27 although the test does not reliably detect smaller endometrial implants. The cancer antigen 125 assay has been extensively researched, but a large systematic review of 23 studies shows limited overall value in the diagnosis of endometriosis. The cancer antigen 125 level is often elevated in women with endometriosis, but its specificity for the disease is low. 28 Magnetic resonance imaging also is being explored, particularly for deeper rectosigmoid and ureteral infiltrating lesions, but it is not a standard diagnostic tool because of its low sensitivity. 29
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first-line treatment for endometriosis, followed by hormone therapy. Laparoscopy can be used to confirm the diagnosis before additional treatments are pursued; empiric therapy with another suppressive medication is also an option. Table 5 summarizes evidence-based therapies. 30 – 37 Figure 1 is an algorithm for treating endometriosis in primary care.
| NSAIDs | A 2009 Cochrane review including only one small RCT of naproxen versus placebo showed no conclusive evidence that NSAIDs improve pain; however, because NSAIDs are effective for primary dysmenorrhea, consensus opinion suggests they are reasonable as a first-line treatment for suspected endometriosis |
| Combination oral contraceptives | A 2007 Cochrane review including only one study comparing combination oral contraceptives with gonadotropin-releasing hormone analogues showed that both were comparable for pain relief ; a Japanese RCT showed that low-dose combined oral contraceptives improved pain compared with placebo |
| Medroxyprogesterone | Small RCTs show that oral medroxyprogesterone (Provera) and depot medroxyprogesterone (Depo-Provera, Depo-subQ Provera) are beneficial for pain , |
| Levonorgestrel-releasing intrauterine system (Mirena) | Small nonrandomized studies show possible benefit for pain , |
| Gonadotropin-releasing hormone analogues | A 2010 Cochrane review showed effectiveness ; however, adverse effects (i.e., menopausal symptoms) limit its use |
| Danazol | A 2007 Cochrane review showed effectiveness ; however, androgenic adverse effects limit its use |
NONSTEROIDAL ANTI-INFLAMMATORY DRUGS
A Cochrane review evaluated NSAIDs in the treatment of endometriosis, but included only one randomized controlled trial (n = 24), which compared naproxen with placebo. 30 There was no difference in pain relief between naproxen and placebo, and there was no evidence that one NSAID is superior.
NSAIDs often are attempted first because they are beneficial in women with primary dysmenorrhea, are available over the counter, and are relatively safe. Although endometriosis is a condition of secondary dysmenorrhea, it seems reasonable to consider NSAIDs as a first-line treatment in women with suspected endometriosis.
COMBINATION ESTROGEN/PROGESTIN CONTRACEPTIVES
Combination oral contraceptives are more effective than placebo at reducing dysmenorrhea in women with endometriosis. 31 – 33 A double-blind, randomized controlled trial of 100 women with endometriosis demonstrated that low-dose combination oral contraceptives improved endometriosis pain compared with placebo. 32 Another study showed that combination oral contraceptives were less effective at six months compared with gonadotropin-releasing hormone (GnRH) analogues, although both significantly improved symptoms after 12 months. 38 Combination oral contraceptives have significantly fewer adverse effects than GnRH analogues.
A small, prospective, nonblinded, cohort study compared the ethinyl estradiol/etonogestrel vaginal ring (Nuvaring) with the norelgestromin/ethinyl estradiol transdermal patch (Ortho Evra) in patients with endometriosis. 39 Although continuous use of both treatments reduced pain, the ring was superior for dysmenorrhea. Patient satisfaction also seemed higher in patients using the ring. Continuous use of these treatments resulted in more breakthrough bleeding compared with cyclic use.
PROGESTERONE-ONLY CONTRACEPTIVES
Medroxyprogesterone (oral [Provera] or depot injection [Depo-Provera]) may improve symptoms of endometriosis compared with placebo. 33 Two trials comparing a lower-dose depot medroxyprogesterone (Depo-subQ Provera) with the GnRH analogue leuprolide (Lupron) showed comparable improvement in pain. 34 , 40 Both trials indicated that depot medroxyprogesterone resulted in less bone loss and hypoestrogenic adverse effects than leuprolide; however, depot medroxyprogesterone labels include U.S. Food and Drug Administration boxed warnings for bone loss. Two studies comparing dienogest (a new selective progestin that is not yet available in the United States) with GnRH analogues also showed comparable improvement in pain. 41 , 42
A small study showed that the etonogestrel subdermal implant (Implanon) was as effective as depot medroxyprogesterone for endometriosis pain. 43 Small nonrandomized studies have shown a possible improvement in endometriosis pain with the levonorgestrel-releasing intrauterine system (Mirena). 33 , 35
GONADOTROPIN-RELEASING HORMONE ANALOGUES
If NSAIDs and hormonal contraceptives are ineffective, the next step is treatment with a GnRH analogue such as leuprolide or goserelin (Zoladex). GnRH analogue therapy downregulates the pituitary, resulting in “medical menopause,” 44 and has been shown to improve pain in women with endometriosis. 36 However, the therapy causes adverse effects, such as hot flashes, night sweats, and possible bone loss, in many women. To mitigate the menopausal symptoms, reinitiating hormone therapy with low-dose estrogen and progestin is common.
Danazol, an androgen, is effective in the treatment of pelvic pain associated with endometriosis. 37 However, androgenic adverse effects, such as acne, hirsutism, and male pattern baldness, often limit its use. The drug has several U.S. Food and Drug Administration boxed warnings, including the risk of thrombosis and teratogenicity.
SURGICAL OPTIONS
Laparoscopic ablation of deposits and excision of endometriomas are options to relieve pain and treat infertility. Excision of endometriomas will more effectively improve pregnancy rates than a drainage and ablation technique, but there is little evidence on the success of surgical treatment in advanced disease. 26 , 45 If a woman with endometriosis does not desire future pregnancy and all medical treatments and conservative surgical therapies have been ineffective, a hysterectomy may be performed.
FUTURE TREATMENTS
Several medications are under evaluation for the treatment of endometriosis, including mifepristone (Mifeprex); aromatase inhibitors (i.e., letrozole [Femara], anastrozole [Arimidex], and exemestane [Aromasin]); Chinese herbal medications; gestrinone (a 19-nortestosterone derivative that has antiprogestational and antiestrogenic properties; not available in the United States); immunomodulators (i.e., pentoxifylline [Trental] and interferon); and selective estrogen receptor modulators. 33 Acupuncture may also be effective in the treatment of pain. 46
Managing Endometriosis-Related Infertility
Women with infertility due to endometriosis usually will undergo laparoscopy. In women with mild endometriosis diagnosed by laparoscopy, surgical treatment of lesions improves pregnancy rates compared with no treatment of lesions. 26 , 47
A Cochrane review evaluated 25 randomized controlled trials comparing oral contraceptives, progestins, and danazol with placebo to determine the effectiveness of temporary ovulation suppression for endometriosis-related infertility. 45 The review measured outcomes related to effects on subsequent fertility, such as live birth after 20 weeks' gestation and clinical pregnancy (evidenced by fetal heart motion and gestational sac) compared with adverse events (i.e., miscarriage, ectopic pregnancy, fetal abnormalities, adverse drug effects). The review showed that ovulation suppression had no effect on subsequent fertility compared with placebo.
Data Sources: We searched PubMed, the Cochrane Database of Systematic Reviews, the National Guideline Clearinghouse, and Clinical Evidence using the search terms endometriosis, etiology of endometriosis, epidemiology of endometriosis, treatment of endometriosis, and infertility associated with endometriosis. Search dates: December 2010 to January 2011.
Bulun SE. Endometriosis. N Engl J Med. 2009;360(3):268-279.
Eltabbakh GH, Bower NA. Laparoscopic surgery in endometriosis. Minerva Ginecol. 2008;60(4):323-330.
Jenkins S, Olive DL, Haney AF. Endometriosis: pathogenetic implications of the anatomic distribution. Obstet Gynecol. 1986;67(3):335-338.
Van Gorp T, Amant F, Neven P, Vergote I, Moerman P. Endometriosis and the development of malignant tumours of the pelvis. A review of literature. Best Pract Res Clin Obstet Gynaecol. 2004;18(2):349-371.
Farquhar C. Endometriosis. BMJ. 2007;334(7587):249-253.
Bedaiwy MA, Abdel-Aleem MA, Miketa A, Falcone T. Endometriosis: a critical appraisal of the advances and the controversies of a challenging health problem. Minerva Ginecol. 2009;61(4):285-298.
Olive DL, Henderson DY. Endometriosis and mullerian anomalies. Obstet Gynecol. 1987;69(3 pt 1):412-415.
Halme J, Hammond MG, Hulka JF, Raj SG, Talbert LM. Retrograde menstruation in healthy women and in patients with endometriosis. Obstet Gynecol. 1984;64(2):151-154.
Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364(9447):1789-1799.
Harada T, Taniguchi F, Izawa M, et al. Apoptosis and endometriosis. Front Biosci. 2007;12:3140-3151.
Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol. 2004;160(8):784-796.
Wheeler JM. Epidemiology of endometriosis-associated infertility. J Reprod Med. 1989;34(1):41-46.
Strathy JH, Molgaard CA, Coulam CB, Melton LJ. Endometriosis and infertility: a laparoscopic study of endometriosis among fertile and infertile women. Fertil Steril. 1982;38(6):667-672.
Ozawa Y, Murakami T, Terada Y, et al.. Management of the pain associated with endometriosis: an update of the painful problems. Tohoku J Exp Med. 2006;210(3):175-188.
Velebil P, Wingo PA, Xia Z, Wilcox LS, Peterson HB. Rate of hospitalization for gynecologic disorders among reproductive-age women in the United States. Obstet Gynecol. 1995;86(5):764-769.
Simoens S, Hummelshoj L, D'Hooghe T. Endometriosis: cost estimates and methodological perspective. Hum Reprod Update. 2007;13(4):395-404.
Kjerulff KH, Erickson BA, Langenberg PW. Chronic gynecological conditions reported by US women: findings from the National Health Interview Survey, 1984 to 1992. Am J Public Health. 1996;86(2):195-199.
Nouri K, Ott J, Krupitz B, Huber JC, Wenzl R. Family incidence of endometriosis in first-, second-, and third-degree relatives: case-control study. Reprod Biol Endocrinol. 2010;8:85.
Missmer SA, Hankinson SE, Spiegelman D, et al. Reproductive history and endometriosis among premenopausal women. Obstet Gynecol. 2004;104(5 pt 1):965-974.
Treloar SA, Bell TA, Nagle CM, Purdie DM, Green AC. Early menstrual characteristics associated with subsequent diagnosis of endometriosis. Am J Obstet Gynecol. 2010;202(6):534.e1-6.
Ozkan S, Murk W, Arici A. Endometriosis and infertility: epidemiology and evidence-based treatments. Ann N Y Acad Sci. 2008;1127:92-100.
Hediger ML, Hartnett HJ, Louis GM. Association of endometriosis with body size and figure. Fertil Steril. 2005;84(5):1366-1374.
Ballard KD, Seaman HE, de Vries CS, Wright JT. Can symptomatology help in the diagnosis of endometriosis? Findings from a national case-control study—part 1. BJOG. 2008;115(11):1382-1391.
Hadfield R, Mardon H, Barlow D, Kennedy S. Delay in the diagnosis of endometriosis: a survey of women from the USA and the UK. Hum Reprod. 1996;11(4):878-880.
Matorras R, Rodríguez F, Pijoan JI, et al. Are there any clinical signs and symptoms that are related to endometriosis in infertile women?. Am J Obstet Gynecol. 1996;174(2):620-623.
Practice bulletin no. 114: management of endometriosis. Obstet Gynecol. 2010;116(1):223-236.
Alcázar JL, Laparte C, Jurado M, López-García G. The role of transvaginal ultrasonography combined with color velocity imaging and pulsed Doppler in the diagnosis of endometrioma. Fertil Steril. 1997;67(3):487-491.
Mol BW, Bayram N, Lijmer JG, et al. The performance of CA-125 measurement in the detection of endometriosis: a meta-analysis. Fertil Steril. 1998;70(6):1101-1108.
Brosens I, Puttemans P, Campo R, Gordts S, Kinkel K. Diagnosis of endometriosis: pelvic endoscopy and imaging techniques. Best Pract Res Clin Obstet Gynaecol. 2004;18(2):285-303.
Allen C, Hopewell S, Prentice A, Gregory D. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. ;2009(2):CD004753.
Davis L, Kennedy SS, Moore J, Prentice A. Modern combined oral contraceptives for pain associated with endometriosis. Cochrane Database Syst Rev. ;2007(3):CD001019.
Harada T, Momoeda M, Taketani Y, Hoshiai H, Terakawa N. Low-dose oral contraceptive pill for dysmenorrhea associated with endometriosis: a placebo-controlled, double-blind, randomized trial. Fertil Steril. 2008;90(5):1583-1588.
Ferrero S, Remorgida V, Venturini PL. Current pharmacotherapy for endometriosis. Expert Opin Pharmacother. 2010;11(7):1123-1134.
Schlaff WD, Carson SA, Luciano A, Ross D, Bergqvist A. Subcutaneous injection of depot medroxyprogesterone acetate compared with leuprolide acetate in the treatment of endometriosis-associated pain. Fertil Steril. 2006;85(2):314-325.
Lockhat FB, Emembolu JO, Konje JC. The efficacy, side-effects and continuation rates in women with symptomatic endometriosis undergoing treatment with an intra-uterine administered progestogen (levonorgestrel): a 3 year follow-up. Hum Reprod. 2005;20(3):789-793.
Brown J, Pan A, Hart RJ. Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. Cochrane Database Syst Rev. ;2010(12):CD008475.
Selak V, Farquhar C, Prentice A, Singla A. Danazol for pelvic pain associated with endometriosis. Cochrane Database Syst Rev. ;2007(4):CD000068.
Ferrero S, Remorgida V, Venturini PL. Endometriosis. Clin Evid (Online) . August 13, 2010. http://clinical-evidence.bmj.com/ceweb/conditions/woh/0802/0802-get.pdf [login required]. Accessed February 15, 2011.
Vercellini P, Barbara G, Somigliana E, Bianchi S, Abbiati A, Fedele L. Comparison of contraceptive ring and patch for the treatment of symptomatic endometriosis. Fertil Steril. 2010;93(7):2150-2161.
Crosignani PG, Luciano A, Ray A, Bergqvist A. Subcutaneous depot medroxyprogesterone acetate versus leuprolide acetate in the treatment of endometriosis-associated pain. Hum Reprod. 2006;21(1):248-256.
Strowitzki T, Marr J, Gerlinger C, Faustmann T, Seitz C. Dienogest is as effective as leuprolide acetate in treating the painful symptoms of endometriosis: a 24-week, randomized, multicentre, open-label trial. Hum Reprod. 2010;25(3):633-641.
Harada T, Momoeda M, Taketani Y, et al. Dienogest is as effective as intranasal buserelin acetate for the relief of pain symptoms associated with endometriosis—a randomized, double-blind, multicenter, controlled trial. Fertil Steril. 2009;91(3):675-681.
Walch K, Unfried G, Huber J, et al. Implanon versus medroxyprogesterone acetate: effects on pain scores in patients with symptomatic endometriosis—a pilot study. Contraception. 2009;79(1):29-34.
de Ziegler D, Borghese B, Chapron C. Endometriosis and infertility: pathophysiology and management. Lancet. 2010;376(9742):730-738.
Hughes E, Brown J, Collins JJ, Farquhar C, Fedorkow DM, Vandekerckhove P. Ovulation suppression for endometriosis. Cochrane Database Syst Rev. ;2007(3):CD000155.
Rubi-Klein K, Kucera-Sliutz E, Nissel H, et al. Is acupuncture in addition to conventional medicine effective as pain treatment for endometriosis? A randomised controlled cross-over trial. Eur J Obstet Gynecol Reprod Biol. 2010;153(1):90-93.
Jacobson TZ, Duffy JM, Barlow D, Farquhar C, Koninckx PR, Olive D. Laparoscopic surgery for subfertility associated with endometriosis. Cochrane Database Syst Rev. ;2010(1):CD001398.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2013 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Research article
- Open access
- Published: 13 August 2015
Gastrointestinal symptoms among endometriosis patients—A case-cohort study
- Malin Ek 1 ,
- Bodil Roth 1 ,
- Per Ekström 2 ,
- Lil Valentin 2 ,
- Mariette Bengtsson 3 &
- Bodil Ohlsson 1
BMC Women's Health volume 15 , Article number: 59 ( 2015 ) Cite this article
20k Accesses
61 Citations
16 Altmetric
Metrics details
Women with endometriosis often experience gastrointestinal symptoms. Gonadotropin-releasing hormone (GnRH) analogs are used to treat endometriosis; however, some patients develop gastrointestinal dysmotility following this treatment. The aims of the present study were to investigate gastrointestinal symptoms among patients with endometriosis and to examine whether symptoms were associated with menstruation, localization of endometriosis lesions, or treatment with either opioids or GnRH analogs, and if hormonal treatment affected the symptoms.
All patients with diagnosed endometriosis at the Department of Gynecology were invited to participate in the study. Gastrointestinal symptoms were registered using the Visual Analogue Scale for Irritable Bowel Syndrome (VAS-IBS); socioeconomic and medical histories were compiled using a clinical data survey. Data were compared to a control group from the general population.
A total of 109 patients and 65 controls were investigated. Compared to controls, patients with endometriosis experienced significantly aggravated abdominal pain ( P = 0.001), constipation ( P = 0.009), bloating and flatulence ( P = 0.000), defecation urgency ( P = 0.010), and sensation of incomplete evacuation ( P = 0.050), with impaired psychological well-being ( P = 0.005) and greater intestinal symptom influence on their daily lives ( P = 0.001). The symptoms were not associated with menstruation or localization of endometriosis lesions, except increased nausea and vomiting ( P = 0.010) in patients with bowel-associated lesions. Half of the patients were able to differentiate between abdominal pain from endometriosis and from the gastrointestinal tract. Patients using opioids experienced more severe symptoms than patients not using opioids, and patients with current or previous use of GnRH analogs had more severe abdominal pain than the other patients ( P = 0.024). Initiation of either combined oral contraceptives or progesterone for endometriosis had no effect on gastrointestinal symptoms when the patients were followed prospectively.
Conclusions
The majority of endometriosis patients experience more severe gastrointestinal symptoms than controls. A poor association between symptoms and lesion localization was found, indicating existing comorbidity between endometriosis and irritable bowel syndrome (IBS). Treatment with opioids or GnRH analogs is associated with aggravated gastrointestinal symptoms.
Peer Review reports
Endometriosis is a benign, gynecological disease associated with the primary symptoms of chronic pelvic pain, deep dyspareunia, and dysmenorrhea [ 1 ]. The prevalence of endometriosis differs in the literature, but is estimated to affect approximately 7–10 % of women [ 2 ]. Clinically, women with endometriosis commonly experience gastrointestinal symptoms, and one study has shown that gastrointestinal symptoms are almost as common as gynecological symptoms in these patients [ 3 ].
Gastrointestinal symptoms among patients with endometriosis described in the literature include abdominal pain, bloating, nausea, constipation, vomiting, painful bowel movements, and diarrhea [ 3 – 5 ]. However, reported symptoms differ between studies. Aggravated symptoms during menstruation have been reported [ 4 , 6 , 7 ] such as cyclic-related bloating and constipation [ 4 ]. Fauconnier et al. [ 7 ] concluded that symptoms including diarrhea, constipation, and colic rectal pain were more frequent among patients with endometriosis lesions within or close to the bowel. In contrast, Maroun et al. [ 3 ] reported gastrointestinal symptoms to be primarily independent of localization of endometriosis lesions in relation to the bowel. Different explanations concerning the occurrence of these symptoms include: endometriosis lesions cause inflammatory activity and local prostaglandin release, which can alter bowel function [ 8 ]; endometriosis lesions within the bowel cause symptoms due to mechanical obstruction or cyclic micro-hemorrhages [ 9 ]; or there is an existing comorbidity between endometriosis and irritable bowel syndrome (IBS) [ 8 ].
Gonadotropin-releasing hormone (GnRH) is a hypothalamic hormone [ 10 ], which has also been shown to be present in neurons in the human enteric nervous system (ENS) [ 11 ]. Recent studies have suggested a link between GnRH and gastrointestinal function [ 12 , 13 ], and some patients develop severe dysmotility in the form of chronic intestinal pseudo-obstruction (CIPO) or enteric dysmotility (ED) after treatment with GnRH analogs in relation to in vitro fertilization (IVF) or endometriosis [ 14 ]. Full-thickness biopsies of the bowel wall have shown enteric neurodegeneration with almost total absence of GnRH-containing neurons [ 11 , 14 , 15 ]. Hammar et al. [ 13 ] investigated 124 patients before and after treatment with GnRH analogs and concluded that there was a significant exacerbation of gastrointestinal symptoms after treatment, and abdominal pain was still exacerbated at 5-year follow-up.
The aim of the present study was to investigate the severity of gastrointestinal symptoms among patients with endometriosis compared to a control group from the general population. Furthermore, an association between symptoms and menstruation, localization of endometriosis lesions, and treatment with opioids or GnRH analogs was investigated. The final aim was to investigate women initiating hormonal treatment to examine whether this treatment had an impact on gastrointestinal symptoms over time.
This study was approved by the Ethics Review Board of Lund University, Dnr 2012/564, and performed in accordance with the declaration of Helsinki. All subjects gave their written, informed consent before inclusion in the study.
Patients who had sought treatment for endometriosis in the past 5 years were recruited from the Department of Gynecology at Skåne University Hospital in Malmö. The patients were identified with the International Statistical Classification of Diseases and Related Health Problems, ICD-10, N80.1, 80.4, 80.5, 80.8, and 80.9 from Skåne University Hospital medical records. The clinic’s catchment area is the southernmost districts of Sweden. The recruitment was conducted continuously from March 2013 through July 2014. Inclusion criteria were a diagnosis of endometriosis made by laparoscopy, ultrasonography, or a definite clinical diagnosis made by a gynecologist. The included patients were also required to comprehend the Swedish or English language. Exclusion criteria were an uncertain diagnosis of endometriosis, patients living too far from the geographical area of Skåne University Hospital, multi-morbidity, current pregnancy, or a diagnosis of cancer, inflammatory bowel disease, multiple sclerosis, psychiatric disease, or rheumatoid arthritis.
Data regarding control subjects was obtained from a previous study conducted by Hammar et al. [ 13 ]. In this study, control subjects were randomly acquired from the Swedish Population Registry, and 248 subjects were contacted. In total, after one reminder, 29 questionnaires were returned. Because of the low response rate, further controls were recruited amongst female hospital staff. In total, 65 women representing the general population, with a mean age of 40 ± 9 years, were recruited and completed the Visual Analogue Scale for Irritable Bowel Syndrome (VAS-IBS).
Study design
The patients were contacted via mail, and within a week, they were also contacted via telephone. After agreement to participate in the study, an appointment for an interview and a blood draw was done 1–4 weeks after inclusion in the study. The questionnaire, Visual Analogue Scale for Irritable Bowel Syndrome (VAS-IBS), and a clinical data survey were sent via mail, with instructions to complete these questionnaires at a maximum of 1 week before the appointment. At the hospital visit, all patients were interviewed regarding previous treatment for endometriosis and their position in the menstrual cycle at the time of completing the VAS-IBS. The patients who were included at the first contact with the Department of Gynecology also completed the VAS-IBS questionnaire and the clinical data survey, were interviewed and had blood samples drawn at 3 and 6 months after their first visit.
A review of the patients’ medical journals was conducted to investigate the localization of endometriosis lesions, current hormonal treatment, and whether they had undergone diagnostic or operative laparoscopy. A lesion was confirmed when it was seen macroscopically during laparoscopy, visualized by ultrasonography, or in a few cases by palpation conducted by a gynecologist.
Questionnaires
Clinical data survey.
The clinical data survey addresses socioeconomic factors, physical exercise, nicotine- and alcohol habits, current diseases, and medication, as well as questions about gastrointestinal symptoms such as onset and triggers, whether the subject can differentiate between the abdominal pain from endometriosis and the gastrointestinal tract, and whether pharmacological treatment was used because of the complaints.
Three questions were added after the study was initiated: which year endometriosis-associated symptoms began; which year gastrointestinal symptoms began; and whether the patient could differentiate symptoms from endometriosis and symptoms from the gastrointestinal tract. Therefore, an additional survey with these questions was sent by mail to the 21 first participants already included in the study.
Visual Analogue Scale for Irritable Bowel Syndrome
The VAS-IBS was used to investigate gastrointestinal complaints in the study groups. It is a validated questionnaire for estimation of the most common gastrointestinal complaints in patients with non-organic, functional bowel disease [ 16 ]. This scale has also been validated for estimation of symptoms over time [ 17 ]. The seven items measured in the VAS-IBS address the symptoms abdominal pain, diarrhea, constipation, bloating and flatulence, nausea and vomiting, psychological well-being, and intestinal symptoms’ influence on daily life. These items were measured on a scale from 0 to 100, where 0 represents severe problems and 100 represents a complete lack of problems. An additional two questions, if the subject experienced defecation urgency and had a sensation of incomplete evacuation, were answered with yes or no.
Statistical methods
The data was analyzed using the statistical software package SPSS for Windows (release 22.0; IBM). Because the controls were slightly older than the endometriosis patients, variables were age-standardized using a linear regression model into which age was added as a covariate and the variables were then expressed as z-scores. When comparing VAS scores between groups, the age-standardized values were used. All variables were analyzed for normal distribution using the Kolomogorov-Smirnov test. As normality was rejected, except for age, the Mann-Whitney U -test and the Fisher’s exact test were used to compare different groups. Student t -test was used to perform a failure analysis. To calculate differences within the group, Friedman’s test and Wilcoxon’s signed rank test were used. Spearman’s correlation test was used for correlations between age and symptoms. Values were expressed as mean ± standard deviation (SD), median [interquartile range (IQR)], or number (n) and percent (%). P ≤ 0.05 was considered statistically significant.
Patient characteristics
A total of 627 patients with suspected endometriosis were identified. Of these, 320 were excluded because they either did not fulfill the inclusion criteria or they fulfilled the exclusion criteria. The most common reason for exclusion was uncertainty about the diagnosis. Then, 307 patients remained who fulfilled the inclusion criteria. Of these, 198 patients were excluded since 144 were not willing to participate, 49 had moved from the region, and 4 denied the diagnosis when contacted. Thus, 109 could finally be included in the study. Eighteen of these patients were followed prospectively regarding their gastrointestinal symptoms, and 14 of these initiated a new hormonal treatment for endometriosis during the study period.
The mean age of the 109 included patients was 37 ± 7 years. The median duration of endometriosis was 8.5 (4.0–16.0) years. Patients who were unwilling to participate in the study were younger (35 ± 6 years) than those who participated ( P = 0.014). Almost two-thirds of the patients had a degree from a university or a college. The vast majority had never smoked and consumed less than one standard glass of alcohol a week (Table 1 ). Aside from endometriosis the majority of patients were healthy ( n = 57), and the most common diseases reported were allergies or bronchial asthma ( n = 18) followed by migraine ( n = 7) and irritable bowel syndrome (IBS) ( n = 6).
Almost all patients had received hormonal treatment for endometriosis, most commonly combined oral contraceptives (Table 2 ). Of the 109 patients, 87 had laparoscopically-verified endometriosis, 21 had received their diagnosis by ultrasonography, and only one was diagnosed clinically. The most common localization of endometriosis lesions was in the ovaries ( n = 83), followed by the peritoneum ( n = 21), the bowel ( n = 18), and the Pouch of Douglas ( n = 16).
Patients’ gastrointestinal complaints
Of the patients, 85 % reported gastrointestinal complaints during the past year. The onset of symptoms had been gradual for a majority. The median duration of gastrointestinal symptoms was 5 months shorter than the median duration of endometriosis. One-third of the patients’ complaints had been diagnosed as IBS or endometriosis, but one out of five reported never having received any diagnosis for the symptoms. However, almost half of the patients reported having the ability to differentiate between pain symptoms from endometriosis and from the gastrointestinal tract. A variety of different triggers for the symptoms were described (Table 3 ). Nearly half of the patients had received pharmacological treatment for their gastrointestinal complaints; slightly less than one out of five had been treated with opioids, and almost half of the patients had been treated with other drugs than opioids, for example nonsteroidal anti-inflammatory drugs (NSAID), paracetamol, or anti-depressant medication. However, in many cases, it was not obvious whether the anti-depressant drugs were given for treatment of abdominal pain or depression (Table 4 ).
Gastrointestinal symptoms measured by the Visual Analogue Scale for Irritable Bowel Syndrome
Patients with endometriosis experienced aggravated symptoms compared to controls regarding abdominal pain, constipation, bloating and flatulence, and impaired psychological well-being and greater influence of intestinal symptoms on daily life. The endometriosis patients also experienced defecation urgency and a sensation of incomplete evacuation significantly more often (Table 5 ). Increasing patient age correlated with less diarrhea ( rs = 0.281, P = 0.03), less bloating and flatulence ( rs = 0.239, P = 0.013), less nausea and vomiting ( rs = 0.286, P = 0.003), and better psychological well-being ( rs = 0.295, P = 0.002), whereas age in controls did not correlate with symptoms (data not shown).
The patients with lesions within the bowel, or in close proximity to the bowel (the pouch of Douglas, the posterior wall of the vagina, or the recto-vaginal septum) ( n = 34), scored more severe symptoms regarding nausea and vomiting than the other patients [69.71 (33.75–100.00) vs. 84.36 (75.00–100.00); P = 0.010]. None of the other symptoms differed depending on localization of the lesions (data not shown).
The patients currently using opioids scored more severe symptoms than the other patients regarding all symptoms except sensation of incomplete evacuation (Table 6 ). The patients who were not currently using opioids scored more severe symptoms than controls regarding abdominal pain [66.12 (45.00–100.00) vs. 81.40 (73.00–98.00); P = 0.013], bloating and flatulence [53.96 (20.00–90.00) vs. 71.72 (41.75–96.00); P = 0.005], intestinal symptoms’ influence on daily life [66.01 (35.00–100.00) vs. 81.28 (75.00–98.00); P = 0.011], and sensation of incomplete evacuation [45 (47.4 %) vs. 17 (26.2 %); P = 0.016]. The following parameters all showed tendency towards significant differences between patients not using opioids and controls: constipation [68.88 (45.00–100.00) vs. 84.47 (83.00–98.00); P = 0.051], psychological well-being [68.74 (50.00–100.00) vs. 82.07 (74.00–96.00); P = 0.064], and defecation urgency [29 (30.5 %) vs. 11 (16.9 %); P = 0.066].
The patients who currently received hormonal treatment for endometriosis (combined oral contraceptives, progesterone, estrogen, or GnRH analogs) ( n = 62) did not experience more severe gastrointestinal symptoms than the other patients ( n = 24) (data not shown). However, when comparing patients with current or previous GnRH treatment ( n = 55) towards the other patients ( n = 51), there was a higher degree of abdominal pain among the first group [55.35 (25.00–91.25) vs. 69.51 (50.00–100.00); P = 0.024]. Among those who had no hormonal treatment, the patients who were currently menstruating ( n = 3), were compared to those who did not menstruate ( n = 21), and no significant differences regarding symptoms between the groups were found (data not shown).
Prospective follow-up of gastrointestinal symptoms during treatment
Of the 14 patients initiating a new hormonal treatment for endometriosis, the only significant effect was improved psychological well-being from 0 to 3 months, followed by impaired well-being from 3 to 6 months (Friedman’s test; P = 0.006). When performing subgroup analyses, the patients who had initiated a new treatment with combined oral contraceptives ( n = 5) did not experience any significant reduction in any of the symptoms over time (data not shown). Subgroup analyses in patients who had initiated treatment with progesterone ( n = 6) showed a significant effect regarding psychological well-being, which had improved at the 3-month follow-up but was impaired at the 6-month follow-up (Friedman’s test; P = 0.016).
Compared to controls, endometriosis patients experience more abdominal pain, constipation, bloating and flatulence, influence of intestinal symptoms on daily life, defecation urgency, sensation of incomplete evacuation, and decreased psychological well-being. Localization of endometriosis lesions showed no association with symptoms, except lesions within or close to the bowel, which were associated with more nausea and vomiting. Patients using opioids had more severe symptoms than patients not using opioids, and patients treated with GnRH analogs had more abdominal pain than the other patients. A prospective analysis of patients initiating a new hormonal treatment of endometriosis during the study showed no impact from treatment of gastrointestinal symptoms over time. In contrast, prior studies have shown that progestins relief gastrointestinal symptoms related to the menstrual cycle, as well as overall diarrhea and intestinal cramping [ 18 ]. However, the latter study could not detect any effect of progestins on overall constipation, abdominal bloating and feeling of incomplete evacuation [ 18 ]. The difference between studies is that the present patients did not experience diarrhea. Thus, hormonal treatment may have its main effect on endometriosis and endometriosis-related symptoms, and less effect on overall gastrointestinal symptoms.
To the best of our knowledge, this is the first study that has investigated gastrointestinal symptoms among patients with endometriosis using a continuous scale, the VAS-IBS. Also, to the best of our knowledge, no study has investigated the symptoms in respect to use of opioids and GnRH analogs.
The findings of the present study partially support the findings of previous studies in regard to bloating, abdominal pain, and constipation among endometriosis patients [ 3 , 5 ]. However, in other studies, diarrhea, nausea, and vomiting were reported to be common [ 3 , 4 ]; however, these symptoms were not more frequent among patients than controls in the current study. Previous studies have reported exacerbation of symptoms during menstruation [ 4 , 6 , 7 ]. This phenomenon does not differentiate between endometriosis and IBS, since not only abdominal pain due to endometriosis, but also gastrointestinal symptoms due to functional bowel diseases have been shown to increase during menstruation [ 19 ]. Symptoms were not found to be more severe during menstruation in this study, which can depend on few menstruating ( n = 3) vs. non-menstruating ( n = 21) patients in the group of non-hormonal treatment, since some patients experienced menstruation as a trigger factor for gastrointestinal symptoms.
Symptoms including diarrhea, constipation, and colic rectal pain have been reported to be more common among patients with endometriosis lesions within or close to the bowel than among patients with distant lesions [ 7 , 9 ]. However, other studies have not found this association [ 3 ]. In the current study, nausea and vomiting were associated with bowel-related lesions, but no other symptom association was detected. These findings, and the fact that hormonal endometriosis treatment did not influence gastrointestinal symptoms over time, indicate an existing comorbidity between endometriosis and IBS.
One explanation for this possible comorbidity is an immunological link, involving increased mast cell activation. In IBS, colonic mast cell activation and mediator release close to mucosal innervation have been reported [ 20 ], and in deep infiltrating endometriosis, the presence of an increased number of activated mast cells close to nerves have been described [ 21 ]. Issa et al. [ 22 ] suggested that the visceral hypersensitivity found in both patients with IBS and endometriosis could amplify gastrointestinal symptoms in patients with endometriosis. A hormonal link is also plausible; GnRH-containing neurons [ 11 ] and receptors for LH [ 23 ] have been shown to be present in the human gastrointestinal tract as well as in the pelvic organs [ 24 , 25 ]. IBS is predominantly diagnosed in women, with a female to male ratio ranging from 2:1 to 4:1, depending on the diagnostic procedure [ 26 ]. Female sex hormones have been suggested to be involved in IBS-associated pain, since fluctuation in IBS symptoms has been reported with exacerbation of abdominal pain during menstruation [ 19 ]. However, the mechanisms underlying these findings are unclear [ 26 ]. Exacerbation of gastrointestinal symptoms in endometriosis patients during menstruation has also been reported [ 4 , 6 , 7 ]. Another explanation for the symptoms could be a yet undefined gastrointestinal disease or undiscovered endometriosis in the intestinal wall.
Use of opioids is known to cause gastrointestinal symptoms such as constipation, nausea, and abdominal pain, in severe cases referred to as narcotic bowel syndrome [ 27 ]. Almost 20 % of the patients had been prescribed opioids because of abdominal pain, and patients with current opioid use had more severe symptoms on almost all parameters measured by the VAS-IBS than patients not using opioids. One explanation to these findings is that the patients with severe symptoms were prescribed opioids, but another explanation is that opioids could cause or aggravate symptoms. A conclusion to be drawn is that many endometriosis patients may not benefit from opioid treatment. Perhaps, opioids have no or weak positive impact on gastrointestinal symptoms; they possibly may even exacerbate them. Thus, all initiating of opioid treatment in this patient group must be carefully evaluated before continued. When excluding current opioid-users, the endometriosis patients still had more severe symptoms than controls, even though the P values were slightly higher than 0.05 in some parameters.
GnRH has been shown to be present in the ENS [ 11 ] and has been linked to gastrointestinal function [ 12 , 13 ], but its role in gut physiology and pathophysiology has not been completely elucidated. Hammar et al. [ 13 ] reported increased symptoms of constipation, as well as nausea and vomiting among women after treatment with GnRH analogs, with exacerbation of abdominal pain showing a tendency towards significance. At 5-year follow-up, the patients had more abdominal pain than they experienced prior to GnRH treatment [ 13 ], and some patients have developed severe dysmotility secondary to repeated or prolonged GnRH treatment [ 11 , 14 , 15 ]. In the present study, patients treated with GnRH analogs had more abdominal pain than the other patients. This could have several explanations; one is that patients with more severe symptoms received GnRH treatment, but another plausible explanation is that the symptoms are due to side effects evoked by GnRH on the ENS. Further research on GnRH and its role in gastrointestinal function and dysfunction is needed.
The current study has several limitations. Approximately half of the patients identified as fulfilling inclusion criteria declined to participate. One can hypothesize that the patients who agreed to participate experienced more severe symptoms, making them more prone to report them. Another weakness is that the patient group and control group were not matched regarding age. To minimize the impact of this factor, z-scores were calculated and analyzed. However, age only correlated with symptoms in patients and not in controls, and the patients who declined to participate were slightly younger, which correlated with more severe symptoms. The patients reported pharmacological treatment of endometriosis and gastrointestinal symptoms, and as the majority of patients most likely had no medical education, one can assume that they less accurately reported their symptoms. To minimize inaccuracy, the pharmacological treatment was discussed at the interview. When asked to measure abdominal pain on the VAS-IBS, it is not clear whether patients responded regarding pain related to endometriosis or gastrointestinal symptoms. However, almost half of the patients reported having the ability to differentiate pain from endometriosis from that of the gastrointestinal tract. The patients appear to be a selected group with high education and a healthy lifestyle; they reported low consumption of alcohol and tobacco. However, these habits could also be due to the fact that alcohol and smoking exacerbate their symptoms.
This study has several clinical impacts. Endometriosis is a disease with a considerable diagnostic delay [ 28 ], and an extended knowledge of symptoms associated with the disease could potentially contribute to reducing this delay. It is also of importance to acknowledge these symptoms in order to provide adequate pharmacological treatment, especially since hormonal treatment of endometriosis appeared to have no effect on gastrointestinal symptoms. The findings also indicate the importance of conservativeness in prescribing opioids to this group of patients, especially if the indication is gastrointestinal symptoms, because opioids appear to have no or weak effect on these symptoms. Physicians must carefully evaluate the effect of opioids and should withdraw opioid treatment when the effect is uncertain.
A large proportion of patients with endometriosis suffer from gastrointestinal symptoms. Compared to controls, patients with endometriosis suffer from more severe abdominal pain, constipation, bloating and flatulence, impaired psychological well-being, influence of symptoms on daily life, defecation urgency, and sensation of incomplete evacuation. The location of the endometriosis lesions is not associated with symptoms, except increased nausea and vomiting among patients with lesions within or close to the bowel. Patients treated with opioids have more severe symptoms than patients not treated with opioids, and current or previous treatment with GnRH analogs is associated with increased abdominal pain. Initiating a new hormonal treatment of endometriosis has no impact on gastrointestinal symptoms over time.

Abbreviations
Chronic intestinal pseudo-obstruction
- Gonadotropin-releasing hormone
In vitro fertilization
Luteinizing hormone
Visual analogue scale for irritable bowel syndrome
Giudice LC, Kao LC. Endometriosis Lancet. 2004;364(9447):1789–99.
Article PubMed Google Scholar
Ozkan S, Arici A. Advances in treatment options of endometriosis. Gynecol Obstet Invest. 2009;67(2):81–91.
Article CAS PubMed Google Scholar
Maroun P, Cooper MJ, Reid GD, Keirse MJ. Relevance of gastrointestinal symptoms in endometriosis. Aust N Z J Obstet Gynaecol. 2009;49(4):411–4.
Luscombe GM, Markham R, Judio M, Grigoriu A, Fraser IS. Abdominal bloating: an under-recognized endometriosis symptom. J Obstet Gynaecol Can. 2009;31(12):1159–71.
Ballweg ML. Impact of endometriosis on women’s health: comparative historical data show that the earlier the onset, the more severe the disease. Best Pract Res Clin Obstet Gynaecol. 2004;18(2):201–18.
Meurs-Szojda MM, Mijatovic V, Felt-Bersma RJ, Hompes PG. Irritable bowel syndrome and chronic constipation in patients with endometriosis. Colorectal Dis. 2011;13(1):67–71.
Fauconnier A, Chapron C, Dubuisson JB, Vieira M, Dousset B, Breart G. Relation between pain symptoms and the anatomic location of deep infiltrating endometriosis. Fertil Steril. 2002;78(4):719–26.
Seaman HE, Ballard KD, Wright JT, de Vries CS. Endometriosis and its coexistence with irritable bowel syndrome and pelvic inflammatory disease: findings from a national case-control study-Part 2. BJOG. 2008;115(11):1392–6.
Roman H, Ness J, Suciu N, Bridoux V, Gourcerol G, Leroi AM, et al. Are digestive symptoms in women presenting with pelvic endometriosis specific to lesion localizations? A preliminary prospective study. Hum Reprod. 2012;27(12):3440–9.
Conn PM, Crowley Jr WF. Gonadotropin-releasing hormone and its analogs. Annu Rev Med. 1994;45:391–405.
Hammar O, Ohlsson B, Veress B, Alm R, Fredrikson GN, Montgomery A. Depletion of enteric gonadotropin-releasing hormone is found in a few patients suffering from severe gastrointestinal dysmotility. Scand J Gastroenterol. 2012;47(10):1165–73.
Mathias JR, Clench MH, Abell TL, Koch KL, Lehman G, Robinson M, et al. Effect of leuprolide acetate in treatment of abdominal pain and nausea in premenopausal women with functional bowel disease: a double-blind, placebo-controlled, randomized study. Dig Dis Sci. 1998;43(6):1347–55.
Hammar O, Roth B, Bengtsson M, Mandl T, Ohlsson B. Autoantibodies and gastrointestinal symptoms in infertile women in relation to in vitro fertilization. BMC Pregnancy Childbirth. 2013;13:201.
Article PubMed PubMed Central Google Scholar
Cordeddu L, Bergvall M, Sand E, Roth B, Papadaki E, Li L, et al. Severe gastrointestinal dysmotility developed after treatment with gonadotropin-releasing hormone analogs. Scand J Gastroenterol. 2015;50(3):291–9.
Ohlsson B, Veress B, Janciauskiene S, Montgomery A, Haglund M, Wallmark A. Chronic intestinal pseudo-obstruction due to buserelin-induced formation of anti-GnRH antibodies. Gastroenterology. 2007;132(1):45–51.
Bengtsson M, Ohlsson B, Ulander K. Development and psychometric testing of the Visual Analogue Scale for Irritable Bowel Syndrome (VAS-IBS). BMC Gastroenterol. 2007;7:16.
Bengtsson M, Persson J, Sjolund K, Ohlsson B. Further validation of the visual analogue scale for irritable bowel syndrome after use in clinical practice. Gastroenterol Nurs. 2013;36(3):188–98.
Ferrero S, Camerini G, Ragni N, Venturini PL, Biscaldi E, Remorgida V. Norethisterone acetate in the treatment of colorectal endometriosis: a pilot study. Hum Reprod. 2010;25(1):94–100.
Moore J, Barlow D, Jewell D, Kennedy S. Do gastrointestinal symptoms vary with the menstrual cycle? Br J Obstet Gynaecol. 1998;105(12):1322–5.
Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126(3):693–702.
Anaf V, Chapron C, El Nakadi I, De Moor V, Simonart T, Noel JC. Pain, mast cells, and nerves in peritoneal, ovarian, and deep infiltrating endometriosis. Fertil Steril. 2006;86(5):1336–43.
Issa B, Onon TS, Agrawal A, Shekhar C, Morris J, Hamdy S, et al. Visceral hypersensitivity in endometriosis: a new target for treatment? Gut. 2012;61(3):367–72.
Sand E, Bergvall M, Ekblad E, D’Amato M, Ohlsson B. Expression and distribution of GnRH, LH, and FSH and their receptors in gastrointestinal tract of man and rat. Regul Pept. 2013;187:24–8.
Rispoli LA, Nett TM. Pituitary gonadotropin-releasing hormone (GnRH) receptor: structure, distribution and regulation of expression. Anim Reprod Sci. 2005;88(1–2):57–74.
Yung Y, Aviel-Ronen S, Maman E, Rubinstein N, Avivi C, Orvieto R, et al. Localization of luteinizing hormone receptor protein in the human ovary. Mol Hum Reprod. 2014;20(9):844–9.
Meleine M, Matricon J. Gender-related differences in irritable bowel syndrome: potential mechanisms of sex hormones. World J Gastroenterol. 2014;20(22):6725–43.
Azizi Z, Javid Anbardan S, Ebrahimi DN. A review of the clinical manifestations, pathophysiology and management of opioid bowel dysfunction and narcotic bowel syndrome. Middle East J Dig Dis. 2014;6(1):5–12.
PubMed PubMed Central Google Scholar
Husby GK, Haugen RS, Moen MH. Diagnostic delay in women with pain and endometriosis. Acta Obstet Gynecol Scand. 2003;82(7):649–53.
Download references
Acknowledgements
This study was sponsored by grants from King Gustaf V and Queen Victoria Free Maison’s Foundation, the Bengt Ihre Foundation, the Development Foundation from Region Skåne, and the Foundation of Skåne University Hospital.
Author information
Authors and affiliations.
Department of Clinical Sciences, Division of Internal Medicine, Skåne University Hospital, Lund University, 205 02,, Malmö, Sweden
Malin Ek, Bodil Roth & Bodil Ohlsson
Department of Clinical Sciences, Division of Gynecology, Skåne University Hospital, Lund University, 205 02, Malmö, Sweden
Per Ekström & Lil Valentin
Faculty of Health and Society, Institution of Care Science, Malmö University, Malmö, Sweden
Mariette Bengtsson
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Malin Ek .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
BO, MB, PE, and LV designed and planned the study. BR enrolled the patients and collected blood samples. ME performed the statistical calculations and wrote the manuscript. BO financed the study. All authors contributed to revision and finalization of the manuscript as well as approval of the final version.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Ek, M., Roth, B., Ekström, P. et al. Gastrointestinal symptoms among endometriosis patients—A case-cohort study. BMC Women's Health 15 , 59 (2015). https://doi.org/10.1186/s12905-015-0213-2
Download citation
Received : 01 April 2015
Accepted : 22 July 2015
Published : 13 August 2015
DOI : https://doi.org/10.1186/s12905-015-0213-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Abdominal pain
- Endometriosis
- Gastrointestinal symptoms
- Menstruation
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Robinson Research Institute
Case study: Revolutionising the diagnosis of endometriosis

In Australia, at least one in nine women, or those assigned female at birth, live with often debilitating symptoms caused by endometriosis. Endometriosis occurs when tissue similar to the lining of the uterus grows elsewhere in the body.
The cause of patients’ symptoms is often unknown to them for too long – the average timeframe for an endometriosis diagnosis in Australia is 6.4 years. Undiagnosed suffering not only comes with the physical symptoms of the condition such as strong period pain and heavy bleeding, bowel and bladder issues or infertility, it also takes a toll on the mental health and social life of those affected.
On track to provide non-invasive, fast and cost-effective diagnosis
The current ‘gold standard’ for diagnosis of endometriosis is invasive abdominal surgery by direct visualisation of lesions, which has long wait times, high costs and the requirement for multidisciplinary, highly skilled surgical teams.
The IMAGENDO® team in the Endometriosis research group led by Professor Louise Hull, is well on track to revolutionise how endometriosis is diagnosed. Funded by an MRFF Primary Health Care Research Data Infrastructure Grant, an interdisciplinary team of endometriosis researchers from Robinson Research Institute, artificial intelligence experts from the University of Adelaide’s Australian Institute for Machine Learning, and specialist gynaecological and obstetrics imaging partners locally and around the globe, are working on technology that is set to improve the lives of many.
IMAGENDO® is an automated and guided diagnostic system for the identification of specific endometriosis features that can be visualised in transvaginal ultrasound (TVUS) and magnetic resonance imaging (MRI) scans. An artificial intelligence algorithm that has been developed and trained by hundreds of images, locates and consolidates a specific set of endometriosis features and yields scores for the probability of a diagnosis of endometriosis and, if present, the likely severity.
"We currently see a 90% accuracy rate of the technology in being able to distinguish positive from negative cases. If the development continues as we expect, we hope to see the technology rolled out worldwide with an aim of having it available in clinics within the next two to five years." Dr Jodie Avery, IMAGENDO Program Manager
Set to improve the lives of many
IMAGENDO® was awarded the prestigious 2023 ANSTO Eureka Prize for Innovative Use of Technology and if the new technology delivers on the promise, the benefits to patients and the public will be many. The rapid and cost-efficient diagnosis option will enable individualised care plans to be established much sooner, without years of waiting. The need for invasive abdominal surgery will be reduced, and unnecessary surgery and some cases of repeated surgery will be avoided. Further, there is potential to safeguard the fertility of young patients with earlier diagnosis providing them the opportunity to freeze their eggs at a younger age. The technology will also help in training and up-skilling sonographers and act as an imaging data repository.
To pave the way for a clinical roll-out, the algorithm undergoes constant iterations to include more markers of endometriosis and expand to cover adolescents and young women. International collaborations are being expanded to further refine the technology and prepare for an international roll-out.
- Previous page
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

Endometriosis Patient Case Study
Created by haerim kwon, mercedes pratt, elisha williams, and jessica witkin, pathophysiology of altered health states, autumn 2019, dr. amy mackos, dr. kelly casler, and dr. lee cordell.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.6(1); 2013 Mar 15
Case study of a rare form of endometriosis
* Obstetrics and Gynecology Department, Bucharest University Hospital
** Orthopedics and Traumatology Department, Bucharest University Hospital
Endometriosis is a common, benign, chronic, estrogen-dependent disorder. The endometrial tissue implants itself outside the uterus and can be usually found in the pelvis or, in rare cases, it can be found nearly anywhere in the body. There are no pathognomonic symptoms of this disease, therefore, in some cases the tumors are incidentally discovered during surgery. Deep infiltrative endometriosis (DIE) is a rare form of this condition, which mostly affects the uterosacral ligaments, the rectovaginal space, and the upper third of the posterior vaginal wall, the bowel, and the urinary tract.
We present the case of a 29-year-old pregnant female who was diagnosed with infiltrative endometriosis during the cesarean section at 38 weeks of gestation. The tumors involving the vesicouterine peritoneum had a tendency of infiltrating the urinary bladder, but the patient had been completely asymptomatic prior to this incidental discovery. As cited by literature, the discovery and management of urinary endometriosis, as well as that of other localizations of DIE, is not based on high-level evidence data, but rather on case-series reported by surgical teams working in different centers worldwide.
Introduction
Endometriosis is defined as the presence of endometrial glands and stroma outside the uterus. These ectopic endometrial implants are usually located in the pelvis, but can occur almost anywhere in the body. Endometriosis is a benign, chronic, estrogen-dependent disorder. It can be associated with many distressing and debilitating symptoms, such as pelvic pain, severe dysmenorrhea, dyspareunia and infertility, or it may be asymptomatic and incidentally discovered at laparoscopy or exploratory surgery [ 1 ]. Three types of endometriosis have been described: peritoneal superficial endometriosis, ovarian endometriomas, and deep infiltrating endometriosis (DIE). The latter usually involves the uterosacral ligaments, the rectovaginal space, the upper third of the posterior vaginal wall, the bowel, and the urinary tract [ 2 ]. Urinary tract DIE may be found in up to 6% of women presenting with pelvic endometriosis and may involve either the bladder or ureters. The management of urinary endometriosis, as well as that of other localizations of DIE, is not based on high-level evidence data, but rather on case-series reported by surgical teams working in different centers around the world [ 3 ].
Case report
A 29-year-old pregnant female was admitted accusing contractions. She was gravida 3, para 1, with a 38 weeks developing pregnancy.
From her medical history during pregnancy, result the following diagnostics: placenta praevia marginalis, antiphospholipid syndrome, autoimmune thyroiditis, vitiligo, inherited trombophilia, urinary tract infections with Proteus mirabilis and Klebsiella pneumoniae, a history of GBS colpitis (Group B Streptococcus) and a pregnancy excess weight gain of +20 kg.
Two years prior to pregnancy, the patient underwent a cervical electro-resection with the diathermal loop (ERAD) for L-SIL (low-grade squamous intraepithelial lesion of the cervix). Her personal female history includes menarche at 12 years old, regular menstrual periods, with several episodes of menstrual pain and occasional constipation. In the past three years, the patient accused cycle-dependent pain in the upper left shoulder and in the right hypochondrium. The severe pain occurred in the 2nd day of menstrual cycle and often leads to syncopal episodes. She also had two abortions for undesired pregnancies.
During the current pregnancy, she had made regular visits to her doctor and had made usual investigations: blood and urine tests, vaginal and abdominal ultrasound, fetal monitoring, all according to gestational stages of development. Her colpitis and urinary tract infections have been treated with antibiotics according to antibiogram results. She also received 0.4 ml of enoxaparine, one daily injection, for her inherited trombophilia and high triglycerides blood levels.
In her 38th week of gestation, she was admitted to hospital accusing contractions and vaginal bleeding. As being formerly diagnosed with placenta praevia, antiphospholipid syndrome and more autoimmune disorders, the patient was subjected to cesarean section delivery.
At the opening of the peritoneal cavity, we discovered 50-60 ml of blood and several bluish tumors, with vegetant and infiltrative aspect, adherent to the vesicouterine peritoneum. Some tumors were actively bleeding, having wide or narrow sites of implantation and dimensions of 5-6 cm. The operator performed viscerolysis of a part of the tumors ( Fig. 1 - -3 3 ).

Vegetant bleeding tumors on the uterus and vesicouterine peritoneum

Tumor with large base of implantation, infiltrating the serous layer of the urinary bladder

Tumor infiltrating the vesicouterine peritoneum
One tumor had a larger implantation base and appeared to infiltrate the serous coat of the urinary bladder. Excision of this tumor was performed and the coat of the bladder was sutured at the site of excision. All tumor fragments were sent to extemporaneous examination.
Hysterotomy incision was carefully performed among the tumoral formations. The baby was extracted in cephalic presentation with no difficulty. It weighted 3250 grams and received APGAR 9. The placenta (praevia marginalis type) was extracted with difficulty as being adherent to the posterior wall of the lower uterine segment. Hemostasis was laborious in the placental bed.
The result of the extemporaneous exam stated: “Hyperplasia of endometrial stroma with decidualized endometrium. Decidualized endometriosis".
After the suture of the uterus was done, the team decided the excision of the rest of the tumors, which had a narrow implantation base. All tissue fragments were sent to histopathology examination along with the placenta. Hemostasis was laborious at the sites of excision and the closing of the vesicouterine peritoneum was difficult due to the tumors infiltrating into the serous coat of the urinary bladder. The further steps of the closing of the abdominal wall were normally performed, with careful but efficient hemostasis.
The evolution of the patient`s recovery in the first 48 hours after surgery was marked by a slow return of the bowel function with important abdominal meteorism. The intestinal transit was re-established with proper medication and the patient was discharged from hospital 5 days after surgery in good health conditions.
Further, the patient had recovered well, stopped breastfeeding and was put under hormonal treatment with GnRH agonist Triptorelin (one intramuscular injection every 4 weeks for 6 months) under regular surveillance.
Endometriosis is primarily found in the pelvis: on the ovaries, uterus, fallopian tubes, uterosacral ligaments, broad ligaments, round ligaments, cul-de-sac or ovarian fossa, as well as on the appendix, large bowel, ureters, bladder, or rectovaginal septum. In the case reported, we were concerned of possible endometriosis expansion into the base of the broad ligaments that can affect the normal trajectory of ureters or even intrinsic invasion cited by some authors [ 11 ]. Extra-pelvic locations of endometriosis are rare, but can include the upper abdomen, diaphragm, abdominal wall or abdominal scar tissue.
Deep endometriosis is defined as a solid mass situated deeper than 5 mm under the peritoneum [ 4 ] and is typically characterized by multifocal locations. According to the theory of retrograde menstruation, deep endometriosis is the result of cells implanting in the most dependent areas of the pelvis, such as the spaces anterior and posterior to the uterus. These spaces serve as anatomic shelters that contain endometrial cells and prevent them from being cleared by the usual processes within the peritoneal cavity. The presence of endometrial cells elicits an inflammatory response.
Endometriosis tissue is biologically the same as basal endometrial tissue. Foci of endometriosis consist of glands, stroma cells, and smooth muscle; they are supplied by nerves, lymphatic vessels, and blood vessels [5,6]. Endometriosis cells express estrogen receptors (ER α/β) and progesterone receptors (PR A/B) and therefore respond to endocrine treatment [ 4 - 7 ].
The estimated prevalence of endometriosis is 5% to 15% among all women of reproductive age. Prevalence is difficult to determine because symptoms are diverse and nonspecific and because some women are asymptomatic.
The main manifestations are primary or secondary dysmenorrhea, bleeding disturbances, infertility, dysuria, pain on defecation (dyschezia), cycle-dependent or cycle-independent pelvic pain, nonspecific cycle-associated gastrointestinal or urogenital symptoms, constipation, diarrhea, or hematochezia, fibromyalgia and migraines. Often, no abnormalities are found and none of these symptoms is pathognomonic [ 10 ].
No strong data are available concerning the prevalence of deep infiltrating intestinal endometriosis, or of endometriosis of the urinary tract. The overall prevalence of urogenital endometriosis is thought to be of 1% to 2% of the overall prevalence of endometriosis [ 8 - 9 ].
Deep pelvic endometriosis usually involves the urinary system, with the bladder being affected in 85% of cases. Currently, the treatment is usually surgical, consisting of either transurethral resection or partial cystectomy, and eventually associated with hormonal therapy. The hormonal therapy alone counteracts only the stimulus of endometriotic tissue proliferation, with no effects on the scarring caused by this tissue. The overall recurrence rate is about 30% for combined therapies and about 35% for the hormonal treatment alone [ 3 ].
Conclusions
In the present case, deep infiltrative endometriosis was incidentally found during the cesarean section in a patient with no previous clear symptoms, which adds this case to the small number of similar cases described by literature.
The management of urinary endometriosis as well as that of other localizations of deep infiltrative endometriosis is not based on high-level evidence data, but rather on case-series reported by surgical teams working in different centers.
Despite numerous studies, considerable controversy remains regarding the incidence, pathogenesis, natural history, and optimal treatment of this disorder.
Deep infiltrating endometriosis and endometriosis of the urinary tract could cause long-term complications, which involve high treatment costs.
Endometriosis may quadruple risk of ovarian cancer, study finds
Women with severe endometriosis are 10 times more likely to get ovarian cancer, while people with endometriosis of any severity are four times as likely, a study suggests. But patients shouldn't panic.

Women with endometriosis may have a substantially increased risk of ovarian cancer, new research suggests.
In the study, women with endometriosis were more than four times as likely to get ovarian cancer than those who did not have the disease. For women with severe endometriosis, the risk of cancer jumped nearly tenfold.
However, experts cautioned that this still represents a relatively small increase in risk, overall, and that patients with endometriosis shouldn't be unduly concerned.
The study, published July 17 in the journal JAMA , included nearly 78,900 U.S. women with endometriosis . The disease, which affects approximately 10% of reproductive-age women , occurs when tissue similar to the lining of the uterus starts growing outside the organ, triggering inflammation and scarring.
Related: Why is endometriosis so hard to diagnose?
There are different types of endometriosis, which vary depending on whether the wayward tissue grows on the membrane that covers organs in the pelvis, in the ovaries, or on and between other organs in the pelvic and abdominal regions. These types vary in their severity, but in general, endometriosis is strongly associated with pelvic pain, infertility, irritable bowel syndrome, and breast, endometrial and ovarian cancers .
Previously, a study from Finland reported that women with endometriosis had double the chance of getting ovarian cancer and 10 times the risk if they had the form of the disease that affects the ovaries, compared with those without the condition. However, that study lacked enough samples to conduct a detailed analysis of the risks tied to each type of endometriosis.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The new JAMA study fills that gap.
"I am passionate about giving women quantitative information that can help them in shared decision making with their primary care providers or gynecological care providers," study co-author Karen Schliep , a reproductive and perinatal epidemiologist at the University of Utah, told Live Science.
At this point, the study doesn't point to any changes in who should get diagnostic or preventive surgeries for ovarian cancer, Schliep stressed. However, "my hope is that, working with other researchers and particularly cancer experts, we can look at development of prediction models that can be used by clinicians and their patients for helping to make some of these tough decisions," she said.
For the study, Schliep and her colleagues pulled information on women ages 18 to 55 from the Utah Population Database . The final cohort included 78,893 women with a history of endometriosis and about 379,000 women without known endometriosis. Within those groups, it included nearly 600 women with ovarian cancer.
The authors split endometriosis into five categories, depending on which organs it affected, and they split the ovarian cancers into two types, based on whether they grew locally or more aggressively.

This large dataset revealed that the women with any type of endometriosis had a 4.2-times-higher lifetime risk of developing ovarian cancer, compared with women without the condition. In this overall group, the boost in risk was higher for local cancers than for aggressive cancers.
For those whose condition affected only the pelvic organs, the cancer risk was 19 times higher than baseline. Those confirmed to have endometriosis on both their pelvic organs and ovaries simultaneously had a 13-times-higher risk. Again, the risk of local cancers was higher than that of aggressive cancers, although both risks were elevated.
Related: New blood test detects ovarian cancer years before conventional methods
"It is of interest to determine — and we don't have a way of doing this right now — which are those few people that have endometriosis and are at higher risk of ovarian cancer," said Dr. Paul Yong , a gynecologist and researcher at the BC Women's Centre for Pelvic Pain & Endometriosis who was not involved in the study. "And then how do you identify them ahead of time? How do you prevent it?"
The size of the study is a strength, but it does have limitations. It's possible that some cases of endometriosis and ovarian cancer may be misclassified as the wrong subtypes, and there was also a lack of data on the use of hormonal contraceptives, some of which are known to reduce the risk of ovarian cancer .
"At the moment, at least on the data that's been presented, the message shouldn't be that there's this hugely increased ovarian cancer risk amongst women with endometriosis, because we simply do not have the evidence that that's the case," said Krina Zondervan , a reproductive and genomic epidemiologist at the University of Oxford who was not involved in the study.
Zondervan emphasized that women with endometriosis should not be unduly concerned and jump to having their ovaries removed. This brings on premature menopause that can raise the risk of other conditions, such as cardiovascular disease and osteoporosis, she noted.
— Endometriosis and gut disorders have a genetic link
— Black patients may be missed on common cancer screening, study suggests
— Endometriosis may be caused by a common gut bacteria, small study suggests
Data suggest that very few women with endometriosis get ovarian cancer — the lifetime risk of ovarian cancer for women without endometriosis is 1.3%, and prior to this study, the reported risk for women with endometriosis was 1.8%. The new analysis raises this risk by only 0.1% — or about 10 extra cases per 10,000 people with any type of endometriosis. That still puts the overall risk much lower than the general population's risk of developing breast (13%) , lung (6%) or bowel (4%) cancer.
Nonetheless, "if a patient comes with concern about risk of ovarian cancer, I think they should be validated," Yong said. "The clinician should talk about it with the patient and not ignore it."
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun ? Send us your questions about how the human body works to [email protected] with the subject line "Health Desk Q," and you may see your question answered on the website!
Sahana Sitaraman is a science writer based in Lausanne, Switzerland, specializing in biology. She particularly enjoys writing about unusual animal behaviours and the neuroscience behind them, mental health and women in STEM. She also dabbles in illustrating cool findings that pique her interest. In her free time, Sahana can be found out on a hike, acting it up with the local improv group or painting. She holds a bachelor's degree in microbiology from the University of Delhi, India and a master's and PhD in life sciences from the National Centre for Biological Sciences in Bangalore, India.
More babies are being born with syphilis, study finds
Experimental menstrual product turns blood to jelly
Scientists drill longest-ever piece of Earth's mantle from underwater mountain near 'Lost City'
Most Popular
- 2 James Webb Space Telescope spies strange shapes above Jupiter's Great Red Spot
- 3 NASA offers SpaceX $843 million to destroy the International Space Station
- 4 Newly discovered asteroid larger than the Great Pyramid of Giza will zoom between Earth and the moon on Saturday
- 5 China opens Chang'e 6 return capsule containing samples from moon's far side
- 2 2,000 years ago, a bridge in Switzerland collapsed on top of Celtic sacrifice victims, new study suggests
- 3 Self-healing 'living skin' can make robots more humanlike — and it looks just as creepy as you'd expect
- 4 Tasselled wobbegong: The master of disguise that can eat a shark almost as big as itself
- 5 This robot could leap higher than the Statue of Liberty — if we ever build it properly
- Olympics 2024
- ₹ 10 Lakh,1" data-value="Loan ₹ 10 Lakh">Loan ₹ 10 Lakh

- Entertainment
- Latest News
- India Vs Spain Live Score
- Olympics 2024 Live
- Bangladesh News Live
- India vs Sri Lanka
- The Interview
- Web Stories
- Mumbai News
- Bengaluru News
- Daily Digest

UPSC aspirants death: CBI reaches Rau's IAS coaching centre; accused move court for bail | Top updates
Cbi took over the investigation in the upsc aspirants death case in delhi, and reached old rajinder nagar as part of the probe..
The Central Bureau of Investigation (CBI) on Wednesday took over the investigation into the Delhi UPSC aspirants death case, where three students drowned inside the basement of an IAS coaching centre in Delhi's Old Rajinder Nagar. A team of CBI officials reached Rau's IAS Study Circle coaching centre on Wednesday evening as part of their probe in the case.
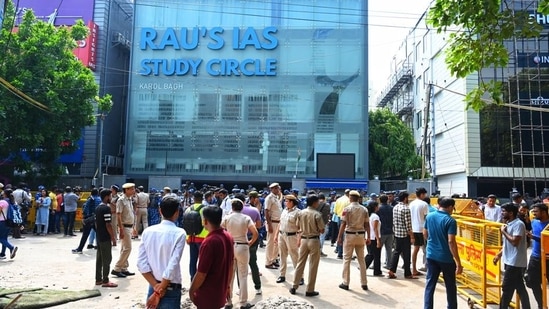
A senior CBI official informed that the agency has taken over the case by registering an FIR into the matter and all documents about the investigation have been handed over by Delhi Police to CBI. "After the initial formalities, the CBI team will soon be visiting the spot where the incident took place for a detailed investigation into the matter," the official said.
Read more: Delhi HC refuses to entertain Puja Khedkar’s appeal against UPSC action
The development comes after the Delhi high court last week transferred the investigation to the CBI, saying that it was unsatisfied with the probe conducted by the Delhi Police in the matter.
UPSC aspirants death: Top updates in case
- A team of CBI officials reached Old Rajinder Nagar on Wednesday evening. As part of their probe, the CBI team visited Rau's IAS Study Circle , where three students drowned in the basement.
- The co-owners of the coaching centre, who were arrested in the case, approached a special CBI court after seeking bail. Accused Harvinder, Tejinder, Parvinder and Sarabjeet have moved bail pleas through Advocates Kaushal Jeet Kait, Daksh Gupta, Jatin Gupta and others.
- After hearing the bail pleas of the accused, the Rouse Avenue Court in Delhi issued a notice to CBI, asking for a status report on the case amid the ongoing investigation.
- On August 5, the Supreme Court took suo motu cognisance on the issue related to safety norms in the coaching centres. A bench of justices, Surya Kant and Ujjal Bhuyan, observed that such institutes have become "death chambers" as the top court was hearing the petition filed by the Coaching Federation of India.
- The court further suggested that such institutes shall operate through online classes until they fully comply with the fire and safety norms under the Master Plan of Delhi, 2021, read with Unified Building Bye-Laws of Delhi, 2016.
(With inputs from PTI)
The Hindustan Times YouTube channel now has 7 million subscribers. We thank our viewers for their support. Follow the channel for exclusive video news on politics, sports, entertainment & more. Click here.
Get Current Updates on India News , Budget 2024 , Weather Today along with Latest News and Top Headlines from India and around the world.
- Terms of use
- Privacy policy
- Weather Today
- HT Newsletters
- Subscription
- Print Ad Rates
- Code of Ethics
- Live Cricket Score
- Cricket Teams
- Cricket Players
- ICC Rankings
- Cricket Schedule
- Shreyas Iyer
- Harshit Rana
- Kusal Mendis
- Ravi Bishnoi
- Rinku Singh
- Riyan Parag
- Washington Sundar
- Avishka Fernando
- Charith Asalanka
- Dasun Shanaka
- Khaleel Ahmed
- Pathum Nissanka
- Other Cities
- RBI MPC Meet 2024 Live
- Budget 2024 Live
- Income Tax LIVE Updates
- Income Tax Calculator
- Petrol Prices
- Diesel Prices
- Silver Rate
- Relationships
- Art and Culture
- Taylor Swift: A Primer
- Telugu Cinema
- Tamil Cinema
- Board Exams
- Exam Results
- Admission News
- Employment News
- Competitive Exams
- BBA Colleges
- Engineering Colleges
- Medical Colleges
- BCA Colleges
- Medical Exams
- Engineering Exams
- Love Horoscope
- Annual Horoscope
- Festival Calendar
- Compatibility Calculator
- Career Horoscope
- Manifestation
- The Economist Articles
- Lok Sabha States
- Lok Sabha Parties
- Lok Sabha Candidates
- Explainer Video
- On The Record
- Vikram Chandra Daily Wrap
- Entertainment Photos
- Lifestyle Photos
- News Photos
- Olympics Medal Tally
- Other Sports
- EPL 2023-24
- ISL 2023-24
- Asian Games 2023
- Public Health
- Economic Policy
- International Affairs
- Climate Change
- Gender Equality
- future tech
- HT Friday Finance
- Explore Hindustan Times
- Privacy Policy
- Terms of Use
- Subscription - Terms of Use

IMAGES
COMMENTS
Table 3 lists the symptoms and comorbidities that are associated with higher rates of endometriosis. 23 In a large case-control study in the United Kingdom, 73 percent of women with endometriosis ...
Patient Case Presentation. Chief Complaint: Infertility. Background: Ms. L.C. is a 34 year old female presenting with concerns of infertility. She has been attempting a pregnancy over the past 16 months with no success. Patient reports that several times she thought she could be pregnant due to a cessation in her menses with accompanying ...
Discussion Endometriosis that affects the gastrointestinal tract often presents with non-specific symptoms. This is a rare case of an acute small bowel obstruction as the index symptom of endometriosis in a peri-menopausal patient.
Endometriosis is a condition that affects women of reproductive age, and it is distinguished by the development of endometrial-like tissue outside the uterine cavity. It is frequently accompanied by persistent pelvic discomfort and infertility.
Patient Case Study. Mrs. M.D. is a 30 year old Caucasian female who was referred to the gynecology clinic by her PCP after complaining of pain in her pelvic area along with increased bleeding during her menstrual cycle. She states that she has experienced this pain for quite some time, but recently it seems to have been worsening with each cycle.
Endometriosis is an inflammatory chronic pain condition caused by uterine tissue growing outside of the uterus that afflicts at least 11% of women (and people assigned female at birth) worldwide. This condition results in a substantial burden to these ...
Pathophysiology. Endometriosis is a disorder characterized by the implantation of endometrial tissue in areas of the body outside of the uterus (Huether & McCance, 2019). The ectopic tissue is typically found in pelvic areas such as the ovaries and pelvic lining and within the abdominal cavity. This tissue is functional, so it proliferates and ...
Pelvic Pain - Endometriosis A 27 year old woman presented with severe dysmenorrhoea and pain with intercourse (dyspareunia). She also complained of bowel related pain during menstruation.
Background Women with endometriosis often experience gastrointestinal symptoms. Gonadotropin-releasing hormone (GnRH) analogs are used to treat endometriosis; however, some patients develop gastrointestinal dysmotility following this treatment. The aims of the present study were to investigate gastrointestinal symptoms among patients with endometriosis and to examine whether symptoms were ...
Endometriosis occurs when tissue similar to the lining of the uterus grows elsewhere in the body. The cause of patients' symptoms is often unknown to them for too long - the average timeframe for an endometriosis diagnosis in Australia is 6.4 years.
Endometriosis is the presence of endometrial gland tissues outside the uterine cavity. The most common sites are the pelvic peritoneum and pelvic organs. 1 Extra pelvic endometriosis is an uncommon entity and sites include the bowel, appendix, pleura and lung, abdominal wall, particularly the umbilicus and around surgical scars.
Harold Bruyere Buy Now About This Title Student Resources Instructor Resources Expand All Part 1: Cardiovascular Disorders Part 2: Respiratory Disorders Part 3: Gastrointestinal Disorders Part 4: Renal Disorders Part 5: Neurological Disorders Part 6: Psychiatric Disorders Part 7: Neuroendocrine Disorders Part 8: Chromosome Abnormality Disorders Part 9: Female Reproductive System Disorders Part ...
An Endometriosis Patient Presentation Enter Space Patient Case Study Pathophysiology Differential Diagnoses Review Questions Review Question Answers Patient Education Sources
Study with Quizlet and memorize flashcards containing terms like Case Study - Endometriosis, What is endometriosis?, Describe what is known about genetic or environmental contributions to endometriosis. and more.
Question: wCASE STUDY 310 65 ENDOMETRIOSIS For the Disease Summary for this case study, see the CD-ROM. PATIENT CASE Initial History P.N. is a 29-year-old white female who presents to her gynecologist complaining of severe lower abdominal cramps that were poorly responsive to OTC ibuprofen or acetaminophen. She has been married for nine years and has two sons, ages 6 wCASE STUDY 310 65 ...
Deep infiltrative endometriosis (DIE) is a rare form of this condition, which mostly affects the uterosacral ligaments, the rectovaginal space, and the upper third of the posterior vaginal wall, the bowel, and the urinary tract. We present the case of a 29-year-old pregnant female who was diagnosed with infiltrative endometriosis during the ...
Women with severe endometriosis are 10 times more likely to get ovarian cancer, while people with endometriosis of any severity are four times as likely, a study suggests. But patients shouldn't ...
A team of CBI officials reached Rau's IAS Study Circle coaching centre on Wednesday evening as part of their probe in the case. Security outside Rau's Study Circle following flooding that left ...